IMBRUVICA Hard capsule Ref.[8478] Active ingredients: Ibrutinib
Source: European Medicines Agency (EU) Revision Year: 2020 Publisher: Janssen-Cilag International NV, Turnhoutseweg 30, B-2340, Beerse, Belgium
Pharmacodynamic properties
Pharmacotherapeutic group: Antineoplastic agents, protein kinase inhibitors
ATC code: L01XE27
Mechanism of action
Ibrutinib is a potent, small-molecule inhibitor of Bruton’s tyrosine kinase (BTK). Ibrutinib forms a covalent bond with a cysteine residue (Cys-481) in the BTK active site, leading to sustained inhibition of BTK enzymatic activity. BTK, a member of the Tec kinase family, is an important signalling molecule of the B-cell antigen receptor (BCR) and cytokine receptor pathways. The BCR pathway is implicated in the pathogenesis of several B-cell malignancies, including MCL, diffuse large B-cell lymphoma (DLBCL), follicular lymphoma, and CLL. BTK’s pivotal role in signalling through the B-cell surface receptors results in activation of pathways necessary for B-cell trafficking, chemotaxis and adhesion. Preclinical studies have shown that ibrutinib effectively inhibits malignant B-cell proliferation and survival in vivo as well as cell migration and substrate adhesion in vitro.
Lymphocytosis
Upon initiation of treatment, a reversible increase in lymphocyte counts (i.e. ≥50% increase from baseline and an absolute count >5,000/mcL), often associated with reduction of lymphadenopathy, has been observed in about three fourths of patients with CLL treated with IMBRUVICA. This effect has also been observed in about one third of patients with relapsed or refractory MCL treated with IMBRUVICA. This observed lymphocytosis is a pharmacodynamic effect and should not be considered progressive disease in the absence of other clinical findings. In both disease types, lymphocytosis typically occurs during the first month of IMBRUVICA therapy and typically resolves within a median of 8.0 weeks in patients with MCL and 14 weeks in patients with CLL. A large increase in the number of circulating lymphocytes (e.g. >400,000/mcL) has been observed in some patients.
Lymphocytosis was not observed in patients with WM treated with IMBRUVICA.
In vitro platelet aggregation
In an in vitro study, ibrutinib demonstrated inhibition of collagen-induced platelet aggregation. Ibrutinib did not show meaningful inhibition of platelet aggregation using other agonists of platelet aggregation.
Effect on QT/QTc interval and cardiac electrophysiology
The effect of ibrutinib on the QTc interval was evaluated in 20 healthy male and female subjects in a randomised, double-blind thorough QT study with placebo and positive controls. At a supratherapeutic dose of 1,680 mg, ibrutinib did not prolong the QTc interval to any clinically relevant extent. The largest upper bound of the 2-sided 90% CI for the baseline adjusted mean differences between ibrutinib and placebo was below 10 ms. In this same study, a concentration dependent shortening in the QTc interval was observed (-5.3 ms [90% CI: -9.4, -1.1] at a Cmax of 719 ng/mL following the supratherapeutic dose of 1,680 mg).
Clinical efficacy and safety
MCL
The safety and efficacy of IMBRUVICA in patients with relapsed or refractory MCL were evaluated in a single open-label, multi-center phase 2 study (PCYC-1104-CA) of 111 patients. The median age was 68 years (range: 40 to 84 years), 77% were male and 92% were Caucasian. Patients with Eastern Cooperative Oncology Group (ECOG) performance status of 3 or greater were excluded from the study. The median time since diagnosis was 42 months, and median number of prior treatments was 3 (range: 1 to 5 treatments), including 35% with prior high-dose chemotherapy, 43% with prior bortezomib, 24% with prior lenalidomide, and 11% with prior autologous or allogeneic stem cell transplant. At baseline, 39% of patients had bulky disease (≥5 cm), 49% had high-risk score by Simplified MCL International Prognostic Index (MIPI), and 72% had advanced disease (extranodal and/or bone marrow involvement) at screening.
IMBRUVICA was administered orally at 560 mg once daily until disease progression or unacceptable toxicity. Tumour response was assessed according to the revised International Working Group (IWG) for non-Hodgkin’s lymphoma (NHL) criteria. The primary endpoint in this study was investigator-assessed overall response rate (ORR). Responses to IMBRUVICA are shown in Table 2.
Table 2. ORR and DOR in patients with relapsed or refractory MCL (Study PCYC-1104-CA):
| Total N=111 | |
|---|---|
| ORR (%) | 67.6 |
| 95% CI (%) | (58.0; 76.1) |
| CR (%) | 20.7 |
| PR (%) | 46.8 |
| Median DOR (CR+PR) (months) | 17.5 (15.8, NR) |
| Median time to initial response, months (range) | 1.9 (1.4-13.7) |
| Median time to CR, months (range) | 5.5 (1.7-11.5) |
CI = confidence interval; CR = complete response; DOR = duration of response; ORR = overall response rate; PR = partial response; NR = not reached
The efficacy data was further evaluated by an Independent Review Committee (IRC) demonstrating an ORR of 69%, with a 21% complete response (CR) rate and a 48% partial response (PR) rate. The IRC estimated median DOR was 19.6 months.
The overall response to IMBRUVICA was independent of prior treatment including bortezomib and lenalidomide or underlying risk/prognostic factors, bulky disease, gender or age.
The safety and efficacy of IMBRUVICA were demonstrated in a randomised phase 3, open-label, multicenter study including 280 patients with MCL who received at least one prior therapy (Study MCL3001). Patients were randomised 1:1 to receive either IMBRUVICA orally at 560 mg once daily for 21 days or temsirolimus intravenously at 175 mg on Days 1, 8, 15 of the first cycle followed by 75 mg on Days 1, 8, 15 of each subsequent 21-day cycle. Treatment on both arms continued until disease progression or unacceptable toxicity. The median age was 68 years (range, 34; 88 years), 74% were male and 87% were Caucasian. The median time since diagnosis was 43 months, and median number of prior treatments was 2 (range: 1 to 9 treatments), including 51% with prior high-dose chemotherapy, 18% with prior bortezomib, 5% with prior lenalidomide, and 24% with prior stem cell transplant. At baseline, 53% of patients had bulky disease (≥5 cm), 21% had high-risk score by Simplified MIPI, 60% had extranodal disease and 54% had bone marrow involvement at screening.
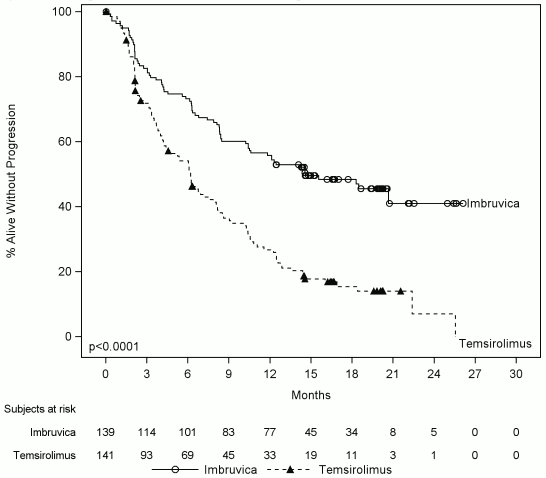
Progression-free survival (PFS) was assessed by IRC according to the revised International Working Group (IWG) for non-Hodgkin’s lymphoma (NHL) criteria. Efficacy results for Study MCL3001 are shown in Table 3 and the Kaplan-Meier curve for PFS in Figure 1.
Table 3. Efficacy Results in patients with relapsed or refractory MCL (Study MCL3001):
| Endpoint | IMBRUVICA N=139 | Temsirolimus N=141 |
|---|---|---|
| PFSa | ||
| Median PFS (95% CI), (months) | 14.6 (10.4, NE) | 6.2 (4.2, 7.9) |
| HR=0.43 [95% CI: 0.32, 0.58] | ||
| ORR (%) | 71.9 | 40.4 |
| p-value | p<0.0001 | |
NE = not estimable; HR = hazard ratio; CI = confidence interval; ORR = overall response rate; PFS = progression-free survival
a IRC evaluated.
A smaller proportion of patients treated with ibrutinib experienced a clinically meaningful worsening of lymphoma symptoms versus temsirolimus (27% versus 52%) and time to worsening of symptoms occurred more slowly with ibrutinib versus temsirolimus (HR 0.27, p<0.0001).
Figure 1. Kaplan-Meier curve of PFS (ITT Population) in Study MCL3001:
CLL
Patients previously untreated for CLL
Single agent:
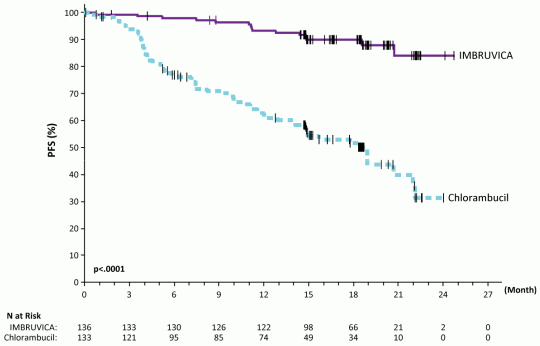
A randomised, multicenter, open-label phase 3 study (PCYC-1115-CA) of IMBRUVICA versus chlorambucil was conducted in patients with treatment-naïve CLL who were 65 years of age or older. Patients between 65 and 70 years of age were required to have at least one comorbidity that precluded the use of frontline chemo-immunotherapy with fludarabine, cyclophosphamide, and rituximab. Patients (n=269) were randomised 1:1 to receive either IMBRUVICA 420 mg daily until disease progression or unacceptable toxicity, or chlorambucil at a starting dose of 0.5 mg/kg on days 1 and 15 of each 28-day cycle for a maximum of 12 cycles, with an allowance for intrapatient dose increases up to 0.8 mg/kg based on tolerability. After confirmed disease progression, patients on chlorambucil were able to crossover to ibrutinib.
The median age was 73 years (range, 65 to 90 years), 63% were male, and 91% were Caucasian. Ninety one percent of patients had a baseline ECOG performance status of 0 or 1 and 9% had an ECOG performance status of 2. The study enrolled 269 patients with CLL. At baseline, 45% had advanced clinical stage (Rai Stage III or IV), 35% of patients had at least one tumor ≥5 cm, 39% with baseline anemia, 23% with baseline thrombocytopenia, 65% had elevated β2 microglobulin >3500 mcg/L, 47% had a CrCL <60 mL/min, 20% of patients presented with del11q, 6% of patients presented with del17p/tumor protein 53 (TP53) mutation, and 44% of patients presented with unmutated immunoglobulin heavy chain variable region (IGHV).
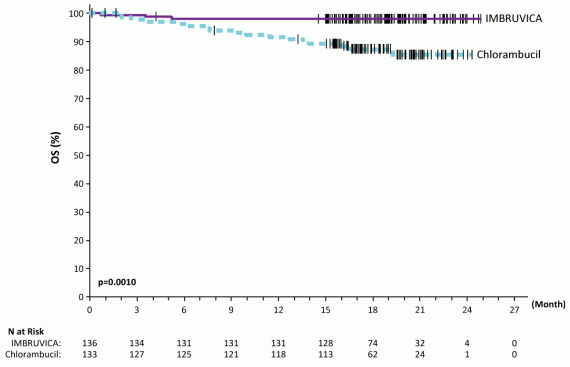
Progression free survival (PFS) as assessed by IRC according to International Workshop on CLL (IWCLL) criteria indicated an 84% statistically significant reduction in the risk of death or progression in the IMBRUVICA arm. Efficacy results for Study PCYC-1115-CA are shown in Table 4 and the Kaplan-Meier curves for PFS and OS are shown in Figures 2 and 3, respectively.
There was a statistically significant sustained platelet or haemoglobin improvement in the ITT population in favor of ibrutinib versus chlorambucil. In patients with baseline cytopenias, sustained hematologic improvement was: platelets 77.1% versus 42.9%; haemoglobin 84.3% versus 45.5% for ibrutinib and chlorambucil respectively.
Table 4. Efficacy results in Study PCYC-1115-CA:
| Endpoint | IMBRUVICA N=136 | Chlorambucil N=133 |
|---|---|---|
| PFSa | ||
| Number of events (%) | 15 (11.0) | 64 (48.1) |
| Median (95% CI), months | Not reached | 18.9 (14.1, 22.0) |
| HR (95% CI) | 0.161 (0.091, 0.283) | |
| ORRa (CR + PR) | 82.4% | 35.3% |
| P-value | <0.0001 | |
| OSb | ||
| Number of deaths (%) | 3 (2.2) | 17 (12.8) |
| HR (95% CI) | 0.163 (0.048, 0.558) | |
CI = confidence interval; HR = hazard ratio; CR = complete response; ORR = overall response rate; OS = overall survival; PFS = progression-free survival; PR = partial response
a IRC evaluated, median follow-up 18.4 months.
b Median OS not reached for both arms. p<0.005 for OS
Figure 2. Kaplan-Meier curve of PFS (ITT Population) in Study PCYC-1115-CA:
Figure 3. Kaplan-Meier curve of OS (ITT Population) in Study PCYC-1115-CA:
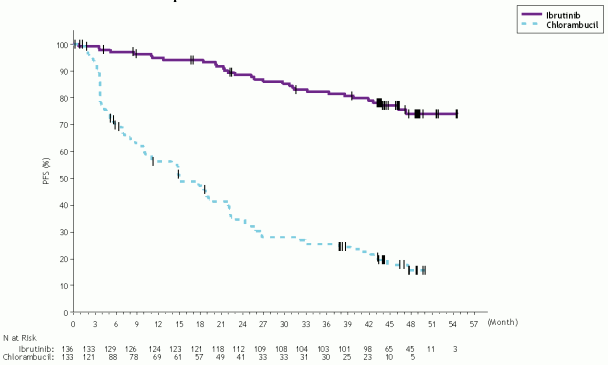
48-month follow-up:
With a median follow-up time on study of 48 months in Study PCYC-1115-CA and its extension study, an 86% reduction in the risk of death or progression by investigator assessment was observed for patients in the IMBRUVICA arm. The median investigator-assessed PFS was not reached in the IMBRUVICA arm and was 15 months [95% CI (10.22, 19.35)] in the chlorambucil arm; (HR=0.14 [95% CI (0.09, 0.21)]). The 4-year PFS estimate was 73.9% in the IMBRUVICA arm and 15.5% in the chlorambucil arm, respectively. The updated Kaplan-Meier curve for PFS is shown in Figure 4. The investigator-assessed ORR was 91.2% in the IMBRUVICA arm versus 36.8% in the chlorambucil arm. The CR rate according to IWCLL criteria was 16.2% in the IMBRUVICA arm versus 3.0% in the chlorambucil arm. At the time of long-term follow-up, a total of 73 subjects (54.9%) originally randomized to the chlorambucil arm subsequently received ibrutinib as cross-over treatment. The Kaplan-Meier landmark estimate for OS at 48-months was 85.5% in the IMBRUVICA arm.
The treatment effect of ibrutinib in Study PCYC-1115-CA was consistent across high-risk patients with del17p/TP53 mutation, del11q, and/or unmutated IGHV.
Figure 4. Kaplan-Meier Curve of PFS (ITT Population) in Study PCYC-1115-CA with 48 Months Follow-up:
Combination therapy:
The safety and efficacy of IMBRUVICA in patients with treatment naïve CLL/SLL were further evaluated in a randomized, multi-center, open-label, Phase 3 study (PCYC-1130-CA) of IMBRUVICA in combination with obinutuzumab versus chlorambucil in combination with obinutuzumab. The study enrolled patients who were 65 years of age or older or <65 years of age with coexisting medical conditions, reduced renal function as measured by creatinine clearance <70 mL/min, or presence of del17p/TP53 mutation. Patients (n=229) were randomized 1:1 to receive either IMBRUVICA 420 mg daily until disease progression or unacceptable toxicity or chlorambucil at a dose of 0.5 mg/kg on Days 1 and 15 of each 28-day cycle for 6 cycles. In both arms, patients received 1000 mg of obinutuzumab on Days 1, 8 and 15 of the first cycle, followed by treatment on the first day of 5 subsequent cycles (total of 6 cycles, 28 days each). The first dose of obinutuzumab was divided between day 1 (100 mg) and day 2 (900 mg).
The median age was 71 years (range, 40 to 87 years), 64% were male, and 96% were Caucasian. All patients had a baseline ECOG performance status of 0 (48%) or 1-2 (52%). At baseline, 52% had advanced clinical stage (Rai Stage III or IV), 32% of patients had bulky disease (≥5 cm), 44% with baseline anemia, 22% with baseline thrombocytopenia, 28% had a CrCL <60 mL/min, and the median Cumulative Illness Rating Score for Geriatrics (CIRS-G) was 4 (range, 0 to 12). At baseline, 65% of patients presented with CLL/SLL with high risk factors (del17p/TP53 mutation [18%], del11q [15%], or unmutated IGHV [54%]).
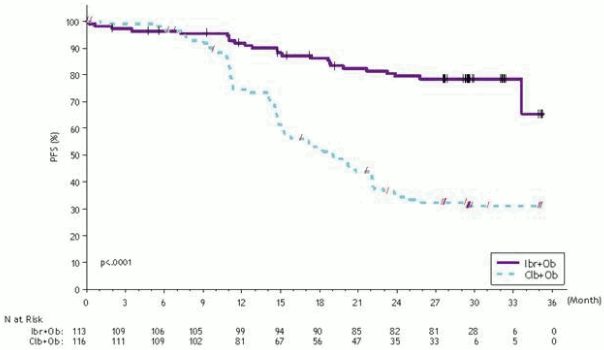
Progression-free survival (PFS) was assessed by IRC according to IWCLL criteria indicated a 77% statistically significant reduction in the risk of death or progression in the IMBRUVICA arm. With a median follow-up time on study of 31 months, the median PFS was not reached in the IMBRUVICA+obinutuzumab arm and was 19 months in the chlorambucil+obinutuzumab arm. Efficacy results for Study PCYC-1130-CA are shown in Table 5 and the Kaplan-Meier curve for PFS is shown in Figure 5.
Table 5. Efficacy results in Study PCYC-1130-CA:
| Endpoint | IMBRUVICA+Obinutuzumab N=113 | Chlorambucil+Obinutuzumab N=116 |
|---|---|---|
| Progression Free Survivala | ||
| Number of events (%) | 24 (21.2) | 74 (63.8) |
| Median (95% CI), months | Not reached | 19.0 (15.1, 22.1) |
| HR (95% CI) | 0.23 (0.15, 0.37) | |
| Overall Response Ratea (%) | 88.5 | 73.3 |
| CRb | 19.5 | 7.8 |
| PRc | 69.0 | 65.5 |
CI=confidence interval; HR=hazard ratio; CR=complete response; PR=partial response.
a IRC evaluated.
b Includes 1 patient in the IMBRUVICA+obinutuzumab arm with a complete response with incomplete marrow recovery (CRi).
c PR=PR+nPR.
Figure 5. Kaplan-Meier Curve of PFS (ITT Population) in Study PCYC-1130-CA:
The treatment effect of ibrutinib was consistent across the high-risk CLL/SLL population (del17p/TP53 mutation, del11q, or unmutated IGHV), with a PFS HR of 0.15 [95% CI (0.09, 0.27)], as shown in Table 6. The 2-year PFS rate estimates for the high-risk CLL/SLL population were 78.8% [95% CI (67.3, 86.7)] and 15.5% [95% CI (8.1, 25.2)] in the IMBRUVICA+obinutuzumab and chlorambucil+obinutuzumab arms, respectively.
Table 6. Subgroup Analysis of PFS (Study PCYC-1130-CA):
| N | Hazard Ratio | 95% CI | |
|---|---|---|---|
| All subjects | 229 | 0,231 | 0,145, 0,367 |
| High risk (del17p/TP53/del11q/unmutated IGHV) | |||
| Yes | 148 | 0,154 | 0,087, 0,270 |
| Noo | 81 | 0,521 | 0,221, 1,231 |
| Del17p/TP53 | |||
| Yes | 41 | 0,109 | 0,031, 0,380 |
| No | 188 | 0,275 | 0,166, 0,455 |
| FISH | |||
| Del17p | 32 | 0,141 | 0,039, 0,506 |
| Del11q | 35 | 0,131 | 0,030, 0,573 |
| Others | 162 | 0,302 | 0,176, 0,520 |
| Unmutated IGHV | |||
| Yes | 123 | 0,150 | 0,084, 0,269 |
| No | 91 | 0,300 | 0,120, 0,749 |
| Age | |||
| <65 | 46 | 0,293 | 0,122, 0,705 |
| ≥65 | 183 | 0,215 | 0,125, 0,372 |
| Bulky disease | |||
| <5 cm | 154 | 0,289 | 0,161, 0,521 |
| ≥5 cm | 74 | 0,184 | 0,085, 0,398 |
| Rai stage | |||
| 0/I/II | 110 | 0,221 | 0,115, 0,424 |
| III/IV | 119 | 0,246 | 0,127, 0,477 |
| ECOG per CRF | |||
| 0 | 110 | 0,226 | 0,110, 0,464 |
| 1-2 | 119 | 0,239 | 0,130, 0,438 |
Hazard ratio based on non-stratified analysis
Any grade infusion-related reactions were observed in 25% of patients treated with IMBRUVICA+obinutuzumab and 58% of patients treated with chlorambucil+obinutuzumab. Grade 3 or higher or serious infusion-related reactions were observed in 3% of patients treated with IMBRUVICA+obinutuzumab and 9% of patients treated with chlorambucil+obinutuzumab.
Patients with CLL who received at least one prior therapy
Single agent:
The safety and efficacy of IMBRUVICA in patients with CLL were demonstrated in one uncontrolled study and one randomised, controlled study. The open-label, multi-center study (PCYC-1102-CA) included 51 patients with relapsed or refractory CLL, who received 420 mg once daily. IMBRUVICA was administered until disease progression or unacceptable toxicity. The median age was 68 years (range: 37 to 82 years), median time since diagnosis was 80 months, and median number of prior treatments was 4 (range: 1 to 12 treatments), including 92.2% with a prior nucleoside analog, 98.0% with prior rituximab, 86.3% with a prior alkylator, 39.2% with prior bendamustine and 19.6% with prior ofatumumab. At baseline, 39.2% of patients had Rai Stage IV, 45.1% had bulky disease (≥5 cm), 35.3% had deletion 17p and 31.4% had deletion 11q.
ORR was assessed according to the 2008 IWCLL criteria by investigators and IRC. At a median duration follow up of 16.4 months, the ORR by IRC for the 51 relapsed or refractory patients was 64.7% (95% CI: 50.1%; 77.6%), all PRs. The ORR including PR with lymphocytosis was 70.6%. Median time to response was 1.9 months. The DOR ranged from 3.9 to 24.2+ months. The median DOR was not reached.
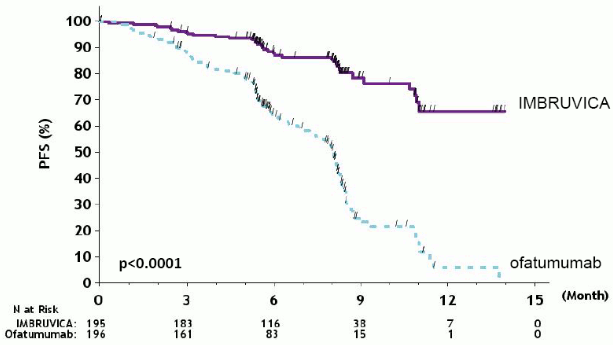
A randomised, multi-center, open-label phase 3 study of IMBRUVICA versus ofatumumab (PCYC-1112-CA) was conducted in patients with relapsed or refractory CLL. Patients (n=391) were randomised 1:1 to receive either IMBRUVICA 420 mg daily until disease progression or unacceptable toxicity, or ofatumumab for up to 12 doses (300/2,000 mg). Fifty-seven patients randomised to ofatumumab crossed over following progression to receive IMBRUVICA. The median age was 67 years (range: 30 to 88 years), 68% were male, and 90% were Caucasian. All patients had a baseline ECOG performance status of 0 or 1. The median time since diagnosis was 91 months and the median number of prior treatments was 2 (range: 1 to 13 treatments). At baseline, 58% of patients had at least one tumour ≥5 cm. Thirty-two percent of patients had deletion 17p (with 50% of patients having deletion 17p/TP53 mutation), 24% had 11q deletion, and 47% of patients had unmutated IGHV.
Progression free survival (PFS) as assessed by an IRC according to IWCLL criteria indicated a 78% statistically significant reduction in the risk of death or progression for patients in the IMBRUVICA arm. Analysis of OS demonstrated a 57% statistically significant reduction in the risk of death for patients in the IMBRUVICA arm. Efficacy results for Study PCYC-1112-CA are shown in Table 7.
Table 7. Efficacy results in patients with CLL (Study PCYC-1112-CA):
| Endpoint | IMBRUVICA N=195 | Ofatumumab N=196 |
|---|---|---|
| Median PFS | Not reached | 8.1 months |
| HR=0.215 [95% CI: 0.146; 0.317] | ||
| OSa | HR=0.434 [95% CI: 0.238; 0.789]b | |
| HR=0.387 [95% CI: 0.216; 0.695]c | ||
| ORRd,e (%) | 42.6 | 4.1 |
| ORR including PR with lymphocytosisd (%) | 62.6 | 4.1 |
HR = hazard ratio; CI = confidence interval; ORR = overall response rate; OS = overall survival; PFS = progression-free survival; PR = partial response
a Median OS not reached for both arms. p<0.005 for OS.
b Patients randomised to ofatumumab were censored when starting IMBRUVICA if applicable.
c Sensitivity analysis in which crossover patients from the ofatumumab arm were not censored at the date of first dose of IMBRUVICA.
d Per IRC. Repeat CT scans required to confirm response.
e All PRs achieved; p<0.0001 for ORR.
Median follow-up time on study=9 months
The efficacy was similar across all of the subgroups examined, including in patients with and without deletion 17p, a pre-specified stratification factor (Table 8).
Table 8. Subgroup analysis of PFS (Study PCYC-1112-CA):
| N | Hazard Ratio | 95 % CI | |
|---|---|---|---|
| All subjects | 391 | 0,210 | (0,143, 0,308) |
| Del17P | |||
| Yes | 127 | 0,247 | (0,136, 0,450) |
| No | 264 | 0,194 | (0,117, 0,323) |
| Refractory disease to purine analog | |||
| Yes | 175 | 0,178 | (0,100, 0,320) |
| No | 216 | 0,242 | (0,145, 0,404) |
| Age | |||
| <65 | 152 | 0,166 | (0,088, 0,315) |
| ≥65 | 239 | 0,243 | (0,149, 0,395) |
| Number of prior lines | |||
| <3 | 198 | 0,189 | (0,100, 0,358) |
| ≥3 | 193 | 0,212 | (0,130, 0,344) |
| Bulky disease | |||
| <5 cm | 163 | 0,237 | (0,127, 0,442) |
| ≥5 cm | 225 | 0,191 | (0,117, 0,311) |
Hazard ratio based on non-stratified analysis.
The Kaplan-Meier curve for PFS is shown in Figure 6.
Figure 6. Kaplan-Meier curve of PFS (ITT Population) in Study PCYC-1112-CA:
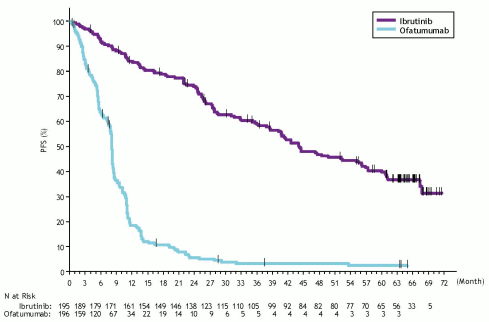
Final Analysis at 65-month follow-up:
With a median follow-up time on study of 65 months in Study PCYC-1112-CA, an 85% reduction in the risk of death or progression by investigator assessment was observed for patients in the IMBRUVICA arm. The median investigator-assessed PFS according to IWCLL criteria was 44.1 months [95% CI (38.47, 56.18)] in the IMBRUVICA arm and 8.1 months [95% CI (7.79, 8.25)] in the ofatumumab arm, respectively; HR=0.15 [95% CI (0.11, 0.20)]. The updated Kaplan-Meier curve for PFS is shown in Figure 7. The investigator-assessed ORR in the IMBRUVICA arm was 87.7% versus 22.4% in the ofatumumab arm. At the time of final analysis, 133 (67.9%) of the 196 subjects originally randomized to the ofatumumab treatment arm had crossed over to ibrutinib treatment. The median investigator-assessed PFS2 (time from randomisation until PFS event after first subsequent anti-neoplastic therapy) according to IWCLL criteria was 65.4 months [95% CI (51.61, not estimable)] in the IMBRUVICA arm and 38.5 months [95% CI (19.98, 47.24)] in the ofatumumab arm, respectively; HR=0.54 [95% CI (0.41, 0.71)]. The median OS was 67.7 months [95% CI (61.0, not estimable)] in the IMBRUVICA arm.
The treatment effect of ibrutinib in Study PCYC-1112-CA was consistent across high-risk patients with deletion 17p/TP53 mutation, deletion 11q, and/or unmutated IGHV.
Figure 7. Kaplan-Meier Curve of PFS (ITT Population) in Study PCYC-1112-CA at Final Analysis with 65 Months Follow-up:
Combination therapy:
The safety and efficacy of IMBRUVICA in patients previously treated for CLL were further evaluated in a randomised, multicenter, double-blinded phase 3 study of IMBRUVICA in combination with BR versus placebo+BR (Study CLL3001). Patients (n=578) were randomised 1:1 to receive either IMBRUVICA 420 mg daily or placebo in combination with BR until disease progression, or unacceptable toxicity. All patients received BR for a maximum of six 28-day cycles. Bendamustine was dosed at 70 mg/m² infused IV over 30 minutes on Cycle 1, Days 2 and 3, and on Cycles 2-6, Days 1 and 2 for up to 6 cycles. Rituximab was administered at a dose of 375 mg/m² in the first cycle, Day 1, and 500 mg/m² Cycles 2 through 6, Day 1. Ninety patients randomised to placebo+BR crossed over to receive IMBRUVICA following IRC confirmed progression. The median age was 64 years (range, 31 to 86 years), 66% were male, and 91% were Caucasian. All patients had a baseline ECOG performance status of 0 or 1. The median time since diagnosis was 6 years and the median number of prior treatments was 2 (range, 1 to 11 treatments). At baseline, 56% of patients had at least one tumour ≥5 cm, 26% had del11q.
Progression free survival (PFS) was assessed by IRC according to IWCLL criteria. Efficacy results for Study CLL3001 are shown in Table 9.
Table 9. Efficacy Results in patients with CLL (Study CLL3001):
| Endpoint | IMBRUVICA+BR N=289 | Placebo+BR N=289 |
|---|---|---|
| PFSa | ||
| Median (95% CI), months | Not reached | 13.3 (11.3, 13.9) |
| HR=0.203 [95% CI: 0.150, 0.276] | ||
| ORRb % | 82.7 | 67.8 |
| OSc | HR=0.628 [95% CI: 0.385, 1.024] | |
CI=confidence interval; HR=hazard ratio; ORR=overall response rate; OS=overall survival; PFS=progression-free survival
a IRC evaluated.
b IRC evaluated, ORR (complete response, complete response with incomplete marrow recovery, nodular partial response, partial response).
c Median OS not reached for both arms.
WM
Single agent:
The safety and efficacy of IMBRUVICA in WM (IgM-excreting lymphoplasmacytic lymphoma) were evaluated in an open-label, multi-center, single-arm trial of 63 previously treated patients. The median age was 63 years (range: 44 to 86 years), 76% were male, and 95% were Caucasian. All patients had a baseline ECOG performance status of 0 or 1. The median time since diagnosis was 74 months, and the median number of prior treatments was 2 (range: 1 to 11 treatments). At baseline, the median serum IgM value was 3.5 g/dL, and 60% of patients were anaemic (haemoglobin ≤11 g/dL or 6.8 mmol/L).
IMBRUVICA was administered orally at 420 mg once daily until disease progression or unacceptable toxicity. The primary endpoint in this study was ORR per investigator assessment. The ORR and DOR were assessed using criteria adopted from the Third International Workshop of WM. Responses to IMBRUVICA are shown in Table 10.
Table 10. ORR and DOR in patients with WM:
| Total (N=63) | |
|---|---|
| ORR (%) | 87.3 |
| 95% CI (%) | (76.5, 94.4) |
| VGPR (%) | 14.3 |
| PR (%) | 55.6 |
| MR (%) | 17.5 |
| Median DOR months (range) | NR (0.03+, 18.8+) |
CI = confidence interval; DOR = duration of response; NR = not reached; MR = minor response; PR = partial response; VGPR = very good partial response; ORR = MR + PR + VGPR
Median follow-up time on study = 14.8 months
The median time to response was 1.0 month (range: 0.7-13.4 months). Efficacy results were also assessed by an IRC demonstrating an ORR of 83%, with a 11% VGPR rate and a 51% PR rate.
Combination therapy:
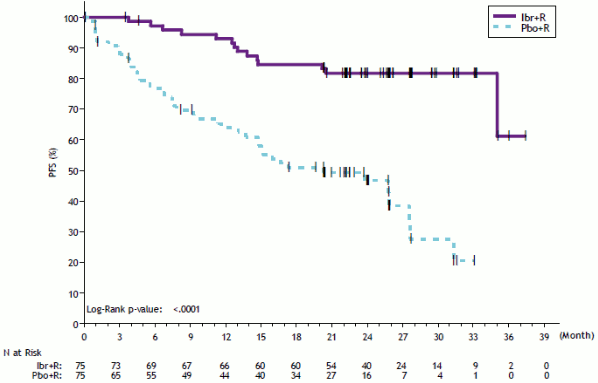
The safety and efficacy of IMBRUVICA in WM were further evaluated in patients with treatment-naïve or previously treated WM in a randomized, multicenter, double-blinded phase 3 study of IMBRUVICA in combination with rituximab versus placebo in combination with rituximab (PCYC-1127-CA). Patients (n=150) were randomized 1:1 to receive either IMBRUVICA 420 mg daily or placebo in combination with rituximab until disease progression or unacceptable toxicity. Rituximab was administered weekly at a dose of 375 mg/m² for 4 consecutive weeks (weeks 1-4) followed by a second course of weekly rituximab for 4 consecutive weeks (weeks 17-20).
The median age was 69 years (range, 36 to 89 years), 66% were male, and 79% were Caucasian. Ninety-three percent of patients had a baseline ECOG performance status of 0 or 1, and 7% of patients had a baseline ECOG performance status of 2. Forty-five percent of patients were treatment-naïve, and 55% of patients were previously treated. The median time since diagnosis was 52.6 months (treatment-naïve patients=6.5 months and previously treated patients=94.3 months). Among previously treated patients, the median number of prior treatments was 2 (range, 1 to 6 treatments). At baseline, the median serum IgM value was 3.2 g/dL (range, 0.6 to 8.3 g/dL), 63% of patients were anaemic (haemoglobin ≤11 g/dL or 6.8 mmol/L) and MYD88 L265P mutations were present in 77% of patients, absent in 13% of patients, and 9% of patients were not evaluable for mutation status.
Progression free survival (PFS) as assessed by IRC indicated an 80% statistically significant reduction in the risk of death or progression in the IMBRUVICA arm. Efficacy results for Study PCYC-1127- CA are shown in Table 11 and the Kaplan-Meier curve for PFS is shown in Figure 8. PFS hazard ratios for treatment-naïve patients, previously treated patients, and patients with or without MYD88 L265P mutations were consistent with the PFS hazard ratio for the ITT population.
Table 11. Efficacy results in Study PCYC-1127-CA:
| Endpoint | IMBRUVICA+R N=75 | Εικονικό φάρμακο + R N=75 |
|---|---|---|
| Progression Free Survivala | ||
| Number of events (%) | 14 (18,7) | 42 (56,0) |
| Median (95% CI), months | Not reached | 20,3 (13,7, 27,6) |
| HR (95% CI) | 0,20 (0,11, 0,38) | |
| TTnT | ||
| Median (95% CI), months | Not reached | 18,1 (11,1, ΜΕ) |
| HR (95% CI) | 0,1 (0,04, 0,23) | |
| Best Overall Response (%) | ||
| CR | 2,7 | 1,3 |
| VGPR | 22,7 | 4,0 |
| PR | 46,7 | 26,7 |
| MR | 20,0 | 14,7 |
| Overall Response Rate (CR, VGPR, PR, MR)b (%) | 92,0 | 46,7 |
| Median duration of overall response, months (range) | Not reached (1,9+, 36,4+) | 24,8 (1,9, 30,3+) |
| Response Rate (CR, VGPR, PR)b (%) | 72,0 | 32,0 |
| Median duration of response, months (range) | Not reached (1,9+, 36,4+) | 21,2 (4,6, 25,8) |
| Rate of Sustained Haemoglobin Improvementb,c (%) | 73,3 | 41,3 |
CI = confidence interval; CR = complete response; HR = hazard ratio; MR = minor response; NE = not estimable; PR = partial response; R = Rituximab; TTnT = time to next treatment; VGPR = very good partial response
a IRC evaluated.
b p-value associated with response rate was <0.0001.
c Defined as increase of ≥2 g/dL over baseline regardless of baseline value, or an increase to >11 g/dL with a ≥0.5 g/dL improvement if baseline was ≤11 g/dL.
Median follow-up time on study=26.5 months.
Figure 8. Kaplan-Meier Curve of PFS (ITT Population) in Study PCYC-1127-CA:
Grade 3 or 4 infusion-related reactions were observed in 1% of patients treated with IMBRUVICA+rituximab and 16% of patients treated with placebo+rituximab.
Tumor flare in the form of IgM increase occurred in 8.0% of subjects in the IMBRUVICA+rituximab arm and 46.7% of subjects in the placebo+rituximab arm.
Study PCYC-1127-CA had a separate monotherapy arm of 31 patients with previously treated WM who failed prior rituximab-containing therapy and received single agent IMBRUVICA. The median age was 67 years (range, 47 to 90 years). Eighty-one percent of patients had a baseline ECOG performance status of 0 or 1, and 19% had a baseline ECOG performance status of 2. The median number of prior treatments was 4 (range, 1 to 7 treatments). The response rate per IRC observed in the monotherapy arm was 71% (0% CR, 29% VGPR, 42% PR). The overall response rate per IRC observed in the monotherapy arm was 87% (0% CR, 29% VGPR, 42% PR, 16% MR). With a median follow-up time on study of 34 months (range, 8.6+ to 37.7 months), the median duration of response has not been reached.
Paediatric population
The European Medicines Agency has waived the obligation to submit the results of studies with IMBRUVICA in all subsets of the paediatric population in MCL, CLL and lymphoplasmacytic lymphoma (LPL) (for information on paediatric use, see section 4.2).
Pharmacokinetic properties
Absorption
Ibrutinib is rapidly absorbed after oral administration with a median Tmax of 1 to 2 hours. Absolute bioavailability in fasted condition (n=8) was 2.9% (90% CI = 2.1–3.9) and doubled when combined with a meal. Pharmacokinetics of ibrutinib does not significantly differ in patients with different B-cell malignancies. Ibrutinib exposure increases with doses up to 840 mg. The steady state AUC observed in patients at 560 mg is (mean ± standard deviation) 953 ± 705 ng h/mL. Administration of ibrutinib in fasted condition resulted in approximately 60% of exposure (AUClast) as compared to either 30 minutes before, 30 minutes after (fed condition) or 2 hours after a high fat breakfast.
Ibrutinib has a pH dependent solubility, with lower solubility at higher pH. In fasted healthy subjects administered a single 560 mg dose of ibrutinib after taking omeprazole at 40 mg once daily for 5 days, compared to ibrutinib alone, geometric mean ratios (90% CI) were 83% (68-102%), 92% (78-110%), and 38% (26-53%) for AUC0-24, AUClast, and Cmax, respectively.
Distribution
Reversible binding of ibrutinib to human plasma protein in vitro was 97.3% with no concentration dependence in the range of 50 to 1,000 ng/mL. The apparent volume of distribution at steady state (Vd,ss/F) was approximately 10,000 L.
Metabolism
Ibrutinib is metabolised primarily by CYP3A4 to produce a dihydrodiol metabolite with an inhibitory activity towards BTK approximately 15 times lower than that of ibrutinib. Involvement of CYP2D6 in the metabolism of ibrutinib appears to be minimal.
Therefore, no precautions are necessary in patients with different CYP2D6 genotypes.
Elimination
Apparent clearance (CL/F) is approximately 1,000 L/h. The half-life of ibrutinib is 4 to 13 hours. After a single oral administration of radiolabeled [14C]-ibrutinib in healthy subjects, approximately 90% of radioactivity was excreted within 168 hours, with the majority (80%) excreted in the faeces and <10% accounted for in urine. Unchanged ibrutinib accounted for approximately 1% of the radiolabeled excretion product in faeces and none in urine.
Special populations
Elderly
Population pharmacokinetics indicated that age does not significantly influence ibrutinib clearance from the circulation.
Paediatric population
No pharmacokinetic studies were performed with IMBRUVICA in patients under 18 years of age.
Gender
Population pharmacokinetics data indicated that gender does not significantly influence ibrutinib clearance from the circulation.
Race
There are insufficient data to evaluate the potential effect of race on ibrutinib pharmacokinetics.
Body weight
Population pharmacokinetics data indicated that body weight (range: 41-146 kg; mean [SD]: 83 [19 kg]) had a negligible effect on ibrutinib clearance.
Renal impairment
Ibrutinib has minimal renal clearance; urinary excretion of metabolites is <10% of the dose. No specific studies have been conducted to date in subjects with impaired renal function. There are no data in patients with severe renal impairment or patients on dialysis (see section 4.2).
Hepatic impairment
Ibrutinib is metabolised in the liver. A hepatic impairment trial was performed in non-cancer subjects administered a single dose of 140 mg of medicinal product under fasting conditions. The effect of impaired liver function varied substantially between individuals, but on average a 2.7-, 8.2-, and 9.8-fold increase in ibrutinib exposure (AUClast) was observed in subjects with mild (n=6, Child-Pugh class A), moderate (n=10, Child-Pugh class B) and severe (n=8, Child-Pugh class C) hepatic impairment, respectively. The free fraction of ibrutinib also increased with degree of impairment, with 3.0, 3.8 and 4.8% in subjects with mild, moderate and severe liver impairment, respectively, compared to 3.3% in plasma from matched healthy controls within this study. The corresponding increase in unbound ibrutinib exposure (AUCunbound,last) is estimated to be 4.1-, 9.8-, and 13-fold in subjects with mild, moderate, and severe hepatic impairment, respectively (see section 4.2).
Co-administration with CYP substrates
In vitro studies indicated that ibrutinib is a weak reversible inhibitor toward CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, and intestinal (but not hepatic) CYP3A4 and does not display clinically relevant time-dependent inhibition of CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19 and CYP2D6. The dihydrodiol metabolite of ibrutinib is a weak inhibitor toward CYP2B6, CYP2C8, CYP2C9, and CYP2D6. The dihydrodiol metabolite is at most a weak inducer of CYP450 isoenzymes in vitro. Although ibrutinib is a sensitive CYP3A4 substrate, it does not have a clinically relevant effect on its own exposure.
Co-administration with transport substrates/inhibitors
In vitro studies indicated that ibrutinib is not a substrate of P-gp, nor other major transporters, except OCT2. The dihydrodiol metabolite and other metabolites are P-gp substrates. Ibrutinib is an in vitro inhibitor of P-gp and BCRP (see section 4.5).
Preclinical safety data
The following adverse effects were seen in studies of 13-weeks duration in rats and dogs. Ibrutinib was found to induce gastrointestinal effects (soft faeces/diarrhoea and/or inflammation) and lymphoid depletion in rats and dogs with a No Observed Adverse Effect Level (NOAEL) of 30 mg/kg/day in both species. Based on mean exposure (AUC) at the 560 mg/day clinical dose, AUC ratios were 2.6 and 21 at the NOAEL in male and female rats, and 0.4 and 1.8 at the NOAEL in male and female dogs, respectively. Lowest Observed Effect Level (LOEL) (60 mg/kg/day) margins in the dog are 3.6-fold (males) and 2.3-fold (females). In rats, moderate pancreatic acinar cell atrophy (considered adverse) was observed at doses of ≥100 mg/kg in male rats (AUC exposure margin of 2.6-fold) and not observed in females at doses up to 300 mg/kg/day (AUC exposure margin of 21.3-fold). Mildly decreased trabecular and cortical bone was seen in female rats administered ≥100 mg/kg/day (AUC exposure margin of 20.3-fold). All gastrointestinal, lymphoid and bone findings recovered following recovery periods of 6-13 weeks. Pancreatic findings partially recovered during comparable reversal periods.
Juvenile toxicity studies have not been conducted.
Carcinogenicity/genotoxicity
Ibrutinib was not carcinogenic in a 6-month study in the transgenic (Tg.rasH2) mouse at oral doses up to 2000 mg/kg/day with an exposure margin of approximately 23 (males) to 37 (females) times the human AUC of ibrutinib at a dose of 560 mg daily. Ibrutinib has no genotoxic properties when tested in bacteria, mammalian cells or in mice.
Reproductive toxicity
In pregnant rats, ibrutinib at a dose of 80 mg/kg/day was associated with increased post-implantation loss and increased visceral (heart and major vessels) malformations and skeletal variations with an exposure margin 14 times the AUC found in patients at a daily dose of 560 mg. At a dose of ≥40 mg/kg/day, ibrutinib was associated with decreased foetal weights (AUC ratio of ≥5.6 as compared to daily dose of 560 mg in patients). Consequently the foetal NOAEL was 10 mg/kg/day (approximately 1.3 times the AUC of ibrutinib at a dose of 560 mg daily) (see section 4.6).
In pregnant rabbits, ibrutinib at a dose of 15 mg/kg/day or greater was associated with skeletal malformations (fused sternebrae) and ibrutinib at a dose of 45 mg/kg/day was associated with increased post-implantation loss. Ibrutinib caused malformations in rabbits at a dose of 15 mg/kg/day (approximately 2.0 times the exposure (AUC) in patients with MCL administered ibrutinib 560 mg daily and 2.8 times the exposure in patients with CLL or WM receiving ibrutinib dose 420 mg per day). Consequently the foetal NOAEL was 5 mg/kg/day (approximately 0.7 times the AUC of ibrutinib at a dose of 560 mg daily) (see section 4.6).
Fertility
No effects on fertility or reproductive capacities were observed in male or female rats up to the maximum dose tested, 100 mg/kg/day (HED 16 mg/kg/day).
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.