DEXILANT Delayed-release capsules Ref.[10006] Active ingredients: Dexlansoprazole
Source: FDA, National Drug Code (US) Revision Year: 2020
12.1. Mechanism of Action
Dexlansoprazole belongs to a class of antisecretory compounds, the substituted benzimidazoles, that suppress gastric acid secretion by specific inhibition of the (H+, K+)-ATPase at the secretory surface of the gastric parietal cell. Because this enzyme is regarded as the acid (proton) pump within the parietal cell, dexlansoprazole has been characterized as a gastric proton-pump inhibitor, in that it blocks the final step of acid production.
12.2. Pharmacodynamics
Antisecretory Activity
The effects of DEXILANT 60 mg (n=20) or lansoprazole 30 mg (n=23) once daily for five days on 24 hour intragastric pH were assessed in healthy subjects in a multiple-dose crossover study. The results are summarized in Table 5.
Table 5. Effect on 24 Hour Intragastric pH on Day 5 After Administration of DEXILANT or Lansoprazole
| DEXILANT 60 mg | Lansoprazole 30 mg |
|---|---|
| Mean Intragastric pH | |
| 4.55 | 4.13 |
| % Time Intragastric pH >4 (hours) | |
| 71 (17 hours) | 60 (14 hours) |
Serum Gastrin Effects
The effect of dexlansoprazole on serum gastrin concentrations was evaluated in approximately 3460 patients in clinical trials up to eight weeks and in 1023 patients for up to six to 12 months. The mean fasting gastrin concentrations increased from baseline during treatment with 30 and 60 mg DEXILANT. In patients treated for more than six months, mean serum gastrin levels increased during approximately the first three months of treatment and were stable for the remainder of treatment. Mean serum gastrin levels returned to pretreatment levels within one month of discontinuation of treatment.
Increased gastrin causes enterochromaffin-like cell hyperplasia and increased serum CgA levels. The increased CgA levels may cause false positive results in diagnostic investigations for neuroendocrine tumors [see Warnings and Precautions (5.8)].
Enterochromaffin-Like Cell (ECL) Effects
There were no reports of ECL cell hyperplasia in gastric biopsy specimens obtained from 653 patients treated with DEXILANT 30, 60, or 90 mg for up to 12 months.
During lifetime exposure of rats dosed daily with up to 150 mg/kg/day of lansoprazole, marked hypergastrinemia was observed followed by ECL cell proliferation and formation of carcinoid tumors, especially in female rats [see Nonclinical Toxicology (13.1)].
Cardiac Electrophysiology
At a dose five times the maximum recommended dose, dexlansoprazole does not prolong the QT interval to any clinically relevant extent.
12.3. Pharmacokinetics
12.3 Pharmacokinetics
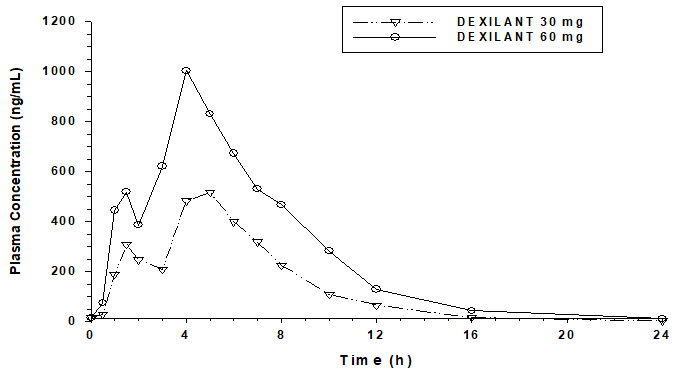
The dual delayed-release formulation of DEXILANT results in a dexlansoprazole plasma concentration-time profile with two distinct peaks; the first peak occurs one to two hours after administration, followed by a second peak within four to five hours (see Figure 1). Dexlansoprazole is eliminated with a half-life of approximately one to two hours in healthy subjects and in patients with symptomatic GERD. No accumulation of dexlansoprazole occurs after multiple, once daily doses of DEXILANT 30 or 60 mg although mean AUCt and Cmax values of dexlansoprazole were slightly higher (less than 10%) on Day 5 than on Day 1.
Figure 1. Mean Plasma Dexlansoprazole Concentration – Time Profile Following Oral Administration of 30 or 60 mg DEXILANT Once Daily for 5 Days in Healthy Adult Subjects:
The pharmacokinetics of dexlansoprazole are highly variable, with percent coefficient of variation (CV) values for Cmax, AUC, and CL/F of greater than 30 (see Table 6).
Table 6. Mean (%CV) Pharmacokinetic Parameters for Adult Subjects on Day 5 After Administration of DEXILANT:
| Dose (mg) | Cmax (ng/mL) | AUC24 (ng∙h/mL) | CL/F (L/h) |
|---|---|---|---|
| 30 | 658 (40%) (N=44) | 3275 (47%) (N=43) | 11.4 (48%) (N=43) |
| 60 | 1397 (51%) (N=79) | 6529 (60%) (N=73) | 11.6 (46%) (N=41) |
Absorption
After oral administration of DEXILANT 30 or 60 mg to healthy subjects and symptomatic GERD patients, mean Cmax and AUC values of dexlansoprazole increased approximately dose proportionally (see Figure 1).
When granules of DEXILANT 60 mg are mixed with water and dosed via NG tube or orally via syringe, the bioavailability (Cmax and AUC) of dexlansoprazole was similar to that when DEXILANT 60 mg was administered as an intact capsule [see Dosage and Administration (2.3)].
Effect on Food
In food-effect studies in healthy subjects receiving DEXILANT under various fed conditions compared to fasting, increases in Cmax ranged from 12 to 55%, increases in AUC ranged from 9 to 37%, and Tmax varied (ranging from a decrease of 0.7 hours to an increase of three hours) [see Dosage and Administration (2.3)].
Distribution
Plasma protein binding of dexlansoprazole ranged from 96 to 99% in healthy subjects and was independent of concentration from 0.01 to 20 mcg/mL. The apparent volume of distribution (Vz/F) after multiple doses in symptomatic GERD patients was 40 L.
Elimination
Metabolism
Dexlansoprazole is extensively metabolized in the liver by oxidation, reduction, and subsequent formation of sulfate, glucuronide and glutathione conjugates to inactive metabolites. Oxidative metabolites are formed by the cytochrome P450 (CYP) enzyme system including hydroxylation mainly by CYP2C19, and oxidation to the sulfone by CYP3A4.
CYP2C19 is a polymorphic liver enzyme which exhibits three phenotypes in the metabolism of CYP2C19 substrates: extensive metabolizers (*1/*1), intermediate metabolizers (*1/mutant) and poor metabolizers (mutant/mutant). Dexlansoprazole is the major circulating component in plasma regardless of CYP2C19 metabolizer status. In CYP2C19 intermediate and extensive metabolizers, the major plasma metabolites are 5-hydroxy dexlansoprazole and its glucuronide conjugate, while in CYP2C19 poor metabolizers dexlansoprazole sulfone is the major plasma metabolite.
Excretion
Following the administration of DEXILANT, no unchanged dexlansoprazole is excreted in urine. Following the administration of [ 14C] dexlansoprazole to six healthy male subjects, approximately 50.7% (standard deviation (SD): 9.0%) of the administered radioactivity was excreted in urine and 47.6% (SD: 7.3%) in the feces. Apparent clearance (CL/F) in healthy subjects was 11.4 to 11.6 L/hour, respectively, after five days of 30 or 60 mg once daily administration.
Specific Populations
Age: Pediatric Population
The pharmacokinetics of dexlansoprazole in patients under the age of 12 years have not been studied.
Patients 12 to 17 Years of Age:
The pharmacokinetics of dexlansoprazole were studied in 36 patients 12 to 17 years of age with symptomatic GERD in a multicenter trial. Patients were randomized to receive DEXILANT 30 or 60 mg once daily for seven days. The dexlansoprazole mean Cmax and AUC in patients 12 to 17 years of age were 105 and 88%, respectively, compared to those observed in adults at the 30 mg dose, and were 81 and 78%, respectively, at the 60 mg dose (see Tables 6 and 7).
Table 7. Mean (%CV) Pharmacokinetic Parameters in Patients 12 to 17 Years of Age with Symptomatic GERD on Day 7 After Administration of DEXILANT Once Daily for 7 Days:
| Dose | Cmax (ng/mL) | AUCtau (ng∙h/mL) | CL/F (L/h) |
|---|---|---|---|
| 30 mg (N=17) | 691 (53) | 2886 (47) | 12.8 (48) |
| 60 mg (N=18) | 1136 (51) | 5120 (58) | 15.3 (49) |
Age: Geriatric Population
The terminal elimination half-life of dexlansoprazole is significantly increased in geriatric subjects compared to younger subjects (2.2 and 1.5 hours, respectively). Dexlansoprazole exhibited higher systemic exposure (AUC) in geriatric subjects (34% higher) than younger subjects [see Use in Specific Populations (8.5)].
Sex
In a study of 12 male and 12 female healthy subjects who received a single dose of DEXILANT 60 mg, females had higher systemic exposure (AUC) (43% higher) than males. This difference in exposure between males and females does not represent a significant safety concern.
Renal Impairment
Dexlansoprazole is extensively metabolized in the liver to inactive metabolites, and no parent drug is recovered in the urine following an oral dose of dexlansoprazole. Therefore, the pharmacokinetics of dexlansoprazole are not expected to be altered in patients with renal impairment, and no studies were conducted in patients with renal impairment. In addition, the pharmacokinetics of lansoprazole were not clinically different in patients with mild, moderate or severe renal impairment compared to healthy subjects with normal renal function.
Hepatic Impairment
In a study of 12 patients with moderate hepatic impairment (Child-Pugh Class B) who received a single dose of 60 mg DEXILANT, the systemic exposure (AUC) of bound and unbound dexlansoprazole was approximately two times greater compared to subjects with normal hepatic function. This difference in exposure was not due to a difference in protein binding. No studies have been conducted in patients with severe hepatic impairment (Child-Pugh Class C) [see Dosage and Administration (2.2), Use in Specific Populations (8.6)].
Drug-Drug Interactions
Effect of Dexlansoprazole on Other Drugs
Cytochrome P 450 Interactions:
Dexlansoprazole is metabolized, in part, by CYP2C19 and CYP3A4 [see Clinical Pharmacology (12.3)].
In vitro studies have shown that dexlansoprazole is not likely to inhibit CYP isoforms 1A1, 1A2, 2A6, 2B6, 2C8, 2C9, 2D6, 2E1 or 3A4. As such, no clinically relevant interactions with drugs metabolized by these CYP enzymes would be expected. Furthermore, in vivo studies showed that DEXILANT did not have an impact on the pharmacokinetics of coadministered phenytoin (CYP2C9 substrate) or theophylline (CYP1A2 substrate).
The subjects' CYP1A2 genotypes in the drug-drug interaction study with theophylline were not determined. Although in vitro studies indicated that DEXILANT has the potential to inhibit CYP2C19 in vivo, an in vivo drug-drug interaction study in mainly CYP2C19 extensive and intermediate metabolizers has shown that DEXILANT does not affect the pharmacokinetics of diazepam (CYP2C19 substrate).
Clopidogrel:
Clopidogrel is metabolized to its active metabolite in part by CYP2C19. A study of healthy subjects who were CYP2C19 extensive metabolizers, receiving once daily administration of clopidogrel 75 mg alone or concomitantly with DEXILANT 60 mg (n=40), for nine days was conducted. The mean AUC of the active metabolite of clopidogrel was reduced by approximately 9% (mean AUC ratio was 91%, with 90% CI of 86 to 97%) when DEXILANT was coadministered compared to administration of clopidogrel alone. Pharmacodynamic parameters were also measured and demonstrated that the change in inhibition of platelet aggregation (induced by 5 mcM ADP) was related to the change in the exposure to clopidogrel active metabolite. The effect on exposure to the active metabolite of clopidogrel and on clopidogrel-induced platelet inhibition is not considered clinically important.
Effect of Other Drugs on Dexlansoprazole
Because dexlansoprazole is metabolized by CYP2C19 and CYP3A4, inducers and inhibitors of these enzymes may potentially alter exposure of dexlansoprazole.
12.5. Pharmacogenomics
Effect of CYP2C19 Polymorphism on Systemic Exposure of Dexlansoprazole
Systemic exposure of dexlansoprazole is generally higher in intermediate and poor metabolizers. In male Japanese subjects who received a single dose of DEXILANT 30 or 60 mg (N=2 to 6 subjects/group), mean dexlansoprazole Cmax and AUC values were up to two times higher in intermediate compared to extensive metabolizers; in poor metabolizers, mean Cmax was up to four times higher and mean AUC was up to 12 times higher compared to extensive metabolizers. Though such study was not conducted in Caucasians and African Americans, it is expected dexlansoprazole exposure in these races will be affected by CYP2C19 phenotypes as well.
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
The carcinogenic potential of dexlansoprazole was assessed using lansoprazole studies. In two, 24 month carcinogenicity studies, Sprague-Dawley rats were treated orally with lansoprazole at doses of 5 to 150 mg/kg/day, about one to 40 times the exposure on a body surface (mg/m²) basis of a 50 kg person of average height [1.46 m² body surface area (BSA)] given the recommended human dose of lansoprazole 30 mg/day.
Lansoprazole produced dose-related gastric ECL cell hyperplasia and ECL cell carcinoids in both male and female rats [see Clinical Pharmacology (12.2)].
In rats, lansoprazole also increased the incidence of intestinal metaplasia of the gastric epithelium in both sexes. In male rats, lansoprazole produced a dose-related increase of testicular interstitial cell adenomas. The incidence of these adenomas in rats receiving doses of 15 to 150 mg/kg/day (four to 40 times the recommended human lansoprazole dose based on BSA) exceeded the low background incidence (range = 1.4 to 10%) for this strain of rat.
In a 24 month carcinogenicity study, CD-1 mice were treated orally with lansoprazole doses of 15 to 600 mg/kg/day, two to 80 times the recommended human lansoprazole dose based on BSA. Lansoprazole produced a dose-related increased incidence of gastric ECL cell hyperplasia. It also produced an increased incidence of liver tumors (hepatocellular adenoma plus carcinoma). The tumor incidences in male mice treated with 300 and 600 mg lansoprazole/kg/day (40 to 80 times the recommended human lansoprazole dose based on BSA) and female mice treated with 150 to 600 mg lansoprazole/kg/day (20 to 80 times the recommended human lansoprazole dose based on BSA) exceeded the ranges of background incidences in historical controls for this strain of mice. Lansoprazole treatment produced adenoma of rete testis in male mice receiving 75 to 600 mg/kg/day (10 to 80 times the recommended human lansoprazole dose based on BSA).
A 26 week p53 (+/-) transgenic mouse carcinogenicity study of lansoprazole was not positive.
Lansoprazole was positive in the Ames test and the in vitro human lymphocyte chromosomal aberration assay. Lansoprazole was not genotoxic in the ex vivo rat hepatocyte unscheduled DNA synthesis (UDS) test, the in vivo mouse micronucleus test or the rat bone marrow cell chromosomal aberration test.
Dexlansoprazole was positive in the Ames test and in the in vitro chromosome aberration test using Chinese hamster lung cells. Dexlansoprazole was negative in the in vivo mouse micronucleus test.
The potential effects of dexlansoprazole on fertility and reproductive performance were assessed using lansoprazole studies. Lansoprazole at oral doses up to 150 mg/kg/day (40 times the recommended human lansoprazole dose based on BSA) was found to have no effect on fertility and reproductive performance of male and female rats.
14. Clinical Studies
14.1 Healing of Erosive Esophagitis in Adults
Two multicenter, double-blind, active-controlled, randomized, eight week studies were conducted in patients with endoscopically confirmed EE. Severity of the disease was classified based on the Los Angeles Classification Grading System (Grades A-D). Patients were randomized to one of the following three treatment groups: DEXILANT 60 mg once daily, DEXILANT 90 mg once daily or lansoprazole 30 mg once daily. Patients who were H. pylori positive or who had Barrett’s Esophagus and/or definite dysplastic changes at baseline were excluded from these studies. A total of 4092 patients were enrolled and ranged in age from 18 to 90 years (median age 48 years) with 54% male. Race was distributed as follows: 87% Caucasian, 5% Black and 8% Other. Based on the Los Angeles Classification, 71% of patients had mild EE (Grades A and B) and 29% of patients had moderate to severe EE (Grades C and D) before treatment.
The studies were designed to test noninferiority. If noninferiority was demonstrated then superiority would be tested. Although noninferiority was demonstrated in both studies, the finding of superiority in one study was not replicated in the other.
The proportion of patients with healed EE at Week 4 or 8 is presented below in Table 8.
Table 8. EE Healing Rates* in Adults: All Grades:
| Study | Number of Patients (N)† | Treatment Group (daily) | Week 4 % Healed | Week 8‡ % Healed | (95% CI) for the Treatment Difference (DEXILANT–Lansoprazole) by Week 8 |
|---|---|---|---|---|---|
| 1 | 657 | DEXILANT 60 mg | 70 | 87 | (-1.5, 6.1)§ |
| 648 | Lansoprazole 30 mg | 65 | 85 | ||
| 2 | 639 | DEXILANT 60 mg | 66 | 85 | (2.2, 10.5)§ |
| 656 | Lansoprazole 30 mg | 65 | 79 |
CI = Confidence interval
* Based on crude rate estimates, patients who did not have endoscopically documented healed EE and prematurely discontinued were considered not healed.
† Patients with at least one postbaseline endoscopy.
‡ Primary efficacy endpoint.
§ Demonstrated noninferiority to lansoprazole.
DEXILANT 90 mg once daily was studied and did not provide additional clinical benefit over DEXILANT 60 mg once daily.
14.2 Maintenance of Healed Erosive Esophagitis and Relief of Heartburn in Adults
A multicenter, double-blind, placebo-controlled, randomized study was conducted in patients who successfully completed an EE study and showed endoscopically confirmed healed EE. Maintenance of healing and symptom resolution over a six month period was evaluated with DEXILANT 30 or 60 mg once daily compared to placebo. A total of 445 patients were enrolled and ranged in age from 18 to 85 years (median age 49 years), with 52% female. Race was distributed as follows: 90% Caucasian, 5% Black and 5% Other.
Sixty-six percent of patients treated with 30 mg of DEXILANT remained healed over the six month time period as confirmed by endoscopy (see Table 9).
Table 9. Maintenance Rates* of Healed EE at Month 6 in Adults:
| Number of Patients (N)† | Treatment Group (daily) | Maintenance Rate (%) |
|---|---|---|
| 125 | DEXILANT 30 mg | 66.4‡ |
| 119 | Placebo | 14.3 |
* Based on crude rate estimates, patients who did not have endoscopically documented relapse and prematurely discontinued were considered to have relapsed.
† Patients with at least one postbaseline endoscopy
‡ Statistically significant vs placebo
DEXILANT 60 mg once daily was studied and did not provide additional clinical benefit over DEXILANT 30 mg once daily.
The effect of DEXILANT 30 mg on maintenance of relief of heartburn was also evaluated. Upon entry into the maintenance study, a majority of patients' baseline heartburn severity was rated as none. DEXILANT 30 mg demonstrated a statistically significantly higher percent of 24 hour heartburn-free periods compared to placebo over the six month treatment period (see Table 10). The majority of patients treated with placebo discontinued due to relapse of EE between Month 2 and Month 6.
Table 10. Median Percentage of 24 Hour Heartburn-Free Periods of the Maintenance of Healed EE Study in Adults:
| Overall Treatment* | Month 1 | Month 6 | ||||
|---|---|---|---|---|---|---|
| Treatment Group (daily) | N | Heartburn-Free 24 hour Periods (%) | N | Heartburn-Free 24 hour Periods (%) | N | Heartburn-Free 24 hour Periods (%) |
| DEXILANT 30 mg | 132 | 96.1† | 126 | 96.7 | 80 | 98.3 |
| Placebo | 141 | 28.6 | 117 | 28.6 | 23 | 73.3 |
* Secondary efficacy endpoint
† Statistically significant vs placebo
14.3 Treatment of Symptomatic Non-Erosive GERD in Adults
A multicenter, double-blind, placebo-controlled, randomized, four week study was conducted in patients with a diagnosis of symptomatic non-erosive GERD made primarily by presentation of symptoms. These patients who identified heartburn as their primary symptom, had a history of heartburn for six months or longer, had heartburn on at least four of seven days immediately prior to randomization and had no esophageal erosions as confirmed by endoscopy. However, patients with symptoms which were not acid-related may not have been excluded using these inclusion criteria. Patients were randomized to one of the following treatment groups: DEXILANT 30 mg daily, 60 mg daily, or placebo. A total of 947 patients were enrolled and ranged in age from 18 to 86 years (median age 48 years) with 71% female. Race was distributed as follows: 82% Caucasian, 14% Black and 4% Other.
DEXILANT 30 mg provided statistically significantly greater percent of days with heartburn-free 24 hour periods over placebo as assessed by daily diary over four weeks (see Table 11). DEXILANT 60 mg once daily was studied and provided no additional clinical benefit over DEXILANT 30 mg once daily.
Table 11. Median Percentages of 24 Hour Heartburn-Free Periods During the 4 Week Treatment Period of the Symptomatic Non-Erosive GERD Study in Adults:
| N | Treatment Group (daily) | Heartburn-Free 24 hour Periods (%) |
|---|---|---|
| 312 | DEXILANT 30 mg | 54.9* |
| 310 | Placebo | 18.5 |
* Statistically significant vs placebo
A higher percentage of patients on DEXILANT 30 mg had heartburn-free 24 hour periods compared to placebo as early as the first three days of treatment and this was sustained throughout the treatment period (percentage of patients on Day 3: DEXILANT 38% vs placebo 15%; on Day 28: DEXILANT 63% vs placebo 40%).
14.4 Pediatric GERD
Use of DEXILANT in patients 12 to 17 years of age is supported by evidence from adequate and well-controlled studies of DEXILANT capsules in adults, with additional safety, efficacy, and pharmacokinetic data from studies performed in pediatric patients.
Healing of EE, Maintenance of Healed EE and Relief of Heartburn
In a multicenter, 36 week trial, 62 patients 12 to 17 years of age with a documented history of GERD for at least three months and endoscopically-proven erosive esophagitis (EE) were enrolled to evaluate the healing of EE, maintenance of healed EE and relief of heartburn, followed by an additional 12 weeks without treatment. The median age was 15 years, with males accounting for 61% of the patients. Based on the Los Angeles Classification Grading Scale, 97% of patients had mild EE (Grades A and B), and 3% of patients had moderate to severe EE (Grades C and D) before treatment.
In the first eight weeks, 62 patients were treated with DEXILANT 60 mg once daily to evaluate the healing of EE. Of the 62 patients, 58 patients completed the eight week trial, and 51 (88%) patients achieved healing of EE, as confirmed by endoscopy, over eight weeks of treatment (see Table 12).
Table 12. Healing of EE at Week 8 in Pediatric Patients 12 to 17 Years of Age:
| DEXILANT 60 mg | |
|---|---|
| Proportion of randomized patients healed n (%) | 51/62 (82%) |
| 95% CI | * |
| Proportion of evaluable patients healed† n (%) | 51/58 (88%) |
| 95% CI | (77, 95)* |
* Reported are the exact confidence limits.
† Includes only patients who underwent postbaseline endoscopy.
After the initial eight weeks of treatment, all 51 patients with healed EE were randomized to receive treatment with DEXILANT 30 mg or placebo, once daily for an additional 16 weeks to evaluate maintenance of healing and symptom resolution. Maintenance of healing was assessed by endoscopy at Week 24. Of the 51 patients randomized, 13 patients discontinued early. Of these, five patients did not undergo postbaseline endoscopy. Eighteen of 22 (82%) evaluable patients treated with DEXILANT 30 mg remained healed over the 16 week treatment period as confirmed by endoscopy, compared with 14 of 24 (58%) in placebo (see Table 13).
Table 13. Maintenance of Healed EE at Week 24* in Pediatric Patients 12 to 17 Years of Age:
| DEXILANT 30 mg | Placebo | |
|---|---|---|
| Proportion of randomized patients who maintained healing of EE n (%) | 18/25 (72%) | 14/26 (54%) |
| 95% Cl | (51, 88)† | (33, 73)† |
| Proportion of evaluable patients who maintained healing of EE‡ n (%) | 18/22 (82%) | 14/24 (58%) |
| 95% Cl | (60, 95)† | (37, 78)† |
* Following eight weeks of initial therapy and 16 weeks of maintenance therapy.
† Reported are the exact confidence limits.
‡ Includes patients with at least one postbaseline endoscopy.
Relief of heartburn was assessed in randomized patients during the 16 week maintenance period. The median percentage of 24 hour heartburn-free periods was 87% for those receiving DEXILANT 30 mg compared to 68% for those receiving placebo.
Out of the 32 patients who maintained healing of EE at the end of the 16 week maintenance period, 27 patients (16 treated with DEXILANT and 11 treated with placebo during the double-blind phase) were followed for an additional 12 weeks without therapy. Twenty-four of the 27 patients completed the 12 week follow-up period. One patient required treatment with acid suppression therapy.
Treatment of Symptomatic Non-Erosive GERD
In a single-arm, open-label, multicenter trial, 104 pediatric patients 12 to 17 years of age with symptomatic non-erosive GERD were treated with DEXILANT 30 mg once daily, for four weeks to evaluate safety and effectiveness. Patients had a documented history of GERD symptoms for at least three months prior to screening, reported heartburn on at least three out of seven days during screening, and had no esophageal erosions as confirmed by endoscopy. The median age was 15 years, with females accounting for 70% of the patients. During the four week treatment period, the median percentage of 24 hour heartburn free periods was 47%.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.