APTIOM Tablet Ref.[10749] Active ingredients: Eslicarbazepine
Source: FDA, National Drug Code (US) Revision Year: 2020
12.1. Mechanism of Action
APTIOM is extensively converted to eslicarbazepine, which is considered to be responsible for therapeutic effects in humans. The precise mechanism(s) by which eslicarbazepine exerts anticonvulsant activity is unknown but is thought to involve inhibition of voltage-gated sodium channels.
12.2. Pharmacodynamics
The effect of APTIOM on cardiac repolarization was evaluated in a randomized, double-blind, placebo- and active-controlled 4-period crossover trial in healthy adult men and women. Subjects received APTIOM 1200 mg once daily × 5 days, APTIOM 2400 mg once daily × 5 days, an active-control, moxifloxacin 400 mg × 1 dose on Day 5, and placebo once daily × 5 days. At both doses of APTIOM, no significant effect on the QTc interval was detected.
12.3. Pharmacokinetics
The pharmacokinetics of eslicarbazepine is linear and dose-proportional in the dose range of 400 mg to 1600 mg once daily, both in healthy adult subjects and patients. The apparent half-life of eslicarbazepine in plasma was 13-20 hours in adult epilepsy patients. Steady-state plasma concentrations are attained after 4 to 5 days of once daily dosing.
Absorption, Distribution, Metabolism, and Excretion
Absorption
APTIOM is mostly undetectable (0.01% of the systemic exposure) after oral administration. Eslicarbazepine, the major metabolite, is primarily responsible for the pharmacological effect of APTIOM. Peak plasma concentrations (Cmax) of eslicarbazepine are attained at 1-4 hours post-dose. Eslicarbazepine is highly bioavailable, because the amount of eslicarbazepine and glucuronide metabolites recovered in urine corresponded to more than 90% of an APTIOM dose. Food has no effect on the pharmacokinetics of eslicarbazepine after oral administration of APTIOM.
Distribution
The binding of eslicarbazepine to plasma proteins is relatively low (<40%) and independent of concentration. In vitro studies have shown that plasma protein binding was not relevantly affected by the presence of warfarin, diazepam, digoxin, phenytoin, or tolbutamide. Similarly, the binding of warfarin, diazepam, digoxin, phenytoin or tolbutamide was not significantly affected by the presence of eslicarbazepine. The apparent volume of distribution of eslicarbazepine is 61 L for body weight of 70 kg based on population PK analysis.
Metabolism
APTIOM is rapidly and extensively metabolized to its major active metabolite eslicarbazepine by hydrolytic first-pass metabolism. Eslicarbazepine corresponds to 91% of systemic exposure. The systemic exposure to minor active metabolites of (R)-licarbazepine is 5% and oxcarbazepine is 1%. The inactive glucuronides of these active metabolites correspond to approximately 3% of systemic exposure.
In in vitro studies in human liver microsomes, eslicarbazepine had no clinically relevant inhibitory effect on the activity of CYP1A2, CYP2A6, CYP2B6, CYP2D6, CYP2E1, and CYP3A4, and only a moderate inhibitory effect on CYP2C19. Studies with eslicarbazepine in fresh human hepatocytes showed no induction of enzymes involved in glucuronidation and sulfation of 7-hydroxy-coumarin. A mild activation of UGT1A1-mediated glucuronidation was observed in human hepatic microsomes.
No apparent autoinduction of metabolism has been observed with APTIOM in humans.
Excretion
APTIOM metabolites are eliminated from the systemic circulation primarily by renal excretion, in the unchanged and glucuronide conjugate forms. In total, eslicarbazepine and its glucuronide account for more than 90% of total metabolites excreted in urine, approximately two thirds in the unchanged form and one third as glucuronide conjugate. Other minor metabolites account for the remaining 10% excreted in the urine. In healthy subjects with normal renal function, the renal clearance of eslicarbazepine (approximately 20 mL/min) is substantially lower than glomerular filtration rate (80-120 mL/min), suggesting that renal tubular reabsorption occurs. The apparent plasma half-life of eslicarbazepine was 13-20 hours in epilepsy patients [see Dosage and Administration (2.4) and Use in Specific Populations (8.6)].
Specific Populations
Geriatric Patients (≥65 Years of Age)
The pharmacokinetic profile of eslicarbazepine was unaffected in elderly subjects with creatinine clearance >60 mL/min compared to healthy subjects (18-40 years) after single and repeated doses of 600 mg APTIOM during 8 days of dosing. No dose adjustment is necessary in adults based on age, if CrCl is ≥50 mL/min.
Pediatric Patients (4 to 17 Years of Age)
A pharmacokinetic study of APTIOM was performed in 29 pediatric patients with partial-onset seizures. Limited pharmacokinetic sampling was also performed during controlled pediatric adjunctive therapy partial-onset seizure studies. As in adult patients, APTIOM is rapidly and extensively metabolized to its major active metabolite eslicarbazepine. The pharmacokinetics of eslicarbazepine is linear and dose-proportional in the dose range of 5 to 30 mg/kg/day. Peak plasma concentrations (Cmax) of eslicarbazepine are attained at 1-3 hours post-dose.
A population pharmacokinetic analysis showed that body weight significantly correlates with the clearance of eslicarbazepine in pediatric patients; clearance increased with an increase in body weight. A weight-based dosing regimen is necessary to achieve eslicarbazepine exposures in pediatric patients aged 4 to 17 years similar to those observed in adults treated at effectives doses of APTIOM [see Dosage and Administration (2.2)]. The apparent half-life of eslicarbazepine in plasma was 10-16 hours in pediatric patients with partial-onset seizures. Steady-state plasma concentrations are attained after 4 to 5 days of once-daily dosing.
The pharmacokinetics of eslicarbazepine in pediatric patients are similar when used as monotherapy or as adjunctive therapy for the treatment of partial-onset seizures.
Gender
Studies in healthy subjects and patients showed that pharmacokinetics of eslicarbazepine was not affected by gender.
Race
No clinically significant effect of race (Caucasian N=849, Black N=53, Asian N=65, and Other N=51) on the pharmacokinetics of eslicarbazepine was noted in a population pharmacokinetic analysis of pooled data from the clinical studies.
Renal Impairment
APTIOM metabolites are eliminated from the systemic circulation primarily by renal excretion. The extent of systemic exposure of eslicarbazepine following an 800 mg single dose was increased by 62% in patients with mild renal impairment (CrCl 50-80 mL/min), by 2-fold in patients with moderate renal impairment (CrCl 30-49 mL/min) and by 2.5-fold in patients with severe renal impairment (CrCl <30 mL/min) in comparison to the healthy subjects (CrCl >80 mL/min). Dosage adjustment is recommended in patients with creatinine clearance below 50 mL/min [see Dosage and Administration (2.4) and Use in Specific Populations (8.6)].
In patients with end stage renal disease, repeated hemodialysis removed APTIOM metabolites from systemic circulation.
Hepatic Impairment
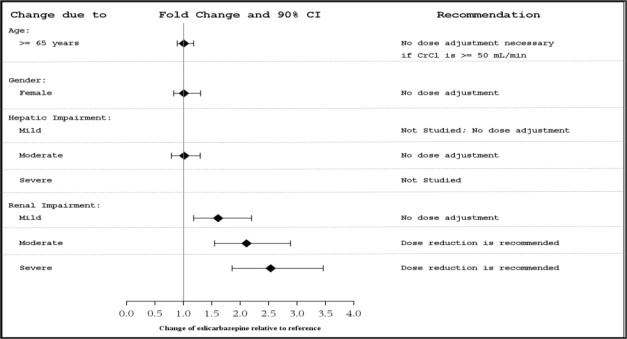
The pharmacokinetics and metabolism of APTIOM was evaluated in healthy subjects and patients with moderate liver impairment (7-9 points on the Child-Pugh assessment) after multiple oral doses (see Figure 1). Moderate hepatic impairment did not affect the pharmacokinetics of APTIOM. No dose adjustment is recommended in patients with mild to moderate liver impairment.
The pharmacokinetics of APTIOM has not been studied in patients with severe hepatic impairment.
Figure 1. Impact of Intrinsic Factors on AUC of Eslicarbazepine:
Drug Interaction Studies
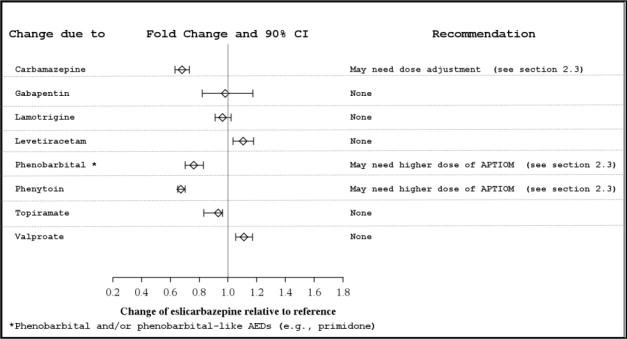
Potential for Other AEDs to Affect Eslicarbazepine
The potential impact of other AEDs on the systemic exposure (area under the curve, AUC) of eslicarbazepine, the active metabolite of APTIOM, is shown in Figure 2:
Figure 2. Potential Impact of Other AEDs on AUC of Eslicarbazepine:
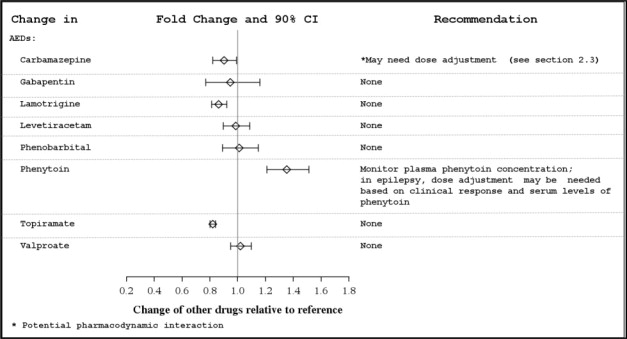
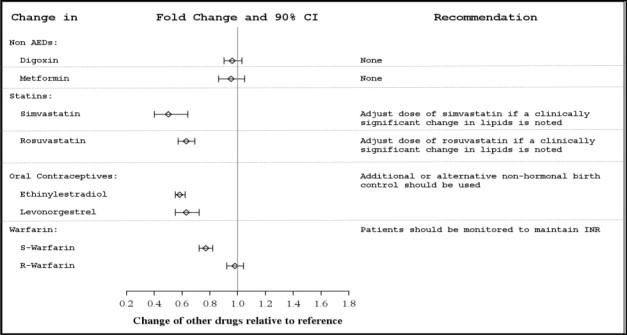
Potential for APTIOM to Affect Other Drugs
The potential impact of APTIOM on the systemic exposure (AUC) of other drugs (including AEDs) is shown in Figures 3a and 3b:
Figure 3a. Potential Impact of APTIOM on the AUC of AEDs:
Figure 3b. Potential Impact of APTIOM on the AUC of Non-AEDs:
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
In a two-year carcinogenicity study in mice, eslicarbazepine acetate was administered orally at doses of 100, 250, and 600 mg/kg/day. An increase in the incidence of hepatocellular adenomas and carcinomas was observed at 250 and 600 mg/kg/day in males and at 600 mg/kg/day in females. The dose not associated with an increase in tumors (100 mg/kg/day) is less than the MRHD (1600 mg/day for monotherapy) on a mg/m² basis.
Mutagenesis
Eslicarbazepine acetate and eslicarbazepine were not mutagenic in the in vitro Ames assay. In in vitro assays in mammalian cells, eslicarbazepine acetate and eslicarbazepine were not clastogenic in human peripheral blood lymphocytes; however, eslicarbazepine acetate was clastogenic in Chinese hamster ovary (CHO) cells, with and without metabolic activation. Eslicarbazepine acetate was positive in the in vitro mouse lymphoma tk assay in the absence of metabolic activation. Eslicarbazepine acetate was not clastogenic in the in vivo mouse micronucleus assay.
Impairment of Fertility
When eslicarbazepine acetate (150, 350, and 650 mg/kg/day) was orally administered to male and female mice prior to and throughout the mating period, and continuing in females to gestation day 6, there was an increase in embryolethality at all doses. The lowest dose tested is less than the MRHD on a mg/m² basis.
When eslicarbazepine acetate (65, 125, 250 mg/kg/day) was orally administered to male and female rats prior to and throughout the mating period, and continuing in females to implantation, lengthening of the estrus cycle was observed at the highest dose tested. The data in rats are of uncertain relevance to humans because of differences in metabolic profile between species.
14. Clinical Studies
14.1 Monotherapy for Partial-Onset Seizures
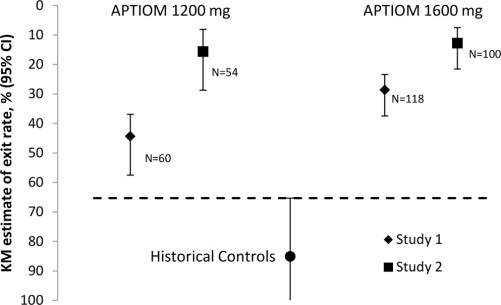
The effectiveness of APTIOM as monotherapy for partial-onset seizures was established in two identical, dose-blinded historical control trials in a total of 365 patients with epilepsy (Study 1 and Study 2). In these trials, patients were randomized in a 2:1 ratio to receive either APTIOM 1600 mg or 1200 mg once daily, and their responses were compared to those of a historical control group. The historical control methodology is described in a publication by French et al. [see References (15)]. The historical control consisted of a pooled analysis of the control groups from 8 trials of similar design, which utilized a subtherapeutic dose of an AED as a comparator. Statistical superiority to the historical control was considered to be demonstrated if the upper limit from a 2-sided 95% confidence interval for the percentage of patients meeting exit criteria in patients receiving APTIOM remained below the lower 95% prediction interval of 65% derived from the historical control data.
In Study 1 and Study 2, patients ≥16 years of age experienced at least 4 seizures during the baseline period with no 28-day seizure free period while receiving 1 or 2 AEDs (both could not be sodium-channel blocking drugs, and at least one AED was limited to ⅔ of a typical dose). APTIOM was titrated over a 1- to 2-week period followed by the gradual withdrawal of the background AED over a 6-week period, followed by a 10-week monotherapy period.
The exit criteria were one or more of the following: (1) an episode of status epilepticus, (2) emergence of a generalized tonic-clonic seizure in patients who had not had one in the past 6 months, (3) doubling of average monthly seizure count during any 28 consecutive days, (4) doubling of highest consecutive 2-day seizure frequency during the entire treatment phase, or (5) worsening of seizure severity considered by the investigator to require intervention. The primary endpoint was the cumulative 112-day exit rate in the efficacy population. Additionally, in Studies 1 and 2, if the discontinuation rate exceeded 10%, patients were randomly reassigned to be counted as exits.
The most commonly used baseline AEDs were carbamazepine, levetiracetam, valproic acid, and lamotrigine. Oxcarbazepine was used as a baseline AED in 6.6% of patients.
In Study 1, the Kaplan-Meier (K-M) estimate of the percentage of patients meeting at least 1 exit criterion was 29% (95% CI: 21%, 38%) in the 1600 mg group and 44% (95% CI 33%, 58%) in the 1200 mg group. In Study 2, the K-M estimate of the percentage of patients meeting at least 1 exit criterion was 13% (95% CI: 8%, 22%) in the 1600 mg group and 16% (95% CI: 8%, 29%) in the 1200 mg group. The upper limit of the 2-sided 95% CI of both doses in both trials were below the threshold of 65% derived from the historical control data, meeting the pre-specified criteria for efficacy (see Figure 4).
Figure 4. Kaplan-Meier Estimates of Cumulative 112-Day Exit Rates for Studies 1 and 2:
14.2 Adjunctive Therapy for Partial-Onset Seizures
The efficacy of APTIOM as adjunctive therapy in partial-onset seizures was established in three randomized, double-blind, placebo-controlled, multicenter trials in adult patients with epilepsy (Study 3, Study 4, and Study 5). Patients enrolled had partial-onset seizures with or without secondary generalization and were not adequately controlled with 1 to 3 concomitant AEDs. During an 8-week baseline period, patients were required to have an average of ≥4 partial-onset seizures per 28 days with no seizure-free period exceeding 21 days. In these three trials, patients had a median duration of epilepsy of 19 years and a median baseline seizure frequency of 8 seizures per 28 days. Two-thirds (69%) of subjects used 2 concomitant AEDs and 28% used 1 concomitant AED. The most commonly used AEDs were carbamazepine (50%), lamotrigine (24%), valproic acid (21%), and levetiracetam (18%). Oxcarbazepine was not allowed as a concomitant AED.
Studies 3 and 4 compared dosages of APTIOM 400, 800, and 1200 mg once daily with placebo. Study 5 compared dosages of APTIOM 800 and 1200 mg once daily with placebo. In all three trials, following an 8-week Baseline Phase, which established a baseline seizure frequency, subjects were randomized to a treatment arm. Patients entered a treatment period consisting of an initial titration phase (2 weeks), and a subsequent maintenance phase (12 weeks). The specific titration schedule differed amongst the three studies. Thus, patients were started on a daily dose of 400 mg or 800 mg and subsequently increased by 400 mg/day following one or two weeks, until the final daily target dose was achieved.
The standardized seizure frequency during the Maintenance Phase over 28 days was the primary efficacy endpoint in all three trials. Table 5 presents the results for the primary endpoint, as well as the secondary endpoint of percent reduction from baseline in seizure frequency. The APTIOM treatment at 400 mg/day was studied in Studies 3 and 4 and did not show significant treatment effect. A statistically significant effect was observed with APTIOM treatment at doses of 800 mg/day in Studies 3 and 4, but not in Study 5, and at doses of 1200 mg/day in all 3 studies.
Table 5. Standardized Seizure Frequency During the Maintenance Phase Over 28 Days and Percent Reduction from Baseline in Seizure Frequency:
| Placebo | APTIOM | ||
|---|---|---|---|
| 800 mg | 1200 mg | ||
| Study 3 | |||
| N | 95 | 88 | 87 |
| Seizure Frequency (LS Mean seizures per 28 days) (p-value) | 6.6 | 5.0 (0.047*) | 4.3 (0.001*) |
| Median Percent Reduction from Baseline in Seizure Frequency (%) | -15 | -36 | -39 |
| Study 4 | |||
| N | 99 | 87 | 81 |
| Seizure Frequency (LS Mean seizures per 28 days) (p-value) | 8.6 | 6.2 (0.006*) | 6.6 (0.042*) |
| Median Percent Reduction from Baseline in Seizure Frequency (%) | -6 | -33 | -28 |
| Study 5 | |||
| N | 212 | 200 | 184 |
| Seizure Frequency (LS Mean seizures per 28 days) (p-value) | 7.9 | 6.5 (0.058) | 6.0 (0.004*) |
| Median Percent Reduction from Baseline in Seizure Frequency (%) | -22 | -30 | -36 |
* statistically significant compared to placebo
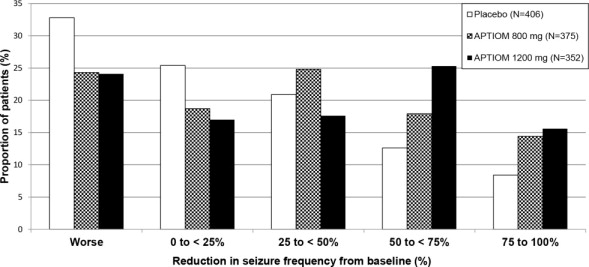
Figure 5 shows changes from baseline in the 28-day total partial seizure frequency by category of reduction in seizure frequency from baseline for patients treated with APTIOM and placebo in an integrated analysis across the three clinical trials. Patients in whom the seizure frequency increased are shown to the left as “Worse.” Patients in whom the seizure frequency decreased are shown in four categories.
Figure 5. Proportion of Patients by Category of Seizure Reduction for APTIOM and Placebo Across All Three Double-blind Trials:
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.