BYANNLI Prolonged-release suspension for injection Ref.[50946] Active ingredients: Paliperidone
Source: European Medicines Agency (EU) Revision Year: 2022 Publisher: Janssen-Cilag International NV, Turnhoutseweg 30, B-2340 Beerse, Belgium
5.1. Pharmacodynamic properties
Pharmacotherapeutic group: Psycholeptics, other antipsychotics
ATC code: N05AX13
BYANNLI contains a racemic mixture of (+)- and (-)-paliperidone.
Mechanism of action
Paliperidone is a selective blocking agent of monoamine effects, whose pharmacological properties are different from that of traditional neuroleptics. Paliperidone binds strongly to serotonergic 5-HT2-and dopaminergic D2-receptors. Paliperidone also blocks alpha 1-adrenergic receptors and slightly less, H1-histaminergic and alpha 2-adrenergic receptors. The pharmacological activity of the (+)- and (-)-paliperidone enantiomers are qualitatively and quantitatively similar.
Paliperidone is not bound to cholinergic receptors. Even though paliperidone is a strong D2-antagonist, which is believed to relieve the symptoms of schizophrenia, it causes less catalepsy and decreases motor functions less than traditional neuroleptics. Dominating central serotonin antagonism may reduce the tendency of paliperidone to cause extrapyramidal side effects.
Clinical efficacy
The efficacy of BYANNLI for the treatment of schizophrenia in patients who had previously been adequately treated with either 1-monthly paliperidone palmitate injection for at least 4 months or 3-monthly paliperidone palmitate injectable for at least one 3-month injection cycle was evaluated in a Phase 3, randomised, double-blind, active-controlled, interventional, parallel-group, multicentre, non-inferiority study in adult patients. The primary outcome was time to relapse.
The study consisted of an open-label phase which included screening, transition and maintenance phases, followed by a 12-month double-blind phase in which patients were randomised to receive either BYANNLI or 3-monthly paliperidone palmitate injectable. 702 adequately treated patients were randomised in a 2:1 ratio to receive BYANNLI (478 patients) or 3-monthly paliperidone palmitate injectable (224 patients). Patients received either 2 injection cycles of BYANNLI (4 injections in total; BYANNLI with alternating placebo) or 4 injections of 3-monthly paliperidone palmitate injection every 3 months with regular scheduled visits between injections over the 12-month study duration. Dose adjustment was not permitted during the double-blind phase. Patients remained in this phase until they experienced a relapse event, met discontinuation/withdrawal criteria, or study conclusion.
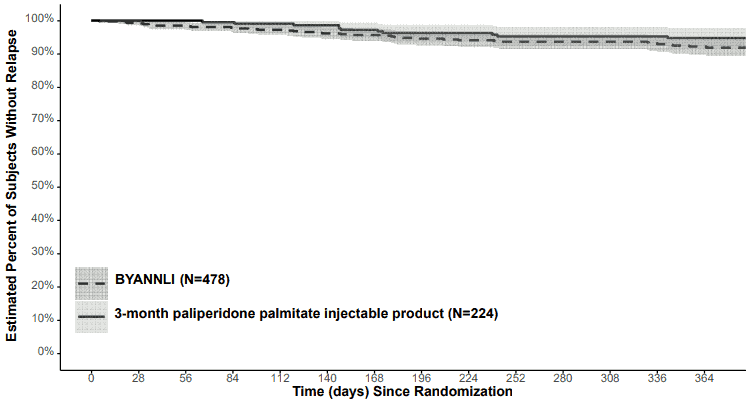
7.5% of patients in the BYANNLI treatment group and 4.9% of patients in the 3-monthly paliperidone palmitate injectable treatment group experienced a relapse event in the 12-month double-blind Phase with the Kaplan-Meier estimated difference (BYANNLI – 3-monthly paliperidone palmitate injection) of 2.9% (95% CI: -1.1% to 6.8%). The Kaplan-Meier plot (with 95% pointwise confidence bands) of time from randomisation to impending relapse during the 12-month double-blind, active-controlled Phase for BYANNLI 700 and 1 000 mg and 3-monthly paliperidone palmitate injectable 350 mg and 525 mg is shown in Figure 1.
Figure 1. Kaplan-Meier Plot (with 95% pointwise confidence bands) of percentage of subjects without relapse:
The efficacy results were consistent across population subgroups (gender, age, and race) in both treatment arms.
It was determined that the efficacy of BYANNLI was noninferior to the efficacy of 3-monthly paliperidone palmitate injection in adults with a DSM-5 diagnosis of schizophrenia. The upper bound of the 95% CI (6.8%) was less than 10%, the prespecified non-inferiority margin.
Paediatric population
The European Medicines Agency has waived the obligation to submit the results of studies with BYANNLI in all subsets of the paediatric population in schizophrenia (see section 4.2 for information on paediatric use).
5.2. Pharmacokinetic properties
The pharmacokinetics for BYANNLI are presented after gluteal administration only.
Absorption and distribution
Due to its extremely low water solubility, the 6-monthly formulation of paliperidone palmitate dissolves slowly after intramuscular injection before being hydrolysed to paliperidone and absorbed into the systemic circulation. The release of the active substance after a single dose of 3-monthly paliperidone palmitate injectable starts as early as day 1 and lasts for as long as 18 months. The release of BYANNLI is expected to last longer. Paliperidone plasma concentrations have only been studied up to 6 months after administration of BYANNLI. Based on population pharmacokinetic simulations paliperidone concentrations are expected to remain in plasma for up to approximately 4 years following a single 1 000 mg dose of BYANNLI. The concentration of paliperidone remaining in the circulation approximately 4 years after a single dose of 1 000 mg BYANNLI is expected to be low (<1% of the average steady state levels).
The data presented in this paragraph are based on a population pharmacokinetic analysis. Following a single gluteal intramuscular injection of BYANNLI at doses of 700 and 1 000 mg, the plasma concentrations of paliperidone gradually rise to reach maximum plasma concentrations predicted on days 33 and 35, respectively. The release profile and dosing regimen of BYANNLI results in sustained therapeutic concentrations over 6 months. Cmax and AUC6month of BYANNLI were approximately dose-proportional in the range of 700-1 000 mg. The median steady-state peak:trough ratio is approximately 3.0.
The plasma protein binding of racemic paliperidone is 74%.
Biotransformation and elimination
In a study with oral immediate release 14C-paliperidone, one week following administration of a single oral dose of 1 mg immediate release 14C-paliperidone, 59% of the dose was excreted unchanged into urine, indicating that paliperidone is not extensively metabolised in the liver. Approximately 80% of the administered radioactivity was recovered in urine and 11% in the faeces. Four metabolic pathways have been identified in vivo, none of which accounted for more than 10% of the dose: dealkylation, hydroxylation, dehydrogenation, and benzisoxazole scission. Although in vitro studies suggested a role for CYP2D6 and CYP3A4 in the metabolism of paliperidone, there is no evidence in vivo that these isozymes play a significant role in the metabolism of paliperidone. Population pharmacokinetics analyses indicated no discernible difference on the apparent clearance of paliperidone after administration of oral paliperidone between extensive metabolisers and poor metabolisers of CYP2D6 substrates. In vitro studies in human liver microsomes showed that paliperidone does not substantially inhibit the metabolism of medicines metabolised by cytochrome P450 isozymes, including CYP1A2, CYP2A6, CYP2C8/9/10, CYP2D6, CYP2E1, CYP3A4, and CYP3A5.
In vitro studies have shown that paliperidone is a P-gp substrate and a weak inhibitor of P-gp at high concentrations. No in vivo data are available and the clinical relevance is unknown.
Based on population pharmacokinetic analysis, the median apparent half-life of paliperidone following BYANNLI gluteal administration at doses of 700 and 1 000 mg is estimated to be 148 and 159 days, respectively.
Long-acting 6-monthly paliperidone palmitate injection versus other paliperidone formulations
BYANNLI is designed to deliver paliperidone over a 6-month period, compared to the 1-monthly or 3-monthly products which are administered every month or every three months, respectively. BYANNLI doses of 700 mg and 1 000 mg results in a range of paliperidone exposures similar to those obtained with corresponding doses of 1-monthly or 3-monthly paliperidone palmitate injections or corresponding once daily doses of paliperidone prolonged-release tablets (see section 4.2).
Hepatic impairment
Paliperidone is not extensively metabolised in the liver. Although BYANNLI was not studied in patients with hepatic impairment, no dose adjustment is required in patients with mild or moderate hepatic impairment. In a study with oral paliperidone in subjects with moderate hepatic impairment (Child-Pugh class B), the plasma concentrations of free paliperidone were similar to those of healthy subjects. Paliperidone has not been studied in patients with severe hepatic impairment.
Renal impairment
BYANNLI has not been systematically studied in patients with renal impairment. The disposition of a single oral dose of a paliperidone 3 mg prolonged-release tablet was studied in subjects with varying degrees of renal function. Elimination of paliperidone decreased with decreasing estimated creatinine clearance. Total clearance of paliperidone was reduced in subjects with impaired renal function by 32% on average in mild (CrCl = 50 to ≤80 mL/min), 64% in moderate (CrCl = 30 to ≤50 mL/min), and 71% in severe (CrCl = 10 to <30 mL/min) renal impairment, corresponding to an average increase in exposure (AUCinf) of 1.5, 2.6, and 4.8-fold, respectively, compared to healthy subjects.
Elderly
Population pharmacokinetics analysis showed no evidence of age related pharmacokinetics differences.
Body mass index (BMI)/body weight
Lower Cmax was observed in overweight and obese subjects. At apparent steady-state with BYANNLI, the trough concentrations were similar among normal, overweight, and obese subjects.
Race
Pharmacokinetic analysis showed no evidence of clinically relevant difference in pharmacokinetics between races.
Gender
Population pharmacokinetics analysis showed no evidence of gender related pharmacokinetics differences.
Smoking status
Based on in vitro studies utilising human liver enzymes, paliperidone is not a substrate for CYP1A2; smoking should, therefore, not have an effect on the pharmacokinetics of paliperidone. Effect of smoking on the pharmacokinetics of paliperidone was not studied with BYANNLI. A population pharmacokinetic analysis based on data with oral paliperidone prolonged-release tablets showed a slightly lower exposure to paliperidone in smokers compared with non-smokers. The difference is not likely to be of clinical relevance.
5.3. Preclinical safety data
Repeat-dose toxicity studies of intramuscularly injected paliperidone palmitate (the 1-monthly formulation) and orally administered paliperidone in rat and dog showed mainly pharmacological effects, such as sedation and prolactin-mediated effects on mammary glands and genitals. In animals treated with paliperidone palmitate an inflammatory reaction was seen at the intramuscular injection site. Occasionally abscess formation occurred.
In rat reproduction studies with oral risperidone, which is extensively converted to paliperidone in rats and humans, adverse effects were seen on the birth weight and survival of the offspring. No embryotoxicity or malformations were observed following intramuscular administration of paliperidone palmitate to pregnant rats up to the highest dose (160 mg/kg/day) corresponding to 1.6 times the exposure level in humans at the maximum recommended dose of 1 000 mg. Other dopamine antagonists, when administered to pregnant animals, have caused negative effects on learning and motor development in the offspring.
Paliperidone palmitate and paliperidone were not genotoxic. In oral carcinogenicity studies of risperidone in rats and mice, increases in pituitary gland adenomas (mouse), endocrine pancreas adenomas (rat), and mammary gland adenomas (both species) were seen. The carcinogenic potential of intramuscularly injected paliperidone palmitate was assessed in rats. There was a statistically significant increase in mammary gland adenocarcinomas in female rats at 10, 30 and 60 mg/kg/month. Male rats showed a statistically significant increase in mammary gland adenomas and carcinomas at 30 and 60 mg/kg/month which is 0.3 and 0.6 times the exposure level at the maximum recommended human 1 000 mg dose. These tumours can be related to prolonged dopamine D2-antagonism and hyperprolactinaemia. The relevance of these tumour findings in rodents in terms of human risk is unknown.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.