AIMOVIG Solution for injection Ref.[8685] Active ingredients: Erenumab
Source: European Medicines Agency (EU) Revision Year: 2020 Publisher: Novartis Europharm Limited, Vista Building, Elm Park, Merrion Road, Dublin 4, Ireland
Pharmacodynamic properties
Pharmacotherapeutic group: Analgesics, antimigraine preparations
ATC code: N02CX07
Mechanism of action
Erenumab is a human monoclonal antibody that binds to the calcitonin gene-related peptide (CGRP) receptor. The CGRP receptor is located at sites that are relevant to migraine pathophysiology, such as the trigeminal ganglion. Erenumab potently and specifically competes with the binding of CGRP and inhibits its function at the CGRP receptor, and has no significant activity against other calcitonin family of receptors.
CGRP is a neuropeptide that modulates nociceptive signalling and a vasodilator that has been associated with migraine pathophysiology. In contrast with other neuropeptides, CGRP levels have been shown to increase significantly during migraine and return to normal with headache relief. Intravenous infusion of CGRP induces migraine-like headache in patients.
Inhibition of the effects of CGRP could theoretically attenuate compensatory vasodilation in ischaemic-related conditions. A study evaluated the effect of a single intravenous dose of 140 mg Aimovig in subjects with stable angina under controlled exercise conditions. Aimovig showed similar exercise duration compared to placebo and did not aggravate myocardial ischaemia in these patients.
Clinical efficacy and safety
Aimovig (erenumab) was evaluated for prophylaxis of migraine in two pivotal studies across the migraine spectrum in chronic and episodic migraine. In both studies, the patients enrolled had at least a 12-month history of migraine (with or without aura) according to the International Classification of Headache Disorders (ICHD-III) diagnostic criteria. Elderly patients (>65 years), patients with opioid overuse in study in chronic migraine, patients with medication overuse in study in episodic migraine, and also patients with pre-existing myocardial infarction, stroke, transient ischaemic attacks, unstable angina, coronary artery bypass surgery or other re-vascularisation procedures within 12 months prior to screening were excluded. Patients with poorly controlled hypertension or BMI >40 were excluded from Study 1.
Chronic migraine
Study 1
Aimovig (erenumab) was evaluated as monotherapy for prophylaxis of chronic migraine in a randomised, multicentre, 12-week, placebo-controlled, double-blind study in patients suffering from migraine with or without aura (≥15 headache days per month with ≥8 migraine days per month).
667 patients were randomised in a 3:2:2 ratio to receive placebo (n=286) or 70 mg (n=191) or 140 mg (n=190) erenumab, stratified by the presence of acute medication overuse (present in 41% of overall patients). Patients were allowed to use acute headache treatments during the study.
Demographics and baseline disease characteristics were balanced and comparable between study arms. Patients had a median age of 43 years, 83% were female and 94% were white. The mean migraine frequency at baseline was approximately 18 migraine days per month. Overall, 68% had failed one or more previous prophylactic pharmacotherapies due to lack of efficacy or poor tolerability, and 49% had failed two or more previous prophylactic pharmacotherapies due to lack of efficacy or poor tolerability. A total of 366 (96%) patients in the erenumab arms and 265 (93%) patients in the placebo arm completed the study (i.e. completed Week 12 assessment).
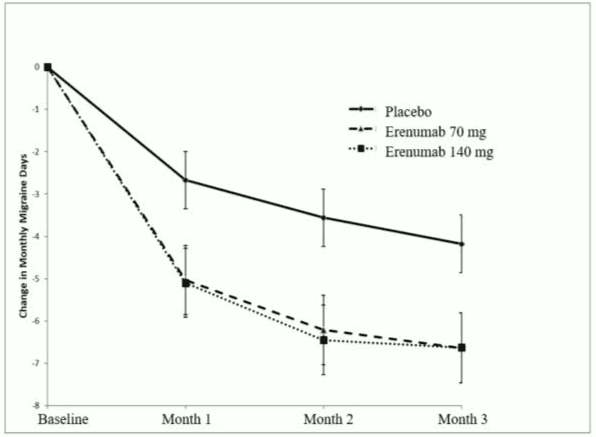
Reduction in mean monthly migraine days from placebo was observed in a monthly analysis from Month 1 and in a follow-up weekly analysis an onset of erenumab effect was seen from the first week of administration.
Figure 1. Change from baseline in monthly migraine days over time in Study 1 (including primary endpoint at Month 3):
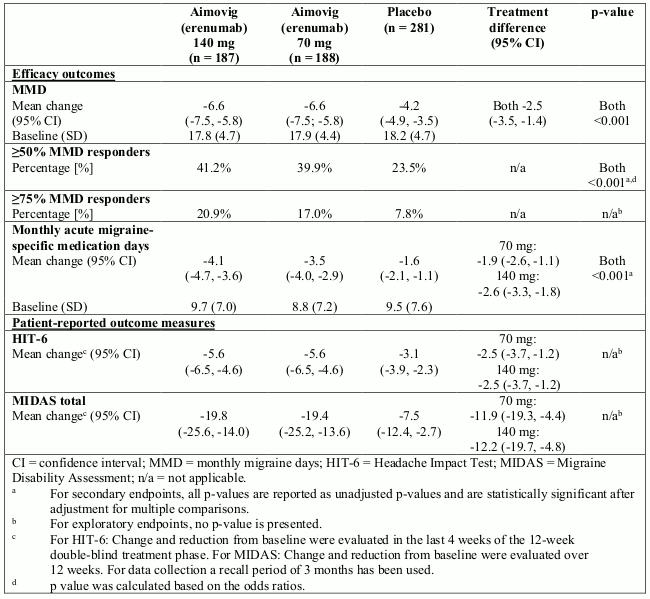
Table 2. Change from baseline in efficacy and patient-reported outcomes at Week 12 in Study 1:
In patients failing one or more prophylactic pharmacotherapies the treatment difference for the reduction of monthly migraine days (MMD) observed between erenumab 140 mg and placebo was -3.3 days (95% CI: -4.6, -2.1) and between erenumab 70 mg and placebo -2.5 days (95% CI: -3.8, -1.2). In patients failing two or more prophylactic pharmacotherapies the treatment difference was -4.3 days (95% CI: -5.8; -2.8) between 140 mg and placebo and -2.7 days (95% CI: -4.2, -1.2) between 70 mg and placebo. There was also a higher proportion of subjects treated with erenumab who achieved at least 50% reduction of MMD compared to placebo in the patients failing one or more prophylactic pharmacotherapies (40.8% for 140 mg, 34.7% for 70 mg versus 17.3% for placebo), with an odds ratio of 3.3 (95% CI: 2.0, 5.5) for 140 mg and 2.6 (95% CI: 1.6, 4.5) for 70 mg. In patients failing two or more prophylactic pharmacotherapies the proportion was 41.3% for 140 mg and 35.6% for 70 mg versus 14.2% for placebo with an odds ratio of 4.2 (95% CI: 2.2, 7.9) and 3.5 (95% CI: 1.8, 6.6), respectively.
Approximately 41% of patients in the study had medication overuse. The treatment difference observed between erenumab 140 mg and placebo and between erenumab 70 mg and placebo for the reduction of MMD in these patients was -3.1 days (95% CI: -4.8, -1.4) in both cases, and for the reduction of acute migraine-specific medication days was -2.8 (95% CI: -4.2, -1.4) for 140 mg and -3.3 (95% CI: -4.7, -1.9) for 70 mg. There was a higher proportion of patients in the erenumab group who achieved at least a 50% reduction of MMD compared to placebo (34.6% for 140 mg, 36.4% for 70 mg versus 17.7% for placebo), with an odds ratio of 2.5 (95% CI: 1.3, 4.9) and 2.7 (95% CI: 1.4, 5.2), respectively.
Efficacy was sustained for up to 1 year in the open-label extension of Study 1 in which patients received 70 mg and/or 140 mg erenumab. 74.1% of patients completed the 52-week extension. Pooled across the two doses, a reduction of -9.3 MMD was observed after 52 weeks relative to core study baseline. 59% of patients completing the study achieved a 50% response in the last month of the study.
Episodic migraine
Study 2
Aimovig (erenumab) was evaluated for prophylaxis of episodic migraine in a randomised, multicentre, 24-week, placebo-controlled, double-blind study in patients suffering from migraine with or without aura (4-14 migraine days per month).
955 patients were randomised in a 1:1:1 ratio to receive 140 mg (n=319) or 70 mg (n=317) erenumab or placebo (n=319). Patients were allowed to use acute headache treatments during the study.
Demographics and baseline disease characteristics were balanced and comparable between study arms. Patients had a median age of 42 years, 85% were female and 89% were white. The mean migraine frequency at baseline was approximately 8 migraine days per month. Overall, 39% had failed one or more previous prophylactic pharmacotherapies due to lack of efficacy or poor tolerability. A total of 294 patients (92%) for 140 mg, 287 (91%) patients for 70 mg and 284 patients (89%) in the placebo arm completed the double-blind phase.
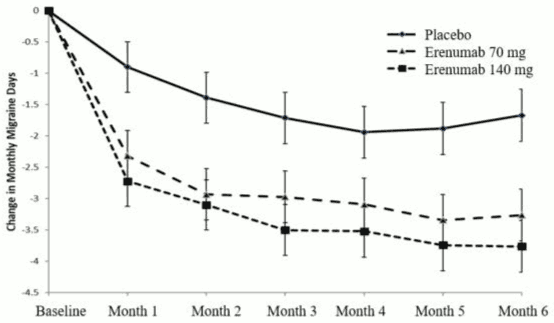
Patients treated with erenumab had a clinically relevant and statistically significant reduction from baseline in the frequency of migraine days from Months 4 to 6 (Figure 2) compared to patients receiving placebo. Differences from placebo were observed from Month 1 onwards.
Figure 2. Change from baseline in monthly migraine days over time in Study 2 (including primary endpoint over Months 4, 5 and 6):
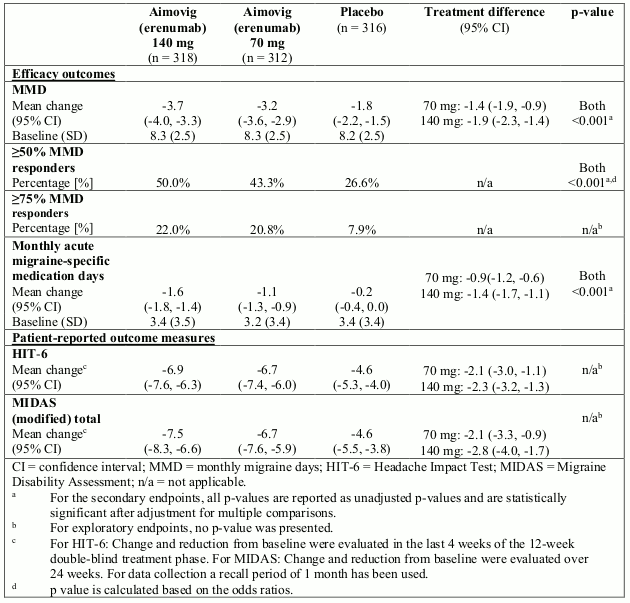
Table 3. Change from baseline in efficacy and patient-reported outcomes at Weeks 13-24 in Study 2:
In patients failing one or more prophylactic pharmacotherapies the treatment difference for the reduction of MMD observed between erenumab 140 mg and placebo was -2.5 (95% CI: -3.4, -1.7) and between erenumab 70 mg and placebo -2.0 (95% CI: -2.8, -1.2). There was also a higher proportion of subjects treated with erenumab who achieved at least 50% reduction of MMD compared to placebo (39.7% for 140 mg and 38.6% for 70 mg, with an odds ratio of 3.1 [95% CI: 1.7, 5.5] and 2.9 [95% CI: 1.6, 5.3], respectively).
Efficacy was sustained up to 1 year in the active re-randomisation part of Study 2. Patients were re-randomised in the active treatment phase (ATP) to 70 mg or 140 mg erenumab. 79.8% completed the entire study out to 52 weeks. The reduction in monthly migraine days from baseline to Week 52 was -4.22 in the 70 mg ATP group and -4.64 days in the 140 mg ATP group. At Week 52, the proportion of subjects who achieved a ≥50% reduction in MMD from baseline was 61.0% in the 70 mg ATP and 64.9% in the 140 mg ATP group.
Paediatric population
The European Medicines Agency has deferred the obligation to submit the results of studies with Aimovig in prevention of migraine headaches in one or more subsets of the paediatric population (see section 4.2 for information on paediatric use).
Pharmacokinetic properties
Erenumab exhibits non-linear kinetics as a result of binding to the CGRP-R receptor. However, at therapeutically relevant doses, the pharmacokinetics of erenumab following subcutaneous dosing every 4 weeks are predominantly linear due to saturation of binding to CGRP-R. Subcutaneous administration of a 140 mg once monthly dose and a 70 mg once monthly dose in healthy volunteers resulted in a Cmax mean (standard deviation [SD]) of 15.8 (4.8) μg/ml and 6.1 (2.1) μg/ml, respectively, and AUClast mean (SD) of 505 (139) day*μg/ml and 159 (58) day*μg/ml, respectively.
Less than 2-fold accumulation was observed in trough serum concentrations following 140 mg doses administered subcutaneously every 4 weeks and serum trough concentrations approached steady state by 12 weeks of dosing.
Absorption
Following a single subcutaneous dose of 140 mg or 70 mg erenumab administered to healthy adults, median peak serum concentrations were attained in 4 to 6 days, and estimated absolute bioavailability was 82%.
Distribution
Following a single 140 mg intravenous dose, the mean (SD) volume of distribution during the terminal phase (Vz) was estimated to be 3.86 (0.77) l.
Biotransformation/Elimination
Two elimination phases were observed for erenumab. At low concentrations, the elimination is predominately through saturable binding to target (CGRP-R), while at higher concentrations the elimination of erenumab is largely through a non-specific proteolytic pathway. Throughout the dosing period erenumab is predominantly eliminated via a non-specific proteolytic pathway with the effective half-life of 28 days.
Special populations
Patients with renal impairment
Patients with severe renal impairment (eGFR <30 ml/min/1.73 m²) have not been studied. Population pharmacokinetic analysis of integrated data from the Aimovig clinical studies did not reveal a difference in the pharmacokinetics of erenumab in patients with mild or moderate renal impairment relative to those with normal renal function (see section 4.2).
Patients with hepatic impairment
No studies have been performed in patients with hepatic impairment. Erenumab, as a human monoclonal antibody, is not metabolised by cytochrome P450 enzymes and hepatic clearance is not a major clearance pathway for erenumab (see section 4.2).
Preclinical safety data
Non-clinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated-dose toxicity, toxicity to reproduction and development.
Carcinogenicity studies have not been conducted with erenumab. Erenumab is not pharmacologically active in rodents. It has biological activity in cynomolgus monkeys, but this species is not an appropriate model for evaluation of tumorigenic risk. The mutagenic potential of erenumab has not been evaluated; however, monoclonal antibodies are not expected to alter DNA or chromosomes.
In repeated-dose toxicology studies there were no adverse effects in sexually mature monkeys dosed up to 150 mg/kg subcutaneously twice weekly for up to 6 months at systemic exposures up to 123-fold and 246-fold higher than the clinical dose of 140 mg and 70 mg, respectively, every 4 weeks, based on serum AUC. There were also no adverse effects on surrogate markers of fertility (anatomical pathology or histopathology changes in reproductive organs) in these studies.
In a reproduction study in cynomolgus monkeys there were no effects on pregnancy, embryo-foetal or post-natal development (up to 6 months of age) when erenumab was dosed throughout pregnancy at exposure levels approximately 17-fold and 34-fold higher than those achieved in patients receiving erenumab 140 mg and 70 mg, respectively, every 4 weeks dosing regimen based on AUC. Measurable erenumab serum concentrations were observed in the infant monkeys at birth, confirming that erenumab, like other IgG antibodies, crosses the placental barrier.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.