EMPLICITI Powder for concentrate for solution for infusion Ref.[8967] Active ingredients: Elotuzumab
Source: European Medicines Agency (EU) Revision Year: 2019 Publisher: Bristol-Myers Squibb Pharma EEIG, Plaza 254, Blanchardstown Corporate Park 2, Dublin 15, D15 T867, Ireland
Pharmacodynamic properties
Pharmacotherapeutic group: Antineoplastic agents, monoclonal antibodies
ATC code: L01XC23
Mechanism of action
Elotuzumab is an immunostimulatory humanised, IgG1 monoclonal antibody that specifically targets the SLAMF7 (signaling lymphocyte activation molecule family member 7) protein. SLAMF7 is highly expressed on multiple myeloma cells independent of cytogenetic abnormalities. SLAMF7 is also expressed on natural killer cells (NK), normal plasma cells, and other immune cells including some T cell subsets, monocytes, B cells, macrophages, and pDCs (plasmacytoid dendritic cells), but is not detected on normal solid tissues or haematopoietic stem cells.
Elotuzumab directly activates natural killer cells through both the SLAMF7 pathway and Fc receptors enhancing anti-myeloma activity in vitro. Elotuzumab also targets SLAMF7 on myeloma cells and through interactions with Fc receptors on specific immune cells, promotes the killing of myeloma cells through NK cell-mediated antibody-dependent cellular cytotoxicity (ADCC) and macrophage-mediated antibody-dependant cellular phagocytosis (ADCP). In nonclinical models, elotuzumab has demonstrated synergistic activity when combined with lenalidomide, pomalidomide or bortezomib.
Clinical efficacy and safety
Empliciti in combination with lenalidomide and dexamethasone (CA204004)
CA204004 is a randomised, open-label study was conducted to evaluate the efficacy and safety of Empliciti in combination with lenalidomide and dexamethasone (E-Ld) in patients with multiple myeloma who have received one to three prior therapies. All patients had documented progression following their most recent therapy. Patients who were refractory to lenalidomide were excluded and 6% of patients had prior lenalidomide treatment. Patients had to recover after transplant for a minimum of 12 weeks from autologous stem cell transplant (SCT), and 16 weeks from allogeneic SCT. Patients with cardiac amyloidosis or plasma cell leukemia were excluded from this study.
Eligible patients were randomised in a 1:1 ratio to receive either Empliciti in combination with lenalidomide and dexamethasone or lenalidomide and dexamethasone (Ld). Treatment was administered in 4-week cycles until disease progression or unacceptable toxicity. Elotuzumab 10 mg/kg was administered intravenously each week for the first 2 cycles and every 2 weeks thereafter. Prior to Empliciti infusion, dexamethasone was administered as a divided dose: an oral dose of 28 mg and an intravenous dose of 8 mg. In the control group and on weeks without Empliciti, dexamethasone 40 mg was administered as a single oral dose weekly. Lenalidomide 25 mg was taken orally once daily for the first 3 weeks of each cycle. Assessment of tumour response was conducted every 4 weeks.
A total of 646 patients were randomised to receive treatment: 321 to Empliciti in combination with lenalidomide and dexamethasone and 325 to lenalidomide and dexamethasone.
Demographics and baseline characteristics were well balanced between treatment arms. The median age was 66 years (range 37 to 91); 57% of patients were older than 65 years; 60% of patients were male; Whites comprised 84% of the study population, Asians 10%, and blacks 4%. The International Staging System (ISS) Stage was I in 43%, II in 32% and III in 21% of patients. The high risk cytogenetic categories of del17p and t(4;14) were present in 32% and 9% of patients, respectively. The median number of prior therapies was 2. Thirty-five percent (35%) of patients were refractory (progression during or within 60 days of last therapy) and 65% were relapsed (progression after 60 days of last therapy). Prior therapies included: stem cell transplant (55%), bortezomib (70%) melphalan (65%), thalidomide (48%), and lenalidomide (6%).
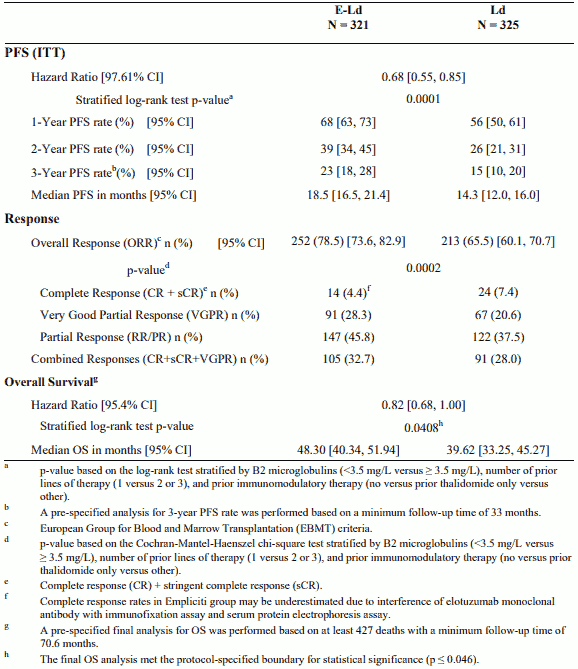
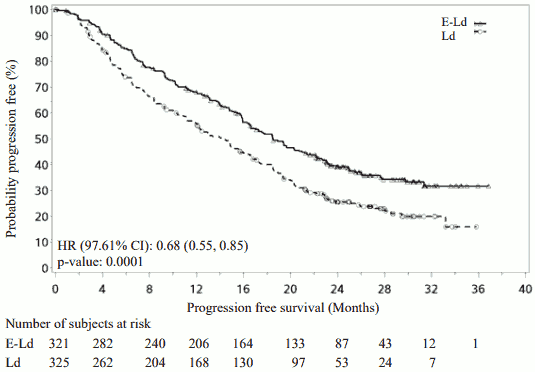
The primary endpoints of this study, progression-free survival (PFS), as assessed by hazard ratio, and overall response rate (ORR) were determined based on assessments made by a blinded Independent Review Committee (IRC). Efficacy results are presented in Table 8 and Figure 1. The median number of treatment cycles was 19 for the Empliciti arm and 14 for the comparator arm.
Overall survival (OS) was a secondary endpoint with the pre-planned final OS analysis to occur after at least 427 deaths.
Table 8. CA204004 Efficacy results:
Figure 1. CA204004 Progression free survival:
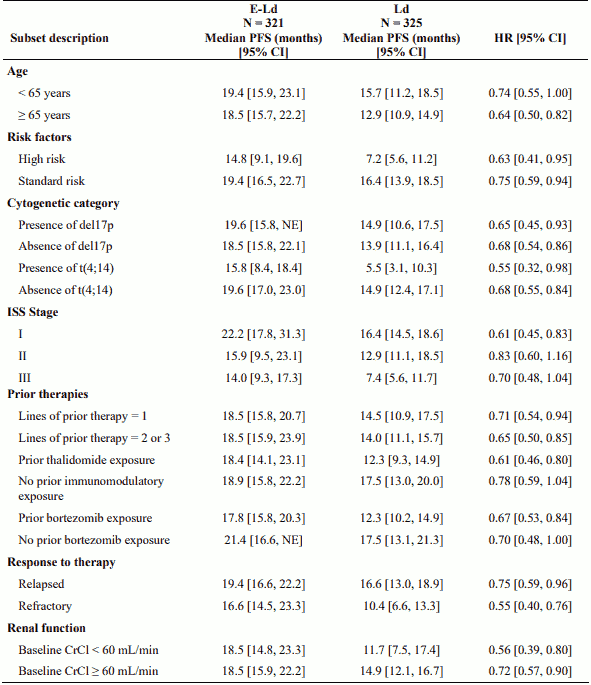
Improvements observed in PFS were consistent across subsets regardless of age (<65 versus ≥65), risk status, presence or absence of cytogenetic categories del17p or t(4;14), ISS stage, number of prior therapies, prior immunomodulatory exposure, prior bortezomib exposure, relapsed or refractory status or renal function as shown in Table 9.
Table 9. CA204004 Efficacy results for subsets:
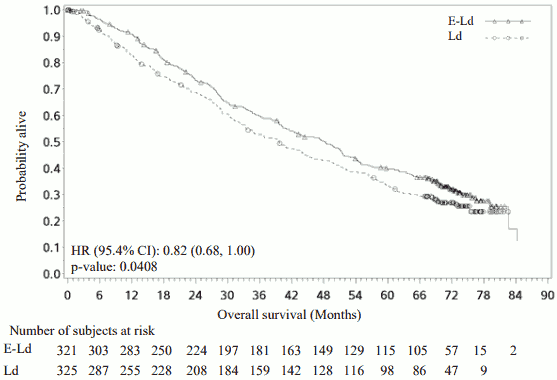
The 1-, 2-, 3-, 4- and 5-year rates of overall survival for Empliciti in combination with lenalidomide and dexamethasone treatment were 91%, 73%, 60%, 50% and 40% respectively, compared with 83%, 69%, 53%, 43% and 33% respectively, for lenalidomide and dexamethasone treatment (See Figure 2).
The pre-planned final OS analysis was performed after 212 deaths in the E-Ld arm and 225 deaths in the Ld arm. The minimum follow-up was 70.6 months. A statistically significant advantage in OS was observed in patients in the E-Ld arm compared to patients in the Ld arm. The median OS in the E-Ld arm was 48.30 months compared with 39.62 months in the Ld arm. Patients in the E-Ld arm had an 18% reduction in the risk of death compared with those in the Ld arm (HR = 0.82; 95.4% CI: 0.68, 1.00; p-value = 0.0408). See Table 8 and Figure 2.
Figure 2. CA204004 Overall survival:
Empliciti in combination with pomalidomide and dexamethasone (CA204125)
CA204125 is a randomised, open-label study conducted to evaluate the efficacy and safety of Empliciti in combination with pomalidomide and dexamethasone (E-Pd) in patients with refractory or relapsed and refractory multiple myeloma who have received at least two prior therapies including lenalidomide and a proteasome inhibitor (PI) and had disease progression on or within 60 days of their last therapy. Patients were refractory if they had progressed on or within 60 days of treatment with lenalidomide and a PI and on or within 60 days of their last treatment, or relapsed and refractory if they had achieved at least a partial response to previous treatment with lenalidomide and a PI but progressed within 6 months and had developed progressive disease on or within 60 days after completing their last treatment. Patients with Grade 2 or higher peripheral neuropathy were excluded from the clinical studies with E-Pd.
A total of 117 patients were randomised in a 1:1 ratio to receive treatment: 60 to elotuzumab in combination with pomalidomide and dexamethasone (E-Pd) and 57 to pomalidomide and dexamethasone (Pd). Treatment was administered in 4-week cycles (28-day cycle) until disease progression or unacceptable toxicity. Elotuzumab 10 mg/kg was administered intravenously each week for the first 2 cycles and 20 mg/kg every 4 weeks thereafter.
Dexamethasone was administered on day 1, 8, 15 and 22 of each cycle. On weeks with Empliciti infusion, dexamethasone was administered before Empliciti as a divided dose: subjects ≤75 years an oral dose of 28 mg and an intravenous dose of 8 mg, and in subjects >75 years an oral dose of 8 mg and an intravenous dose of 8 mg. On weeks without an Empliciti infusion and in the control group, dexamethasone was administered in subjects ≤75 years as an oral dose of 40 mg and in subjects >75 years as an oral dose of 20 mg dexamethasone. Assessment of tumour response was conducted every 4 weeks.
Demographics and baseline characteristics were balanced between treatment arms. The median age was 67 years (range 36 to 81); 62% of patients were older than 65 years; 57% of patients were male; whites comprised 77% of the study population, Asians 21%, and blacks 1%. The International Staging System (ISS) Stage was I in 50%, II in 38% and III in 12% of patients. The chromosomal abnormalities as determined by the FISH of del(17p), t(4;14) and t(14;16) were present in 5%, 11% and 7% of patients, respectively. Eleven (9.4%) patients had high-risk myeloma. The median number of prior therapies was 3. Eighty-seven percent (87%) of the patients were refractory to lenalidomide, 80% refractory to a PI and 70% were refractory to both lenalidomide and a PI. Prior therapies included stem cell transplant (55%), bortezomib (100%), lenalidomide (99%), cyclophosphamide (66%), melphalan (63%), carfilzomib (21%), ixazomib (6%), and daratumumab (3%).
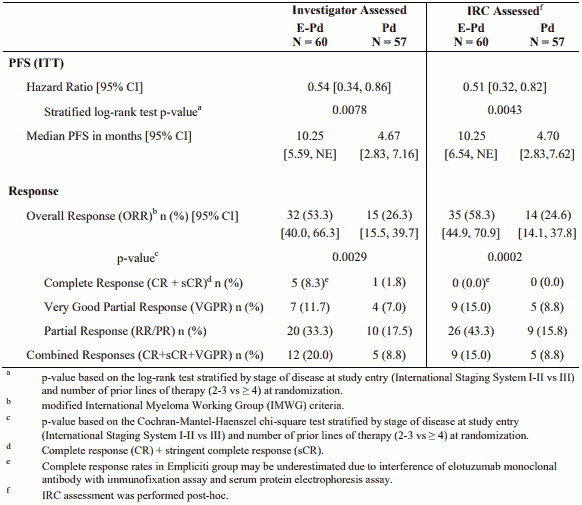
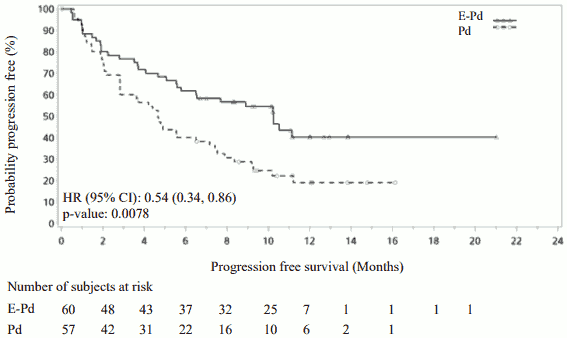
The median number of treatment cycles was 9 for the E-Pd arm and 5 for the Pd arm. The primary endpoint was investigator assessed PFS by modified International Myeloma Working Group (IMWG) criteria. The median PFS per ITT was 10.25 months (95% CI: 5.59, NE) in the E-Pd arm and 4.67 months (95% CI: 2.83, 7.16) in the Pd arm. PFS and ORR were also assessed by the IRC.
PFS results per the investigator and IRC are summarised in Table 10 (minimum follow-up of 9.1 months). Kaplan-Meier curve for PFS per the investigator is provided in Figure 3.
Table 10. CA204125 Efficacy results:
Figure 3. CA204125 Progression free survival per investigator:
PFS ITT assessment per investigator was evaluated in several subgroups including age (<65 versus ≥65), race, ISS stage, prior therapies, transplant, risk category, ECOG status, creatinine clearance, and cytogenic abnormalities. Regardless of the subgroup evaluated, PFS was generally consistent with that observed in the ITT population for the treatment groups. However, results should be taken with caution as assessment of consistency of effect within the different subgroups was hampered by the very limited number of patients included in the different subgroups.
Overall survival (OS) was a key secondary study endpoint. The OS data from the exploratory analysis were not mature at the data cut-off (29 November 2018) with a minimum follow up of 18.3 months. A total of 40 (67%) patients were alive in the E-Pd arm and 29 (51%) in the Pd arm. Median OS was not reached for E-Pd treatment group. The hazard ratio and 95% CI were 0.54 (0.30, 0.96).
Paediatric population
The European Medicines Agency has waived the obligation to submit the results of studies in all subsets of the paediatric population in treatment of multiple myeloma (see section 4.2 for information on paediatric use).
Pharmacokinetic properties
The pharmacokinetics (PK) of elotuzumab was studied in patients with multiple myeloma. Elotuzumab exhibits nonlinear PK with decrease in clearance with increase in dose from 0.5-20 mg/kg.
Absorption
Elotuzumab is dosed via intravenous route and therefore is immediately and completely bioavailable.
Distribution
The geometric mean volume of distribution of elotuzumab at the recommended dosing regimen in combination with lenalidomide/dexamethasone or pomalidomide/dexamethasone at steady state is 5.7 L (CV: 23%) and 5.6 L (CV: 21%) respectively.
Biotransformation
The metabolic pathway of elotuzumab has not been characterized. As an IgG monoclonal antibody, elotuzumab is expected to be degraded into small peptides and amino acids via catabolic pathways.
Elimination
The geometric mean total clearance of elotuzumab at 10 mg/kg (in combination with lenalidomide and dexamethasone) at steady state is 0.194 L/day (CV: 62.9%). Upon discontinuation of elotuzumab in combination with lenalidomide and dexamethasone or in combination with pomalidomide and dexamethasone, concentrations of elotuzumab will decrease to approximately 3% (approximately 97% washout as estimated by 5 half-lives) of the population predicted steady-state maximal serum concentration by 3 months.
Special populations
Based on a population PK analysis using data from 440 patients, the clearance of elotuzumab increased with increasing body weight supporting a weight-based dose. Population PK analysis suggested that the following factors had no clinically important effect on the clearance of elotuzumab: age, gender, race, baseline LDH, albumin, renal impairment, mild hepatic impairment, and coadministration with lenalidomide/dexamethasone or pomalidomide/dexamethasone. Target-mediated clearance of elotuzumab increased with higher serum M-protein concentrations.
Renal impairment
An open-label study (CA204007) evaluated the pharmacokinetics of elotuzumab in combination with lenalidomide and dexamethasone in patients with multiple myeloma with varying degrees of renal impairment (classified using the CrCl values). The effect of renal impairment on the pharmacokinetics of elotuzumab was evaluated in patients with normal renal function (CrCl >90 mL/min; N = 8), severe renal impairment not requiring dialysis (CrCl <30 mL/min; N = 9), or end-stage renal disease requiring dialysis (CrCl <30 mL/min; N = 9). No clinically important differences in the pharmacokinetics of elotuzumab were found between patients with severe renal impairment (with and without dialysis) and patients with normal renal function (see section 4.2).
Hepatic impairment
Empliciti is an IgG1 monoclonal antibody, which is principally cleared by catabolism. Thus, hepatic functional impairment is not likely to alter its clearance. The effect of hepatic impairment on the clearance of Empliciti was evaluated by population PK analyses in patients with mild hepatic impairment (total bilirubin [TB] ≤ the upper limit of normal [ULN] and AST > ULN or TB <1 to 1.5 × ULN and any AST; N = 33). No clinically important differences in the clearance of Empliciti were found between patients with mild hepatic impairment and patients with normal hepatic function. Elotuzumab has not been studied in patients with moderate (TB >1.5 to 3 × ULN and any AST) or severe hepatic impairment (TB >3 × ULN and any AST) (see section 4.2).
Preclinical safety data
Elotuzumab only recognizes human SLAMF7 protein. Because elotuzumab does not recognize non-human forms of SLAMF7 protein, in vivo safety data from animal studies are irrelevant. In the same line, no carcinogenicity data are available for elotuzumab in animals, nor were fertility and embryo-foetal toxicity studies performed. Non-clinical safety information primarily consists of limited in vitro human cell/tissue studies where no safety findings were identified.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.