INTRAROSA Pessary Ref.[7593] Active ingredients: Prasterone
Source: European Medicines Agency (EU) Revision Year: 2022 Publisher: Endoceutics S.A., Rue Belliard 40, 1040, Brussels, Belgium
Pharmacodynamic properties
Pharmacotherapeutic group: Other sex hormones and modulators of the genital system
ATC code: G03XX01
Mechanism of action
Intrarosa contains the active ingredient prasterone, i.e. dehydroepiandrosterone (DHEA), which is biochemically and biologically identical to the endogenous human DHEA, a precursor steroid which is inactive by itself and it is converted into oestrogens and androgens. Intrarosa is thus different from the oestrogens preparations since it delivers also androgen metabolites.
An oestrogen-mediated increase in the number of superficial and intermediate cells and decrease in the number of parabasal cells in the vaginal mucosa is noted. In addition, the vaginal pH decreased towards the normal range, thus facilitating the growth of the normal bacterial flora.
Clinical efficacy
Physiological responses (objective measures)
Efficacy data were obtained from two US and Canadian randomised, double-blind, placebo-controlled, multicentre, pivotal phase III trials (ERC-231/Trial 1 and ERC-238/Trial 2) performed in postmenopausal women aged 40 to 80 years (mean age = 58.6 years in Trial 1 and 59.5 years in Trial 2) with vulvar and vaginal atrophy (VVA). At baseline, women had ≤5.0% superficial cells in the vaginal smear, a vaginal pH ˃5.0 and they had identified dyspareunia (moderate to severe) as their most bothersome symptom (MBS) of VVA. After 12 weeks of daily treatment with a prasterone 6.5 mg pessary (n=81 in Trial 1 and n=325 in Trial 2), the change from baseline, in comparison with placebo treatment (n=77 in Trial 1 and n=157 in Trial 2), demonstrated significant improvements of the 3 co-primary endpoints compared to placebo in both studies, namely increase of the percentage of superficial cells (p<0.0001), decrease of the percentage of parabasal cells (p<0.0001), and decrease in the vaginal pH (p<0.0001).
Symptoms (subjective measures)
The most bothersome symptom (MBS) dyspareunia (co-primary endpoint) was assessed at baseline and 12 weeks with the severity scored as follows: None=0, Mild=1, Moderate=2, Severe=3. Table 1 shows the mean change in severity score in MBS dyspareunia after 12 weeks with associated statistical testing for the difference vs. placebo for Trial 1 (ERC-231) and Trial 2 (ERC-238).
Table 1. Primary Efficacy Analysis – Change from Baseline to Week 12 in the Most Bothersome Symptom Dyspareunia (ITT Population; LOCF):
| Study | Dyspareunia | ||
|---|---|---|---|
| Intrarosa 6.5 mg | Placebo | p-value | |
| Trial 1 | -1.27 | -0.87 | 0.0132 |
| Trial 2 | -1.42 | -1.06 | 0.0002 |
Table 2 shows the percentage of subjects who reported a change from baseline in their MBS dyspareunia at week 12. "Improvement" was defined as a reduction in the severity score of 1 or more. "Relief" was defined as no or only mild symptoms at week 12. "Substantial improvement" was restricted to patients who had moderate or severe MBS at baseline and changed from severe to mild or severe or moderate to none.
Table 2: Percentage of Patients with Improvement, Relief or Substantial Improvement of MBS Dyspareunia after 12 Weeks on Intrarosa vs. Placebo (ITT, LOCF):
| Improvement | Relief | Substantial improvement | ||||
|---|---|---|---|---|---|---|
| Intrarosa | Placebo | Intrarosa | Placebo | Intrarosa | Placebo | |
| Trial 1 (Intrarosa: n=81) (Placebo: n=77) | 72.8% (p=0.0565) | 58.4% | 58.0% (p=0.0813) | 44.2% | 43.2% (p=0.0821) | 29.9% |
| Trial 2 (Intrarosa: n=325) (Placebo: n=157) | 80.3% (p=0.0003) | 65.0% | 68.6% (p=0.0003) | 51.6% | 47.1% (p=0.0179) | 35.7% |
Clinical safety
Apart from the main two 12-week phase III clinical studies, the safety data of Intrarosa has also been obtained from one non comparative open-label safety study of one year.
Cases of breast and ovarian cancer have been reported in women treated with 6.5 mg of prasterone for 52 weeks (see section 4.4).
Cases of abnormal Pap smears either Atypical Squamous Cells of Undetermined Significance (ASCUS) or Low Grade Squamous Intraepithelial Lesion (LSIL) have been reported with a common frequency in women treated with Intrarosa for 52 weeks (see section 4.4).
Endometrial safety
On the 389 evaluable end-of-study endometrial biopsies performed after 52 weeks of treatment with Intrarosa, no histological abnormalities were reported on the biopsies.
Paediatric population
The European Medicines Agency has waived the obligation to submit the results of studies with Intrarosa in all subsets of the paediatric population.
Pharmacokinetic properties
Absorption
Prasterone administered in the vagina is an inactive precursor that enters the vaginal cells and is converted intracellularly into cell-specific small amounts of both oestrogens and androgens depending upon the level of enzymes expressed in each cell type. The beneficial effects on the symptoms and signs of vulvar and vaginal atrophy are exerted through activation of the vaginal oestrogen and androgen receptors.
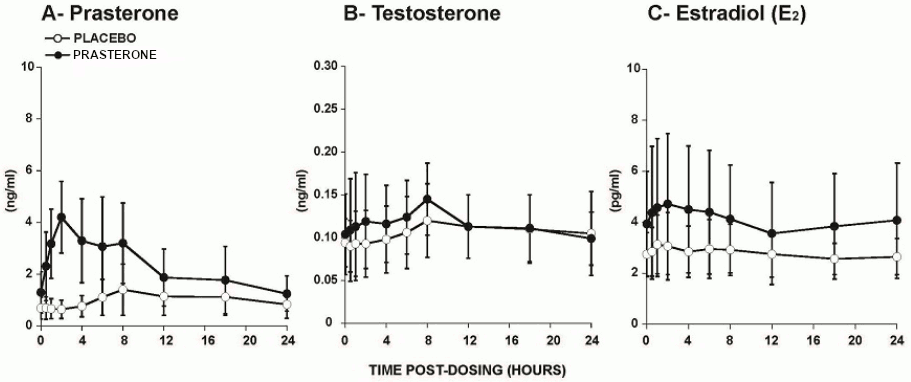
In a study conducted in postmenopausal women, administration of the Intrarosa pessary once daily for 7 days resulted in a mean prasterone Cmax and area under the curve from 0 to 24 hours (AUC0-24) at day 7 of 4.4 ng/mL and 56.2 ng h/mL, respectively, which were significantly higher than those in the group treated with placebo (Table 3; Figure 1). The Cmax and AUC0-24 of the metabolites testosterone and estradiol were also slightly higher in women treated with the Intrarosa pessary compared to those receiving placebo but all remained within normal values of postmenopausal women (<10 pg estradiol/mL; <0.26 ng testosterone/mL) as measured by validated mass spectrometry-based assays for both the study samples and reference values.
Table 3. Cmax and AUC0-24 of Prasterone, Testosterone, and Estradiol on Day 7 Following Daily Administration of Placebo or Intrarosa (mean ± S.D.):
| Placebo (N=9) | INTRAROSA (N=10) | |||||
|---|---|---|---|---|---|---|
| Prasterone | Cmax (ng/ml) | 1.60 (±0.95) | 4.42 (±1.49) | |||
| AUC0-24 (ng⋅h/ml) | 24.82 (±14.31) | 56.17 (±28.27) | ||||
| Testosterone | Cmax (ng/ml) | 0.12 (±0.04)1 | 0.15 (±0.05) | AUC0-24 (ng⋅h/ml) | 2.58 (±0.94)1 | 2.79 (±0.94) |
| Estradiol | Cmax (pg/ml) | 3.33 (±1.31) | 5.04 (±2.68) | |||
| AUC0-24 (pg⋅h/ml) | 66.49 (±20.70) | 96.93 (±52.06) | ||||
1 N=8
Figure 1. Serum Concentrations of Prasterone (A), Testosterone (B), and Estradiol ==(C)== Measured Over a 24h Period on Day 7 Following Daily Administration of Placebo or Intrarosa (mean ± S.D.):
Distribution
The distribution of intravaginal (exogenous) prasterone is mainly local but some increase in systemic exposure is observed especially for the metabolites but within normal values.
Biotransformation
Exogenous prasterone is metabolized in the same manner as endogenous prasterone. Systemic metabolism has not been studied in this application.
Elimination
Systemic elimination has not been studied specifically for this application.
Preclinical safety data
Prasterone was not mutagenic or clastogenic in a standard battery of in vitro and in vivo studies.
Carcinogenic and reproductive and development toxicity studies were not performed.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.