ACARIZAX Oral lyophilisate Ref.[50644] Active ingredients:
Source: Medicines & Healthcare Products Regulatory Agency (GB) Revision Year: 2021 Publisher: ALK-Abelló A/S, Bøge Alle 6-8, DK-2970 Hørsholm, Denmark
5.1. Pharmacodynamic properties
Pharmacotherapeutic group: Allergen extracts, house dust mite
ATC code: V01AA03
Mechanism of action
ACARIZAX is allergy immunotherapy. Allergy immunotherapy with allergen products is the repeated administration of allergens to allergic individuals with the purpose of modifying the immunological response to the allergen.
The immune system is the target for the pharmacodynamic effect of allergy immunotherapy, but the complete and exact mechanism of action regarding the clinical effect is not fully understood. Treatment with ACARIZAX has been demonstrated to induce an increase in house dust mite specific IgG4 and to induce a systemic antibody response that can compete with IgE in the binding of house dust mite allergens. This effect is observed already after 4 weeks of treatment.
ACARIZAX works by addressing the cause of house dust mite respiratory allergic disease, and clinical effect during treatment has been demonstrated for both upper and lower airways. The underlying protection provided by ACARIZAX leads to improvement in disease control and improved quality of life demonstrated through symptom relief, reduced need for other medications and a reduced risk for exacerbation.
Clinical efficacy in adults
The efficacy of treatment with ACARIZAX 12 SQ-HDM in house dust mite respiratory allergic disease was investigated in two double-blind, randomised, placebo-controlled trials with different endpoints and in different patient populations. Two thirds of the trial subjects were sensitised to more allergens than just house dust mite. Being sensitised to house dust mite only or to house dust mite and one or more other allergens did not impact the trial results. Supportive evidence from an allergen exposure chamber trial as well as a trial conducted with lower doses is also presented.
Allergic rhinitis
The MERIT trial (MT-06)
The MERIT trial included 992 adults with moderate-to-severe house dust mite allergic rhinitis despite the use of rhinitis pharmacotherapy. Subjects were randomised to approximately 1 year of daily treatment with 12 SQ-HDM, 6 SQ-HDM or placebo and were given free access to standardised rhinitis pharmacotherapy. Subjects were seen by a specialist approximately every two months during the entire trial.
The primary endpoint was the average daily total combined rhinitis score (TCRS) evaluated during the last 8 weeks of treatment. The TCRS was the sum of the rhinitis symptoms score and the rhinitis medication score. The rhinitis symptoms score evaluated 4 nasal symptoms (runny nose, blocked nose, itching nose, sneezing) daily on a 0-3 scale (no, mild, moderate, severe symptoms), i.e. range of scale is 0-12. The rhinitis medication score was the sum of the score for nasal steroid intake (2 points per puff, max. 4 puffs/day) and oral antihistamine intake (4 points/tablet, max. 1 tablet/day), i.e. range: 0-12. Thus the TCRS range is: 0-24.
Additional pre-defined key secondary endpoints were the total combined rhinoconjunctivitis score and rhinoconjunctivitis quality of life (RQLQ).
Post-hoc analyses of the days with a rhinitis exacerbation were also conducted to further illustrate the clinical relevance of the results. A rhinitis exacerbation was defined as a day where the subject returned to the high level of symptoms required for trial inclusion: a rhinitis symptom score of at least 6 or at least 5 with one symptom rated severe.
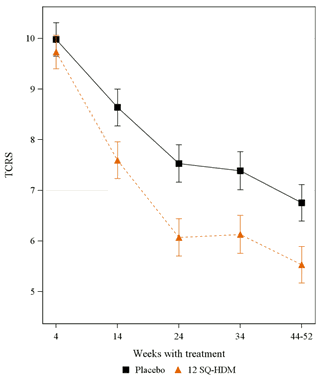
Figure. TCRS adjusted means over time:
(Error bars are ½ width of a 95% confidence interval for the difference in adjusted means)
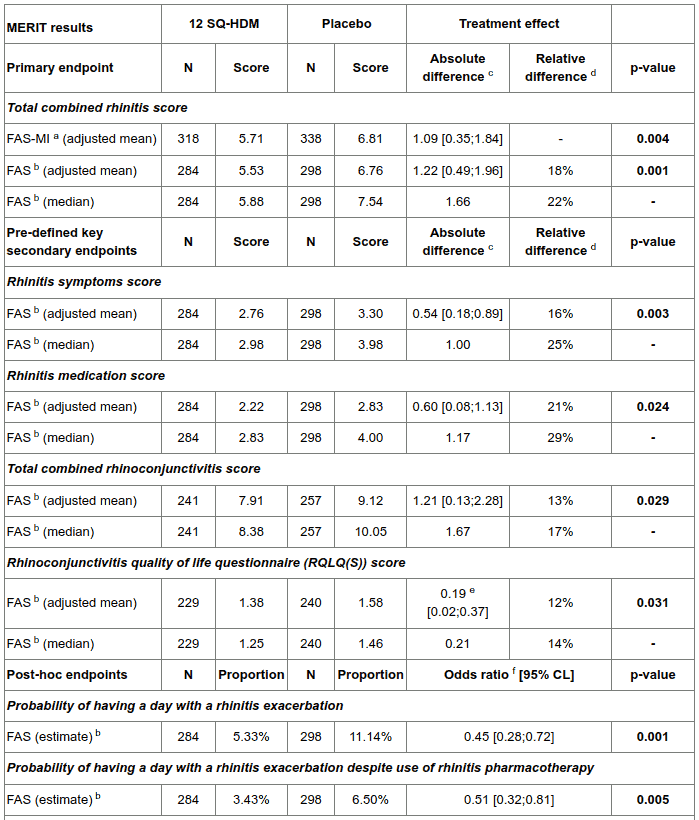
Table. Summary of main efficacy results in adults (allergic rhinitis):
N: number of subjects in treatment group with data available for the analysis.
CL: confidence limits
a FAS-MI: full analysis set with multiple imputations. The analysis treats subjects who discontinued the trial before the efficacy assessment period as placebo subjects. For the primary analysis (FAS-MI) only the absolute difference was pre-specified.
b FAS: full analysis set. All available data used to its full extent, i.e. subjects who provided data during the efficacy assessment period.
c Absolute difference: placebo minus 12 SQ-HDM, 95% confidence limits.
d Relative difference to placebo: placebo minus 12 SQ-HDM divided by placebo.
e The difference between 12 SQ-HDM and placebo was primarily driven by differences in three domains: sleep problems, practical problems and nose symptoms.
f Odds ratio for having a rhinitis exacerbation: 12 SQ-HDM over placebo.
Supportive evidence - allergic rhinitis
A randomised, double-blind, placebo-controlled phase II trial was conducted in an allergen exposure chamber in 124 adults with house dust mite allergic rhinitis. Before each allergen challenge, subjects were washed out of all allergy pharmacotherapy. At the end-of-trial allergen challenge after 24 weeks of treatment with 12 SQ-HDM, 6 SQ-HDM or placebo, the mean rhinitis symptoms score was 7.45 [6.57;8.33] in the placebo group and 3.83 [2.94;4.72] in the 12 SQ-HDM group, corresponding to an absolute difference of 3.62 and a relative difference of 49% (95% confidence interval [35%;60%], p<0.001). The difference between 12 SQ-HDM and placebo was also statistically significant at 16 weeks (mean scores of 4.82 and 6.90, difference of 2.08 corresponding to 30%, 95% CI [17%;42%], p<0.001) and at 8 weeks (mean scores of 5.34 and 6.71, difference of 1.37 corresponding to 20%, 95% CI [7%;33%], p=0.007).
Allergic asthma
The MITRA trial (MT-04)
The MITRA trial included 834 adults with house dust mite allergic asthma not well-controlled by daily use of inhaled corticosteroid (ICS) corresponding to 400-1200 µg budesonide. All subjects received 7-12 months' treatment with 12 SQ-HDM, 6 SQ-HDM or placebo in addition to ICS and short-acting beta-agonist prior to ICS reduction. No titration phase to establish the lowest maintenance dose of ICS was conducted prior to randomisation. Efficacy was assessed by time to first moderate or severe asthma exacerbation under ICS reduction over the last 6 months of 13-18 months of treatment.
- The definition of a moderate asthma exacerbation was fulfilled if the subject experienced one or more of the 4 criteria below, and it led to change in treatment:
- Nocturnal awakening or increase in symptoms: nocturnal awakening(s) due to asthma requiring short-acting β2 agonist (SABA) for two consecutive nights or increase of ≥0.75 from baseline in daily symptom score on two consecutive days.
- Increased SABA use: increase from baseline in occasions of SABA use on two consecutive days (minimum increase: 4 puffs/day).
- Deterioration in lung function: ≥20% decrease in PEF from baseline on at least two consecutive mornings/evenings or ≥20% decrease in FEV1 from baseline.
- Healthcare visit: visit to the emergency room/trial site for asthma treatment not requiring systemic corticosteroids.
- A severe asthma exacerbation was defined as experiencing at least one of the two following:
- Need for systemic corticosteroids for ≥3 days
- Emergency room visit requiring systemic corticosteroids or hospitalisation for ≥12h.
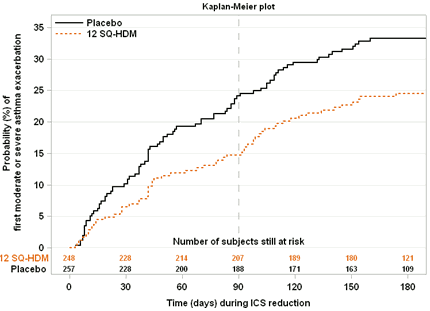
Figure. Risk of moderate/severe asthma exacerbation during ICS reduction/withdrawal phase:
Note: time 0 represents the time of the ICS reduction to 50%. At time 90, ICS was completely withdrawn for those subjects who had not exacerbated.
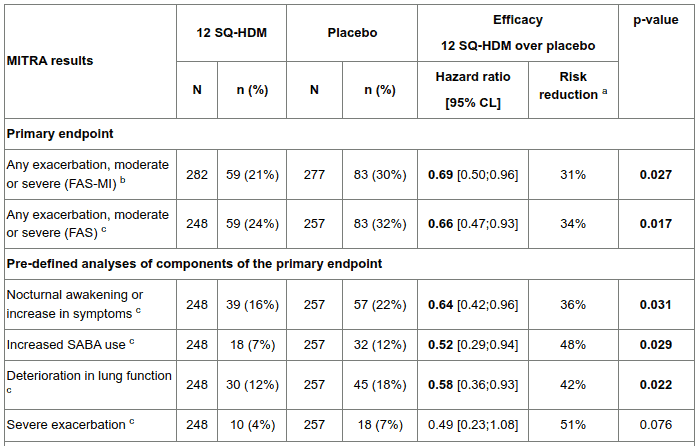
Table. Summary of main efficacy results in adults (allergic asthma):
N: number of subjects in treatment group with data available for the analysis.
n (%): number and percentage of subjects in treatment group meeting criterion.
CL: confidence limits
a Estimated by hazard ratio
b FAS-MI: full analysis set with multiple imputations. The analysis treats subjects who discontinued the trial before the efficacy assessment period as placebo subjects.
c FAS: full analysis set. All available data used to its full extent, i.e. including all subjects who provided data during the efficacy assessment period.
Post-hoc analyses of the asthma symptoms and symptomatic medication use in the last 4 weeks of the treatment period prior to reduction of inhaled corticosteroids were also conducted to investigate the effect of ACARIZAX as add-on to inhaled corticosteroid. The analyses looked at asthma daytime and nocturnal symptom scores, nocturnal awakenings, and SABA intake. The post-hoc analyses showed numerical differences consistently in favour of 12 SQ-HDM over placebo for all parameters investigated during the last 4 weeks prior to inhaled corticosteroid reduction. The differences were only statistically significant for the asthma daytime symptom score (p=0.0450) and the odds for no nocturnal awakenings (p=0.0409).
Supportive evidence - allergic asthma
In a double-blind, randomised, placebo-controlled phase II trial, 604 subjects ≥14 years old with house dust mite allergic asthma controlled by inhaled corticosteroids (100-800µg budesonide) and a clinical history of house dust mite allergic rhinitis were randomised to approximately 1 year of treatment with 1, 3 or 6 SQ-HDM or placebo. At the 4-week end-of-trial efficacy evaluation period, the mean change from baseline in the daily ICS dose was 207.6 µg budesonide in the 6 SQ-HDM group and 126.3 µg in the placebo group corresponding to an absolute difference of 81 µg budesonide per day (95% confidence interval [27;136], p= 0.004. Relative mean and median ICS reductions from baseline were 42% and 50% for 6 SQ-HDM and 15% and 25% for placebo. In a post-hoc analysis of a subgroup (N=108) of subjects with lower asthma control and ICS ≥400 µg budesonide, the mean change from baseline in the daily ICS dose was 384.4 µg budesonide in the 6 SQ-HDM group and 57.8 µg in the placebo group corresponding to an absolute difference between 6 SQ-HDM and placebo of 327 µg budesonide per day (95% CI [182;471], p<0.0001, post-hoc analysis).
Clinical efficacy in adolescents (12-17 years of age)
Allergic rhinitis
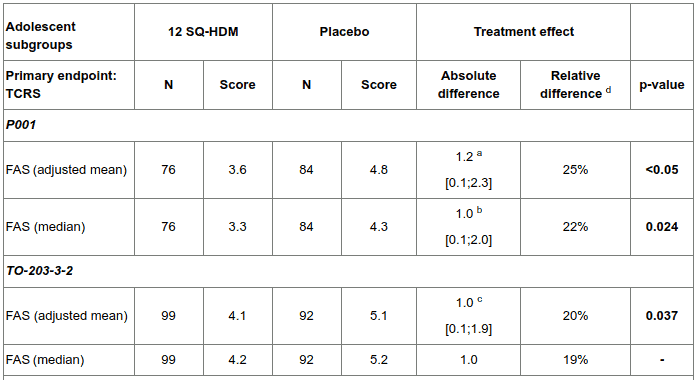
The efficacy of treatment with ACARIZAX 12 SQ-HDM in house dust mite allergic rhinitis in adolescents was investigated in two double-blind, randomised, placebo-controlled trials (P001 and TO-203-3-2). In these studies a proportion of the subjects were adolescents.
The P001 trial included 189 adolescents (of 1482 subjects randomised in total) with moderate-to-severe house dust mite allergic rhinitis/rhinoconjunctivitis with or without asthma. Subjects were randomised to approximately 1 year of daily treatment with 12 SQ-HDM or placebo and were given free access to standardised rhinitis pharmacotherapy.
The primary endpoint was the average daily total combined rhinitis score (TCRS) evaluated during the last 8 weeks of treatment.
After 1 year of treatment with 12 SQ-HDM, an absolute difference in medians of 1.0 (95% confidence interval [0.1; 2.0]) and a relative difference of 22% (p=0.024) compared to placebo was found in the adolescent group.
The TO-203-3-2 trial included 278 adolescents (of 851 subjects randomised in total) with moderate-to-severe persistent house dust mite allergic rhinitis. Subjects were randomised to approximately 1 year of daily treatment with 12 SQ-HDM, 6 SQ-HDM, or placebo and were given free access to standardised rhinitis pharmacotherapy.
The primary endpoint was the average daily TCRS evaluated during the last 8 weeks of treatment.
At the end-of-trial after 1 year of treatment with 12 SQ-HDM, an absolute difference in means of 1.0 (95% confidence interval [0.1; 1.9], p=0.037) and a relative difference of 20% compared to placebo was found in the adolescent group.
Table. Summary of main efficacy results in adolescents (allergic rhinitis):
TCRS: total combined rhinitis score
a: ANCOVA
b: Hodges-Lehmann estimate with 95% confidence intervals (primary analysis in the P001 trial)
c: Linear mixed-effects model (primary analysis in the TO-203-3-2 trial)
d: Relative differencto placebo: placebo minus 12 SQ-HDM divided by placebo
Other paediatric population
The licensing authority has waived the obligation to submit the results of studies with ACARIZAX in children under the age of 5 in house dust mite respiratory allergy (treatment of allergic rhinitis, treatment of asthma).
Long-term treatment
International treatment guidelines refer to a treatment period of 3 years for allergy immunotherapy to achieve disease modification. Efficacy data is available for 18 months of treatment with ACARIZAX from the MITRA trial. Long-term efficacy has not been established.
5.2. Pharmacokinetic properties
No clinical studies investigating the pharmacokinetic profile and metabolism of ACARIZAX have been conducted. The effect of allergy immunotherapy is mediated through immunological mechanisms, and there is limited information available on the pharmacokinetic properties.
The active molecules of an allergen extract are composed primarily of proteins. For sublingually administered allergy immunotherapy products, studies have shown that no passive absorption of the allergen through the oral mucosa occurs. Evidence points towards the allergen being taken up through the oral mucosa by dendritic cells, in particular Langerhans cells. Allergen which is not absorbed in this manner is expected to be hydrolysed to amino acids and small polypeptides in the lumen of the gastrointestinal tract. There is no evidence to suggest that the allergens present in ACARIZAX are absorbed into the vascular system after sublingual administration to any significant extent.
5.3. Preclinical safety data
Conventional studies of general toxicology and toxicity to reproduction in mice have revealed no special hazards to humans.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.