EFFEXOR XR Extended-release capsule Ref.[10578] Active ingredients: Venlafaxine
Source: FDA, National Drug Code (US) Revision Year: 2020
4. Contraindications
4.1 Hypersensitivity
Hypersensitivity to venlafaxine hydrochloride, desvenlafaxine succinate or to any excipients in the formulation.
4.2 Concomitant Use with Monoamine Oxidase Inhibitors (MAOIs)
The use of MAOIs (intended to treat psychiatric disorders) concomitantly with Effexor XR or within 7 days of discontinuing treatment with Effexor XR is contraindicated because of an increased risk of serotonin syndrome. The use of Effexor XR within 14 days of discontinuing treatment with an MAOI (intended to treat psychiatric disorders) is also contraindicated [see Dosage and Administration (2.9), Warnings and Precautions (5.2), and Drug Interactions (7.2)].
Starting Effexor XR in a patient who is being treated with an MAOI such as linezolid or intravenous methylene blue is also contraindicated, because of an increased risk of serotonin syndrome [see Dosage and Administration (2.9), Warnings and Precautions (5.2), and Drug Interactions (7.3)].
5. Warnings and Precautions
5.1 Suicidal Thoughts and Behaviors in Children, Adolescents, and Young Adults
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term placebo-controlled studies of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18-24) with MDD and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled studies in children and adolescents with MDD, Obsessive Compulsive Disorder (OCD), or other psychiatric disorders included a total of 24 short-term studies of 9 antidepressant drugs in over 4,400 patients. The pooled analyses of placebo-controlled studies in adults with MDD or other psychiatric disorders included a total of 295 short-term studies (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug versus placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1,000 patients treated) are provided in Table 1.
Table 1. Difference in the Number of Cases of Suicidality per 1,000 Patients Treated versus Placebo:
| Age Range | Increases Compared to Placebo |
|---|---|
| < 18 | 14 additional cases |
| 18–24 | 5 additional cases |
| Decreases Compared to Placebo | |
| 25–64 | 1 fewer case |
| ≥ 65 | 6 fewer cases |
No suicides occurred in any of the pediatric studies. There were suicides in the adult studies, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer term use, i.e., beyond several months. However, there is substantial evidence from placebo-controlled maintenance studies in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for MDD, as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient's presenting symptoms.
If the decision has been made to discontinue treatment, medication should be tapered, as rapidly as is feasible, but with recognition that abrupt discontinuation can be associated with certain symptoms [see Warnings and Precautions (5.7) and Dosage and Administration (2.8)].
Families and caregivers of patients being treated with antidepressants for MDD or other indications, both psychiatric and nonpsychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to healthcare providers. Such monitoring should include daily observation by families and caregivers. Prescriptions for Effexor XR should be written for the smallest quantity of capsules consistent with good patient management, in order to reduce the risk of overdose.
Screening Patients for Bipolar Disorder
A major depressive episode may be the initial presentation of bipolar disorder. It is generally believed (though not established in controlled studies) that treating such an episode with an antidepressant alone may increase the likelihood of precipitation of a mixed/manic episode in patients at risk for bipolar disorder. Whether any of the symptoms described above represent such a conversion is unknown. However, prior to initiating treatment with an antidepressant, patients with depressive symptoms should be adequately screened to determine if they are at risk for bipolar disorder; such screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression. It should be noted that Effexor XR is not approved for use in treating bipolar depression.
5.2 Serotonin Syndrome
The development of a potentially life-threatening serotonin syndrome has been reported with SNRIs and SSRIs, including Effexor XR alone, but particularly with concomitant use of other serotonergic drugs (including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, buspirone, amphetamines, and St. John's wort) and with drugs that impair metabolism of serotonin in particular, MAOIs, both those intended to treat psychiatric disorders and others, such as linezolid or intravenous methylene blue).
Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, delirium, coma) autonomic instability (e.g., tachycardia, labile blood pressure, hyperthermia, diaphoresis, flushing, and dizziness), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination); seizures and gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Patients should be monitored for the emergence of serotonin syndrome.
The concomitant use of Effexor XR with MAOIs (intended to treat psychiatric disorders) is contraindicated. Effexor XR should also not be started in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue. All reports with methylene blue that provided information on the route of administration involved intravenous administration in the dose range of 1 mg/kg to 8 mg/kg. No reports involved the administration of methylene blue by other routes (such as oral tablets or local tissue injection) or at lower doses. There may be circumstances when it is necessary to initiate treatment with a MAOI such as linezolid or intravenous methylene blue in a patient taking Effexor XR. Effexor XR should be discontinued before initiating treatment with the MAOI [see Contraindications (4.2), Dosage and Administration (2.6), and Drug Interactions (7.3)].
If concomitant use of Effexor XR with other serotonergic drugs (e.g., triptans, tricyclic antidepressants, mirtazapine, fentanyl, lithium, tramadol, buspirone, amphetamines, tryptophan, or St. John's wort) is clinically warranted, careful observation of the patient is advised, particularly during treatment initiation and dose increases [see Drug Interactions (7.3)]. Patients should be made aware of the potential risk of serotonin syndrome. Treatment with Effexor XR and any concomitant serotonergic agents should be discontinued immediately if the above events occur, and supportive symptomatic treatment should be initiated.
5.3 Elevations in Blood Pressure
In controlled trials, there were dose-related increases in systolic and diastolic blood pressure, as well as cases of sustained hypertension [see Adverse Reactions (6.2)].
Monitor blood pressure before initiating treatment with Effexor XR and regularly during treatment. Control pre-existing hypertension before initiating treatment with Effexor XR. Use caution in treating patients with pre-existing hypertension or cardiovascular or cerebrovascular conditions that might be compromised by increases in blood pressure. Sustained blood pressure elevation can lead to adverse outcomes. Cases of elevated blood pressure requiring immediate treatment have been reported with Effexor XR. Consider dose reduction or discontinuation of treatment for patients who experience a sustained increase in blood pressure.
Across all clinical studies with Effexor, 1.4% of patients in the Effexor XR treated groups experienced a ≥15 mm Hg increase in supine diastolic blood pressure (SDBP) ≥105 mm Hg, compared to 0.9% of patients in the placebo groups. Similarly, 1% of patients in the Effexor XR treated groups experienced a ≥20 mm Hg increase in supine systolic blood pressure (SSBP) with blood pressure ≥180 mm Hg, compared to 0.3% of patients in the placebo groups [see Table 10 in Adverse Reactions (6.2)]. Effexor XR treatment was associated with sustained hypertension (defined as treatment-emergent SDBP ≥90 mm Hg and ≥10 mm Hg above baseline for three consecutive on-therapy visits [see Table 11 in Adverse Reactions (6.2)]. An insufficient number of patients received mean doses of Effexor XR over 300 mg per day in clinical studies to fully evaluate the incidence of sustained increases in blood pressure at these higher doses.
5.4 Abnormal Bleeding
SSRIs and SNRIs, including Effexor XR, may increase the risk of bleeding events, ranging from ecchymoses, hematomas, epistaxis, petechiae, and gastrointestinal hemorrhage to life-threatening hemorrhage. Concomitant use of aspirin, Nonsteroidal Anti-Inflammatory Drugs (NSAIDs), warfarin, and other anti-coagulants or other drugs known to affect platelet function may add to this risk. Case reports and epidemiological studies (case-control and cohort design) have demonstrated an association between use of drugs that interfere with serotonin reuptake and the occurrence of gastrointestinal bleeding. Caution patients about the risk of bleeding associated with the concomitant use of Effexor XR and NSAIDs, aspirin, or other drugs that affect coagulation.
5.5 Angle-Closure Glaucoma
The pupillary dilation that occurs following use of many antidepressant drugs including Effexor XR may trigger an angle closure attack in a patient with anatomically narrow angles who does not have a patent iridectomy.
5.6 Activation of Mania / Hypomania
Mania or hypomania was reported in Effexor XR treated patients in the premarketing studies in MDD, SAD, and PD (see Table 2). Mania/hypomania has also been reported in a small proportion of patients with mood disorders who were treated with other marketed drugs to treat MDD. Effexor XR should be used cautiously in patients with a history of mania or hypomania.
Table 2. Incidence (%) of Mania or Hypomania Reported in Effexor XR Treated Patients in the Premarketing Studies:
| Indication | Effexor XR | Placebo |
|---|---|---|
| MDD | 0.3 | 0.0 |
| GAD | 0.0 | 0.2 |
| SAD | 0.2 | 0.0 |
| PD | 0.1 | 0.0 |
5.7 Discontinuation Syndrome
Discontinuation symptoms have been systematically evaluated in patients taking venlafaxine, including prospective analyses of clinical studies in GAD and retrospective surveys of studies in MDD and SAD. Abrupt discontinuation or dose reduction of venlafaxine at various doses has been found to be associated with the appearance of new symptoms, the frequency of which increased with increased dose level and with longer duration of treatment. Reported symptoms include agitation, anorexia, anxiety, confusion, impaired coordination and balance, diarrhea, dizziness, dry mouth, dysphoric mood, fasciculation, fatigue, flu-like symptoms, headaches, hypomania, insomnia, nausea, nervousness, nightmares, sensory disturbances (including shock-like electrical sensations), somnolence, sweating, tremor, vertigo, and vomiting.
During marketing of Effexor XR, other SNRIs, and SSRIs, there have been spontaneous reports of adverse events occurring upon discontinuation of these drugs, particularly when abrupt, including the following: dysphoric mood, irritability, agitation, dizziness, sensory disturbances (e.g., paresthesia, such as electric shock sensations), anxiety, confusion, headache, lethargy, emotional lability, insomnia, hypomania, tinnitus, and seizures. While these events are generally self-limiting, there have been reports of serious discontinuation symptoms.
Patients should be monitored for these symptoms when discontinuing treatment with Effexor XR. A gradual reduction in the dose, rather than abrupt cessation, is recommended whenever possible. If intolerable symptoms occur following a decrease in the dose or upon discontinuation of treatment, then resuming the previously prescribed dose may be considered. Subsequently, the physician may continue decreasing the dose, but at a more gradual rate [see Dosage and Administration (2.8)].
5.8 Seizures
Seizures have occurred with venlafaxine therapy. Effexor XR, like many antidepressants, should be used cautiously in patients with a history of seizures and should be discontinued in any patient who develops seizures [Must mitigate the risk: Risk factors, concomitant meds that lower the seizure threshold].
5.9 Hyponatremia
Hyponatremia can occur as a result of treatment with SSRIs and SNRIs, including Effexor XR. In many cases, the hyponatremia appears to be the result of the Syndrome of Inappropriate Antidiuretic Hormone (SIADH) secretion. Cases with serum sodium lower than 110 mmol/L have been reported. Elderly patients may be at greater risk of developing hyponatremia with SSRIs and SNRIs [see Use in Specific Populations (8.5)]. Also, patients taking diuretics, or those who are otherwise volume-depleted, may be at greater risk. Consider discontinuation of Effexor XR in patients with symptomatic hyponatremia, and institute appropriate medical intervention.
Signs and symptoms of hyponatremia include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which may lead to falls. Signs and symptoms associated with more severe and/or acute cases have included hallucination, syncope, seizure, coma, respiratory arrest, and death.
5.10 Weight and Height Changes in Pediatric Patients
Weight Changes
The average change in body weight and incidence of weight loss (percentage of patients who lost 3.5% or more) in the placebo-controlled pediatric studies in MDD, GAD, and SAD are shown in Tables 3 and 4.
Table 3. Average Change in Body Weight (kg) From Beginning of Treatment in Pediatric Patients in Double-blind, Placebo-controlled Studies of Effexor XR:
| Indication (Duration) | Effexor XR | Placebo |
|---|---|---|
| MDD and GAD (4 pooled studies, 8 weeks) | -0.45 (n = 333) | +0.77 (n = 333) |
| SAD (16 weeks) | -0.75 (n = 137) | +0.76 (n = 148) |
Table 4. Incidence ==(%)== of Pediatric Patients Experiencing Weight Loss (3.5% or more) in Double-blind, Placebo-controlled Studies of Effexor XR:
| Indication (Duration) | Effexor XR | Placebo |
|---|---|---|
| MDD and GAD (4 pooled studies, 8 weeks) | 18* (n = 333) | 3.6 (n = 333) |
| SAD (16 weeks) | 47* (n = 137) | 14 (n = 148) |
* p <0.001 versus placebo
Weight loss was not limited to patients with treatment-emergent anorexia [see Warnings and Precautions (5.11)].
The risks associated with longer term Effexor XR use were assessed in an open-label MDD study of children and adolescents who received Effexor XR for up to six months. The children and adolescents in the study had increases in weight that were less than expected, based on data from age- and sex-matched peers. The difference between observed weight gain and expected weight gain was larger for children (<12 years old) than for adolescents (≥12 years old).
Height Changes
Table 5 shows the average height increase in pediatric patients in the short-term, placebo-controlled MDD, GAD, and SAD studies. The differences in height increases in GAD and MDD studies were most notable in patients younger than twelve.
Table 5. Average Height Increases (cm) in Pediatric Patients in Placebo-controlled Studies of Effexor XR:
| Indication (Duration) | Effexor XR | Placebo |
|---|---|---|
| MDD (8 weeks) | 0.8 (n = 146) | 0.7 (n = 147) |
| GAD (8 weeks) | 0.3 ?footnote? (n = 122) | 1.0 (n = 132) |
| SAD (16 weeks) | 1.0 (n = 109) | 1.0 (n = 112) |
In the six-month, open-label MDD study, children and adolescents had height increases that were less than expected, based on data from age- and sex-matched peers. The difference between observed and expected growth rates was larger for children (<12 years old) than for adolescents (≥12 years old).
5.11 Appetite Changes in Pediatric Patients
Decreased appetite (reported as treatment-emergent anorexia) was more commonly observed in Effexor XR treated patients versus placebo-treated patients in the premarketing evaluation of Effexor XR for MDD, GAD, and SAD (see Table 6).
Table 6. Incidence (%) of Decreased Appetite and Associated Discontinuation Rates* (%) in Pediatric Patients in Placebo-controlled Studies of Effexor XR:
| Indication (Duration) | Effexor XR Incidence | Discontinuation | Placebo Incidence | Discontinuation |
|---|---|---|---|---|
| MDD and GAD (pooled, 8 weeks) | 10 | 0.0 | 3 | – |
| SAD (16 weeks) | 22 | 0.7 | 3 | 0.0 |
* The discontinuation rates for weight loss were 0.7% for patients receiving either Effexor XR or placebo.
5.12 Interstitial Lung Disease and Eosinophilic Pneumonia
Interstitial lung disease and eosinophilic pneumonia associated with venlafaxine therapy have been rarely reported. The possibility of these adverse events should be considered in venlafaxine-treated patients who present with progressive dyspnea, cough or chest discomfort. Such patients should undergo a prompt medical evaluation, and discontinuation of venlafaxine therapy should be considered.
6. Adverse Reactions
The following adverse reactions are discussed in greater detail in other sections of the label:
- Hypersensitivity [see Contraindications (4.1)]
- Suicidal Thoughts and Behaviors in Children, Adolescents, and Adults [see Warnings and Precautions (5.1)]
- Serotonin Syndrome [see Warnings and Precautions (5.2)]
- Elevations in Blood Pressure [see Warnings and Precautions (5.3)]
- Abnormal Bleeding [see Warnings and Precautions (5.4)]
- Angle Closure Glaucoma [see Warnings and Precautions (5.5)]
- Activation of Mania/Hypomania [see Warnings and Precautions (5.6)]
- Discontinuation Syndrome [see Warnings and Precautions (5.7)]
- Seizure [see Warnings and Precautions (5.8)]
- Hyponatremia [see Warnings and Precautions (5.9)]
- Weight and Height changes in Pediatric Patients [see Warnings and Precautions (5.10)]
- Appetite Changes in Pediatric Patients [see Warnings and Precautions (5.11)]
- Interstitial Lung Disease and Eosinophilic Pneumonia [see Warnings and Precautions (5.12)]
6.1. Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
Most Common Adverse Reactions
The most commonly observed adverse reactions in the clinical study database in Effexor XR treated patients in MDD, GAD, SAD, and PD (incidence ≥5% and at least twice the rate of placebo) were: nausea (30.0%), somnolence (15.3%), dry mouth (14.8%), sweating (11.4%), abnormal ejaculation (9.9%), anorexia (9.8%), constipation (9.3%), impotence (5.3%) and decreased libido (5.1%).
Adverse Reactions Reported as Reasons for Discontinuation of Treatment
Combined across short-term, placebo-controlled premarketing studies for all indications, 12% of the 3,558 patients who received Effexor XR (37.5-225 mg) discontinued treatment due to an adverse experience, compared with 4% of the 2,197 placebo-treated patients in those studies.
The most common adverse reactions leading to discontinuation in ≥1% of the Effexor XR treated patients in the short-term studies (up to 12 weeks) across indications are shown in Table 7.
Table 7. Incidence (%) of Patients Reporting Adverse Reactions Leading to Discontinuation in Placebo-controlled Clinical Studies (up to 12 Weeks Duration):
| Body System Adverse Reaction | Effexor XR n = 3,558 | Placebo n = 2,197 |
|---|---|---|
| Body as a whole | ||
| Asthenia | 1.7 | 0.5 |
| Headache | 1.5 | 0.8 |
| Digestive system | ||
| Nausea | 4.3 | 0.4 |
| Nervous system | ||
| Dizziness | 2.2 | 0.8 |
| Insomnia | 2.1 | 0.6 |
| Somnolence | 1.7 | 0.3 |
| Skin and appendages | 1.5 | 0.6 |
| Sweating | 1.0 | 0.2 |
Common Adverse Reactions in Placebo-controlled Studies
The number of patients receiving multiple doses of Effexor XR during the premarketing assessment for each approved indication is shown in Table 8. The conditions and duration of exposure to venlafaxine in all development programs varied greatly, and included (in overlapping categories) open and double-blind studies, uncontrolled and controlled studies, inpatient (Effexor only) and outpatient studies, fixed-dose, and titration studies.
Table 8. Patients Receiving Effexor XR in Premarketing Clinical Studies:
| Indication | Effexor XR |
|---|---|
| MDD | 705* |
| GAD | 1,381 |
| SAD | 819 |
| PD | 1,314 |
* In addition, in the premarketing assessment of Effexor, multiple doses were administered to 2,897 patients in studies for MDD
The incidences of common adverse reactions (those that occurred in ≥2% of Effexor XR treated patients [357 MDD patients, 1,381 GAD patients, 819 SAD patients, and 1,001 PD patients] and more frequently than placebo) in Effexor XR treated patients in short-term, placebo-controlled, fixed- and flexible-dose clinical studies (doses 37.5 to 225 mg per day) are shown in Table 9.
The adverse reaction profile did not differ substantially between the different patient populations.
Table 9. Common Adverse Reactions: Percentage of Patients Reporting Adverse Reactions (≥2% and > placebo) in Placebo-controlled Studies (up to 12 Weeks Duration) across All Indications:
| Body System Adverse Reaction | Effexor XR n = 3,558 | Placebo n = 2,197 |
|---|---|---|
| Body as a whole | ||
| Asthenia | 12.6 | 7.8 |
| Cardiovascular system | ||
| Hypertension | 3.4 | 2.6 |
| Palpitation | 2.2 | 2.0 |
| Vasodilatation | 3.7 | 1.9 |
| Digestive system | ||
| Anorexia | 9.8 | 2.6 |
| Constipation | 9.3 | 3.4 |
| Diarrhea | 7.7 | 7.2 |
| Dry mouth | 14.8 | 5.3 |
| Nausea | 30.0 | 11.8 |
| Vomiting | 4.3 | 2.7 |
| Nervous system | ||
| Abnormal dreams | 2.9 | 1.4 |
| Dizziness | 15.8 | 9.5 |
| Insomnia | 17.8 | 9.5 |
| Libido decreased | 5.1 | 1.6 |
| Nervousness | 7.1 | 5.0 |
| Paresthesia | 2.4 | 1.4 |
| Somnolence | 15.3 | 7.5 |
| Tremor | 4.7 | 1.6 |
| Respiratory system | ||
| Yawn | 3.7 | 0.2 |
| Skin and appendages | ||
| Sweating (including night sweats) | 11.4 | 2.9 |
| Special senses | ||
| Abnormal vision | 4.2 | 1.6 |
| Urogenital system | ||
| Abnormal ejaculation/orgasm (men)* | 9.9 | 0.5 |
| Anorgasmia (men)* | 3.6 | 0.1 |
| Anorgasmia (women)† | 2.0 | 0.2 |
| Impotence (men)* | 5.3 | 1.0 |
* Percentages based on the number of men (Effexor XR, n = 1,4 4 0; placebo, n = 923)
† Percentages based on the number of women (Effexor XR, n = 2,118; placebo, n = 1,274)
Other Adverse Reactions Observed in Clinical Studies
Body as a whole – Photosensitivity reaction, chills
Cardiovascular system – Postural hypotension, syncope, hypotension, tachycardia
Digestive system – Gastrointestinal hemorrhage [see Warnings and Precautions (5.4)], bruxism
Hemic/Lymphatic system – Ecchymosis [see Warnings and Precautions (5.4)]
Metabolic/Nutritional – Hypercholesterolemia, weight gain [see Warnings and Precautions (5.10)], weight loss [see Warnings and Precautions (5.10)]
Nervous system – Seizures [see Warnings and Precautions (5.8)], manic reaction [see Warnings and Precautions (5.6)], agitation, confusion, akathisia, hallucinations, hypertonia, myoclonus, depersonalization, apathy
Skin and appendages – Urticaria, pruritus, rash, alopecia
Special senses – Mydriasis, abnormality of accommodation, tinnitus, taste perversion
Urogenital system – Urinary retention, urination impaired, urinary incontinence, urinary frequency increased, menstrual disorders associated with increased bleeding or increased irregular bleeding (e.g., menorrhagia, metrorrhagia)
6.2 Vital Sign Changes
In placebo-controlled premarketing studies, there were increases in mean blood pressure (see Table 10). Across most indications, a dose-related increase in mean supine systolic and diastolic blood pressure was evident in patients treated with Effexor XRs. Across all clinical studies in MDD, GAD, SAD and PD, 1.4% of patients in the Effexor XR groups experienced an increase in SDBP of ≥15 mm Hg along with a blood pressure ≥105 mm Hg, compared to 0.9% of patients in the placebo groups. Similarly, 1% of patients in the Effexor XR groups experienced an increase in SSBP of ≥20 mm Hg with a blood pressure ≥180 mm Hg, compared to 0.3% of patients in the placebo groups.
Table 10. Final On-therapy Mean Changes From Baseline in Supine Systolic (SSBP) and Diastolic (SDBP) Blood Pressure (mm Hg) in Placebo-controlled Studies:
| Effexor XR | Placebo | |||||
|---|---|---|---|---|---|---|
| Indication | ≤ 75 mg per day | > 75 mg per day | ||||
| (Duration) | SSBP | SDBP | SSBP | SDBP | SSBP | SDBP |
| MDD | ||||||
| (8–12 weeks) | -0.28 | 0.37 | 2.93 | 3.56 | -1.08 | -0.10 |
| GAD | ||||||
| (8 weeks) | -0.28 | 0.02 | 2.40 | 1.68 | -1.26 | -0.92 |
| (6 months) | 1.27 | -0.69 | 2.06 | 1.28 | -1.29 | -0.74 |
| SAD | ||||||
| (12 weeks) | -0.29 | -1.26 | 1.18 | 1.34 | -1.96 | -1.22 |
| (6 months) | -0.98 | -0.49 | 2.51 | 1.96 | -1.84 | -0.65 |
| PD | ||||||
| (10–12 weeks) | -1.15 | 0.97 | -0.36 | 0.16 | -1.29 | -0.99 |
Effexor XR treatment was associated with sustained hypertension (defined as treatment-emergent Supine Diastolic Blood Pressure [SDBP] ≥90 mm Hg and ≥10 mm Hg above baseline for three consecutive on-therapy visits (see Table 11). An insufficient number of patients received mean doses of Effexor XR over 300 mg per day in clinical studies to fully evaluate the incidence of sustained increases in blood pressure at these higher doses.
Table 11. Sustained Elevations in SDBP in Effexor XR Premarketing Studies:
| Indication | Dose Range (mg per day) | Incidence (%) |
|---|---|---|
| MDD | 75-375 | 19/705 (3) |
| GAD | 37.5-225 | 5/1011 (0.5) |
| SAD | 75-225 | 5/771 (0.6) |
| PD | 75-225 | 9/973 (0.9) |
Effexor XR was associated with mean increases in pulse rate compared with placebo in premarketing placebo-controlled studies (see Table 12) [see Warnings and Precautions (5.3, 5.4)].
Table 12. Approximate Mean Final On-therapy Increase in Pulse Rate (beats/min) in Effexor XR Premarketing Placebo-controlled Studies (up to 12 Weeks Duration):
| Indication (Duration) | Effexor XR | Placebo |
|---|---|---|
| MDD (12 weeks) | 2 | 1 |
| GAD (8 weeks) | 2 | < 1 |
| SAD (12 weeks) | 3 | 1 |
| PD (12 weeks) | 1 | < 1 |
6.3 Laboratory Changes
Serum Cholesterol
Effexor XR was associated with mean final increases in serum cholesterol concentrations compared with mean final decreases for placebo in premarketing MDD, GAD, SAD and PD clinical studies (Table 13).
Table 13. Mean Final On-therapy Changes in Cholesterol Concentrations (mg/dL) in Effexor XR Premarketing Studies:
| Indication (Duration) | Effexor XR | Placebo |
|---|---|---|
| MDD | ||
| (12 weeks) | +1.5 | -7.4 |
| GAD | ||
| (8 weeks) | +1.0 | -4.9 |
| (6 months) | +2.3 | -7.7 |
| SAD | ||
| (12 weeks) | +7.9 | -2.9 |
| (6 months) | +5.6 | -4.2 |
| PD | ||
| (12 weeks) | 5.8 | -3.7 |
Effexor XR (venlafaxine hydrochloride) extended-release capsules treatment for up to 12 weeks in premarketing placebo-controlled trials for major depressive disorder was associated with a mean final on-therapy increase in serum cholesterol concentration of approximately 1.5 mg/dL compared with a mean final decrease of 7.4 mg/dL for placebo. Effexor XR treatment for up to 8 weeks and up to 6 months in premarketing placebo-controlled GAD trials was associated with mean final on-therapy increases in serum cholesterol concentration of approximately 1.0 mg/dL and 2.3 mg/dL, respectively while placebo subjects experienced mean final decreases of 4.9 mg/dL and 7.7 mg/dL, respectively. Effexor XR treatment for up to 12 weeks and up to 6 months in premarketing placebo-controlled Social Anxiety Disorder trials was associated with mean final on-therapy increases in serum cholesterol concentration of approximately 7.9 mg/dL and 5.6 mg/dL, respectively, compared with mean final decreases of 2.9 and 4.2 mg/dL, respectively, for placebo. Effexor XR treatment for up to 12 weeks in premarketing placebo-controlled panic disorder trials was associated with mean final on-therapy increases in serum cholesterol concentration of approximately 5.8 mg/dL compared with a mean final decrease of 3.7 mg/dL for placebo.
Patients treated with Effexor (immediate release) for at least 3 months in placebo-controlled 12-month extension trials had a mean final on-therapy increase in total cholesterol of 9.1 mg/dL compared with a decrease of 7.1 mg/dL among placebo-treated patients. This increase was duration dependent over the study period and tended to be greater with higher doses. Clinically relevant increases in serum cholesterol, defined as 1) a final on-therapy increase in serum cholesterol ≥50 mg/dL from baseline and to a value ≥261 mg/dL, or 2) an average on-therapy increase in serum cholesterol ≥50 mg/dL from baseline and to a value ≥261 mg/dL, were recorded in 5.3% of venlafaxine-treated patients and 0.0% of placebo-treated patients.
Serum Triglycerides
Effexor XR was associated with mean final on-therapy increases in fasting serum triglycerides compared with placebo in premarketing clinical studies of SAD and PD up to 12 weeks (pooled data) and 6 months duration (Table 14).
Table 14. Mean Final On-therapy Increases in Triglyceride Concentrations (mg/dL) in Effexor XR Premarketing Studies:
| Indication (Duration) | Effexor XR | Placebo |
|---|---|---|
| SAD (12 weeks) | 8.2 | 0.4 |
| SAD (6 months) | 11.8 | 1.8 |
| PD (12 weeks) | 5.9 | 0.9 |
| PD (6 months) | 9.3 | 0.3 |
6.4 Pediatric Patients
In general, the adverse reaction profile of venlafaxine (in placebo-controlled clinical studies) in children and adolescents (ages 6 to 17) was similar to that seen for adults. As with adults, decreased appetite, weight loss, increased blood pressure, and increased serum cholesterol were observed [see Warnings and Precautions (5.3, 5.10, 5.11) and Use in Specific Populations (8.4)].
In pediatric clinical studies, the adverse reaction, suicidal ideation, was observed.
Particularly, the following adverse reactions were observed in pediatric patients: abdominal pain, agitation, dyspepsia, ecchymosis, epistaxis, and myalgia.
6.5 Adverse Reactions Identified During Postapproval Use
The following adverse reactions have been identified during postapproval use of Effexor XR. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure:
Body as a whole – Anaphylaxis, angioedema
Cardiovascular system – QT prolongation, ventricular fibrillation, ventricular tachycardia (including torsade de pointes), takotsubo cardiomyopathy
Digestive system – Pancreatitis
Hemic/Lymphatic system – Mucous membrane bleeding [see Warnings and Precautions (5.4)], blood dyscrasias (including agranulocytosis, aplastic anemia, neutropenia and pancytopenia), prolonged bleeding time, thrombocytopenia
Metabolic/Nutritional – Hyponatremia [see Warnings and Precautions (5.9)], Syndrome of Inappropriate Antidiuretic Hormone (SIADH) secretion [see Warnings and Precautions (5.9)], abnormal liver function tests, hepatitis, prolactin increased
Musculoskeletal – Rhabdomyolysis
Nervous system – Neuroleptic Malignant Syndrome (NMS) [see Warnings and Precautions (5.2)], serotonergic syndrome [see Warnings and Precautions (5.2)], delirium, extrapyramidal reactions (including dystonia and dyskinesia), impaired coordination and balance, tardive dyskinesia
Respiratory system – Dyspnea, interstitial lung disease, pulmonary eosinophilia [see Warnings and Precautions (5.12)]
Skin and appendages – Stevens-Johnson syndrome, toxic epidermal necrolysis, erythema multiforme
Special senses – Angle-closure glaucoma [see Warnings and Precautions (5.5)]
7. Drug Interactions
7.1 Central Nervous System (CNS)-Active Drugs
The risk of using venlafaxine in combination with other CNS-active drugs has not been systematically evaluated. Consequently, caution is advised when Effexor XR is taken in combination with other CNS-active drugs.
7.2 Monoamine Oxidase Inhibitors
Adverse reactions, some of which were serious, have been reported in patients who have recently been discontinued from an MAOI and started on antidepressants with pharmacological properties similar to Effexor XR (SNRIs or SSRIs), or who have recently had SNRI or SSRI therapy discontinued prior to initiation of an MAOI [see Dosage and Administration (2.9), Contraindications (4.2) and Warnings and Precautions (5.2)].
7.3 Serotonergic Drugs
Based on the mechanism of action of Effexor XR and the potential for serotonin syndrome, caution is advised when Effexor XR is coadministered with other drugs that may affect the serotonergic neurotransmitter systems, such as triptans, SSRIs, other SNRIs, linezolid (an antibiotic which is a reversible non-selective MAOI), lithium, tramadol, or St. John's wort. If concomitant treatment with Effexor XR and these drugs is clinically warranted, careful observation of the patient is advised, particularly during treatment initiation and dose increases. The concomitant use of Effexor XR with tryptophan supplements is not recommended [see Dosage and Administration (2.9), Contraindications (4.2), and Warnings and Precautions (5.2)].
7.4 Drugs that Interfere with Hemostasis (e.g., NSAIDs, Aspirin, and Warfarin)
Serotonin release by platelets plays an important role in hemostasis. The use of psychotropic drugs that interfere with serotonin reuptake is associated with the occurrence of upper gastrointestinal bleeding and concurrent use of an NSAID or aspirin may potentiate this risk of bleeding [see Warnings and Precautions (5.4)]. Altered anticoagulant effects, including increased bleeding, have been reported when SSRIs and SNRIs are coadministered with warfarin. Patients receiving warfarin therapy should be carefully monitored when Effexor XR is initiated or discontinued.
7.5 Weight Loss Agents
The safety and efficacy of venlafaxine therapy in combination with weight loss agents, including phentermine, have not been established. Coadministration of Effexor XR and weight loss agents is not recommended. Effexor XR is not indicated for weight loss alone or in combination with other products.
7.6 Effects of Other Drugs on Effexor XR
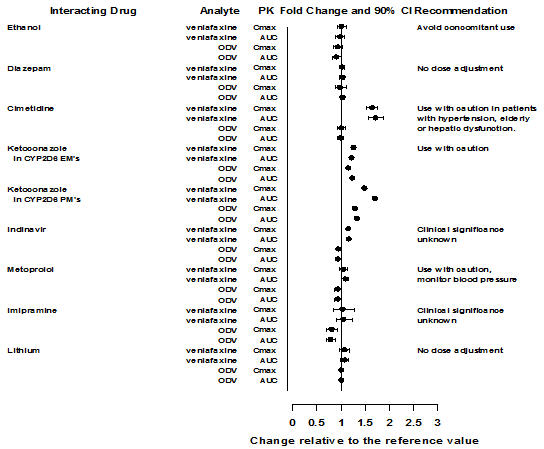
Figure 1. Effect of interacting drugs on the pharmacokinetics of venlafaxine and active metabolite O-desmethylvenlafaxine (ODV):
Abbreviations: ODV, O-desmethylvenlafaxine; AUC, area under the curve; Cmax, peak plasma concentrations; EM's, extensive metabolizers; PM's, poor metabolizers
* No dose adjustment on co-administration with CYP2D6 inhibitors (Fig 3 and Metabolism Section 12.3)
7.7 Effects of Effexor XR on Other Drugs
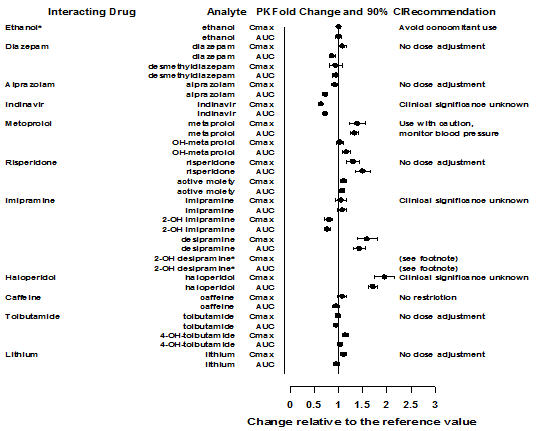
Figure 2. Effect of venlafaxine on the pharmacokinetics interacting drugs and their active metabolites:
Abbreviations: AUC, area under the curve; Cmax, peak plasma concentrations; OH, hydroxyl
* Data for 2-OH desipramine were not plotted to enhance clarity; the fold change and 90% CI for Cmax and AUC of 2-OH desipramine were 6.6 (5.5, 7.9) and 4.4 (3.8, 5.0), respectively.
Note:
*: Administration of venlafaxine in a stable regimen did not exaggerate the psychomotor and psychometric effects induced by ethanol in these same subjects when they were not receiving venlafaxine.
7.8 Drug-Laboratory Test Interactions
False-positive urine immunoassay screening tests for phencyclidine (PCP) and amphetamine have been reported in patients taking venlafaxine. This is due to lack of specificity of the screening tests. False positive test results may be expected for several days following discontinuation of venlafaxine therapy. Confirmatory tests, such as gas chromatography/mass spectrometry, will distinguish venlafaxine from PCP and amphetamine.
8.1. Pregnancy
Teratogenic Effects – Pregnancy Category C
Venlafaxine did not cause malformations in offspring of rats or rabbits given doses up to 2.5 times (rat) or 4 times (rabbit) the maximum recommended human daily dose on a mg/m2 basis. However, in rats, there was a decrease in pup weight, an increase in stillborn pups, and an increase in pup deaths during the first 5 days of lactation, when dosing began during pregnancy and continued until weaning. The cause of these deaths is not known. These effects occurred at 2.5 times (mg/m2) the maximum human daily dose. The no effect dose for rat pup mortality was 0.25 times the human dose on a mg/m2 basis. In reproductive developmental studies in rats and rabbits with O-desmethylvenlafaxine (ODV), the major human metabolite of venlafaxine, evidence of teratogenicity was not observed at exposure margins of 13 in rats and 0.3 in rabbits. There are no adequate and well-controlled studies in pregnant women. Effexor XR should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Non-teratogenic Effects
Neonates exposed to Effexor XR, other SNRIs, or SSRIs, late in the third trimester have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding. Such complications can arise immediately upon delivery. Reported clinical findings have included respiratory distress, cyanosis, apnea, seizures, temperature instability, feeding difficulty, vomiting, hypoglycemia, hypotonia, hypertonia, hyperreflexia, tremor, jitteriness, irritability, and constant crying. These features are consistent with either a direct toxic effect of SSRIs and SNRIs, or possibly a drug discontinuation syndrome. It should be noted, that in some cases the clinical picture is consistent with serotonin syndrome [see Warnings and Precautions (5.2) and Drug Interactions (7.3)]. When treating a pregnant woman with Effexor XR during the third trimester, the physician should carefully consider the potential risks and benefits of treatment.
8.2. Labor and Delivery
The effect of venlafaxine on labor and delivery in humans is unknown.
8.3. Nursing Mothers
Venlafaxine and ODV have been reported to be excreted in human milk. Because of the potential for serious adverse reactions in nursing infants from Effexor XR, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4. Pediatric Use
Two placebo-controlled trials in 766 pediatric patients with MDD and two placebo-controlled trials in 793 pediatric patients with GAD have been conducted with Effexor XR, and the data were not sufficient to support a claim for use in pediatric patients.
Anyone considering the use of Effexor XR in a child or adolescent must balance the potential risks with the clinical need [see Boxed Warning, Warnings and Precautions (5.1, 5.10, 5.11) and Adverse Reactions (6.4)].
Although no studies have been designed to primarily assess Effexor XR's impact on the growth, development, and maturation of children and adolescents, the studies that have been done suggest that Effexor XR may adversely affect weight and height [see Warnings and Precautions (5.10)]. Should the decision be made to treat a pediatric patient with Effexor XR, regular monitoring of weight and height is recommended during treatment, particularly if treatment is to be continued long-term [see Warnings and Precautions (5.10, 5.11)]. The safety of Effexor XR treatment for pediatric patients has not been systematically assessed for chronic treatment longer than six months in duration. In the studies conducted in pediatric patients (ages 6-17), the occurrence of blood pressure and cholesterol increases considered to be clinically relevant in pediatric patients was similar to that observed in adult patients. Consequently, the precautions for adults apply to pediatric patients [see Warnings and Precautions (5.3, 6.3)].
8.5. Geriatric Use
The percentage of patients in clinical studies for Effexor XR for MDD, GAD, SAD, and PD who were 65 years of age or older are shown in Table 15.
Table 15. Percentage (and Number of Patients Studied) of Patients 65 Years of Age and Older by Indication*:
| Indication | Effexor XR |
|---|---|
| MDD | 4 (14/357) |
| GAD | 6 (77/1,381) |
| SAD | 1 (10/819) |
| PD | 2 (16/1,001) |
* In addition, in the premarketing assessment of Effexor (immediate release), 12% (357/2,897) of patients were ≥65 years of age.
No overall differences in effectiveness or safety were observed between geriatric patients and younger patients, and other reported clinical experience generally has not identified differences in response between the elderly and younger patients. However, greater sensitivity of some older individuals cannot be ruled out. SSRIs and SNRIs, including Effexor XR, have been associated with cases of clinically significant hyponatremia in elderly patients, who may be at greater risk for this adverse event [see Warnings and Precautions (5.9)].
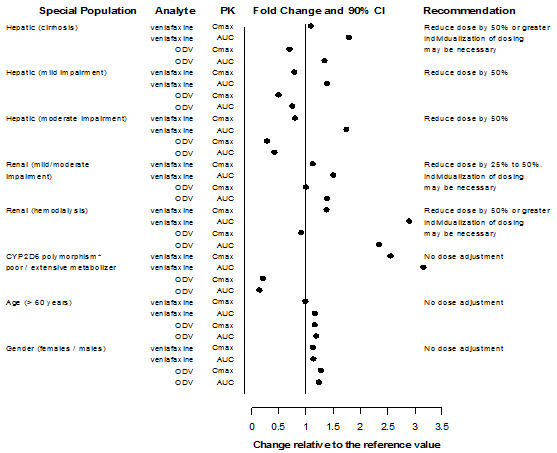
The pharmacokinetics of venlafaxine and ODV are not substantially altered in the elderly [see Clinical Pharmacology (12.3)] (see Figure 3). No dose adjustment is recommended for the elderly on the basis of age alone, although other clinical circumstances, some of which may be more common in the elderly, such as renal or hepatic impairment, may warrant a dose reduction [see Dosage and Administration (2.6)].
8. Use in Specific Populations
8.6 Age and Gender
A population pharmacokinetic analysis of 404 Effexor-treated patients from two studies involving both twice daily and three times daily regimens showed that dose-normalized trough plasma levels of either venlafaxine or ODV were unaltered by age or gender differences. Dosage adjustment based on the age or gender of a patient is generally not necessary [see Dosage and Administration (2.6)] (see Table 15).
8.7 Use in Patient Subgroups
Figure 3. Pharmacokinetics of venlafaxine and its metabolite O-desmethylvenlafaxine (ODV) in special populations:
Abbreviations: ODV, O-desmethylvenlafaxine; AUC, area under the curve; Cmax, peak plasma concentrations;
* Similar effect is expected with strong CYP2D6 inhibitors
9.1. Controlled Substance
Effexor XR is not a controlled substance.
9.2. Abuse
While venlafaxine has not been systematically studied in clinical studies for its potential for abuse, there was no indication of drug-seeking behavior in the clinical studies. However, it is not possible to predict on the basis of premarketing experience the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed. Consequently, physicians should carefully evaluate patients for history of drug abuse and follow such patients closely, observing them for signs of misuse or abuse of venlafaxine (e.g., development of tolerance, incrementation of dose, drug-seeking behavior).
9.3. Dependence
In vitro studies revealed that venlafaxine has virtually no affinity for opiate, benzodiazepine, phencyclidine (PCP), or N-methyl-D-aspartic acid (NMDA) receptors.
Venlafaxine was not found to have any significant CNS stimulant activity in rodents. In primate drug discrimination studies, venlafaxine showed no significant stimulant or depressant abuse liability.
Discontinuation effects have been reported in patients receiving venlafaxine [see Dosage and Administration (2.8)].
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.