JALYN Capsule Ref.[10461] Active ingredients: Dutasteride Tamsulosin
Source: FDA, National Drug Code (US) Revision Year: 2017
12.1. Mechanism of Action
JALYN is a combination of 2 drugs with different mechanisms of action to improve symptoms in patients with BPH: dutasteride, a 5-alpha-reductase inhibitor, and tamsulosin, an antagonist of alpha1A-adrenoreceptors.
Dutasteride
Dutasteride inhibits the conversion of testosterone to DHT. DHT is the androgen primarily responsible for the initial development and subsequent enlargement of the prostate gland. Testosterone is converted to DHT by the enzyme 5 alpha-reductase, which exists as 2 isoforms, type 1 and type 2. The type 2 isoenzyme is primarily active in the reproductive tissues, while the type 1 isoenzyme is also responsible for testosterone conversion in the skin and liver.
Dutasteride is a competitive and specific inhibitor of both type 1 and type 2 5-alpha-reductase isoenzymes, with which it forms a stable enzyme complex. Dissociation from this complex has been evaluated under in vitro and in vivo conditions and is extremely slow. Dutasteride does not bind to the human androgen receptor.
Tamsulosin
Smooth muscle tone is mediated by the sympathetic nervous stimulation of alpha1-adrenoceptors, which are abundant in the prostate, prostatic capsule, prostatic urethra, and bladder neck. Blockade of these adrenoceptors can cause smooth muscles in the bladder neck and prostate to relax, resulting in an improvement in urine flow rate and a reduction in symptoms of BPH.
Tamsulosin, an alpha1-adrenoceptor blocking agent, exhibits selectivity for alpha1-receptors in the human prostate. At least 3 discrete alpha1-adrenoceptor subtypes have been identified: alpha1A, alpha1B, and alpha1D; their distribution differs between human organs and tissue. Approximately 70% of the alpha1-receptors in human prostate are of the alpha1A subtype. Tamsulosin is not intended for use as an antihypertensive.
12.2. Pharmacodynamics
Dutasteride
Effect on 5 Alpha-Dihydrotestosterone and Testosterone
The maximum effect of daily doses of dutasteride on the reduction of DHT is dose-dependent and is observed within 1 to 2 weeks. After 1 and 2 weeks of daily dosing with dutasteride 0.5 mg, median serum DHT concentrations were reduced by 85% and 90%, respectively. In patients with BPH treated with dutasteride 0.5 mg/day for 4 years, the median decrease in serum DHT was 94% at 1 year, 93% at 2 years, and 95% at both 3 and 4 years. The median increase in serum testosterone was 19% at both 1 and 2 years, 26% at 3 years, and 22% at 4 years, but the mean and median levels remained within the physiologic range.
In patients with BPH treated with 5 mg/day of dutasteride or placebo for up to 12 weeks prior to transurethral resection of the prostate, mean DHT concentrations in prostatic tissue were significantly lower in the dutasteride group compared with placebo (784 and 5,793 pg/g, respectively, P <0.001). Mean prostatic tissue concentrations of testosterone were significantly higher in the dutasteride group compared with placebo (2,073 and 93 pg/g, respectively, P <0.001).
Adult males with genetically inherited type 2 5-alpha-reductase deficiency also have decreased DHT levels. These 5-alpha-reductase-deficient males have a small prostate gland throughout life and do not develop BPH. Except for the associated urogenital defects present at birth, no other clinical abnormalities related to 5-alpha-reductase deficiency have been observed in these individuals.
Effects on Other Hormones
In healthy volunteers, 52 weeks of treatment with dutasteride 0.5 mg/day (n=26) resulted in no clinically significant change compared with placebo (n=23) in sex hormone-binding globulin, estradiol, luteinizing hormone, follicle-stimulating hormone, thyroxine (free T4), and dehydroepiandrosterone. Statistically significant, baseline-adjusted mean increases compared with placebo were observed for total testosterone at 8 weeks (97.1 ng/dL, P <0.003) and thyroid-stimulating hormone at 52 weeks (0.4 mcIU/mL, P <0.05). The median percentage changes from baseline within the dutasteride group were 17.9% for testosterone at 8 weeks and 12.4% for thyroid-stimulating hormone at 52 weeks. After stopping dutasteride for 24 weeks, the mean levels of testosterone and thyroid-stimulating hormone had returned to baseline in the group of subjects with available data at the visit. In subjects with BPH treated with dutasteride in a large randomized, double-blind, placebo-controlled trial, there was a median percent increase in luteinizing hormone of 12% at 6 months and 19% at both 12 and 24 months.
Other Effects
Plasma lipid panel and bone mineral density were evaluated following 52 weeks of dutasteride 0.5 mg once daily in healthy volunteers. There was no change in bone mineral density as measured by dual energy x-ray absorptiometry compared with either placebo or baseline. In addition, the plasma lipid profile (i.e., total cholesterol, low density lipoproteins, high density lipoproteins, and triglycerides) was unaffected by dutasteride. No clinically significant changes in adrenal hormone responses to adrenocorticotropic hormone (ACTH) stimulation were observed in a subset population (n=13) of the 1-year healthy volunteer trial.
12.3. Pharmacokinetics
The pharmacokinetics of dutasteride and tamsulosin from JALYN are comparable to the pharmacokinetics of dutasteride and tamsulosin when administered separately.
Absorption
The pharmacokinetic parameters of dutasteride and tamsulosin observed after administration of JALYN in a single-dose, randomized, 3-period, partial cross-over trial are summarized in Table 2 below.
Table 2. Arithmetic Means (SD) of Serum Dutasteride and Tamsulosin in Single-dose Pharmacokinetic Parameters under Fed Conditions:
| Component | N | AUC(0-t) (ng h/mL) | Cmax (ng/mL) | Tmax (h)a | t½ (h) |
|---|---|---|---|---|---|
| Dutasteride | 92 | 39.6 (23.1) | 2.14 (0.77) | 3.00 (1.00-10.00) | |
| Tamsulosin | 92 | 187.2 (95.7) | 11.3 (4.44) | 6.00 (2.00-24.00) | 13.5 (3.92)b |
a Median (range).
b N=91.
Dutasteride: Following administration of a single 0.5-mg dose of a soft gelatin capsule, time to peak absolute bioavailability in 5 healthy subjects is approximately 60% (range: 40% to 94%).
Tamsulosin: Absorption of tamsulosin is essentially complete (>90%) following oral administration of 0.4-mg tamsulosin hydrochloride capsules under fasting conditions. Tamsulosin exhibits linear kinetics following single and multiple dosing, with achievement of steady-state concentrations by the fifth day of once-daily dosing.
Effect of Food
Food does not affect the pharmacokinetics of dutasteride following administration of JALYN. However, a mean 30% decrease in tamsulosin Cmax was observed when JALYN was administered with food, similar to that seen when tamsulosin monotherapy was administered under fed versus fasting conditions.
Distribution
Dutasteride: Pharmacokinetic data following single and repeat oral doses show that dutasteride has a large volume of distribution (300 to 500 L). Dutasteride is highly bound to plasma albumin (99.0%) and alpha-1 acid glycoprotein (AAG, 96.6%).
In a trial of healthy subjects (n=26) receiving dutasteride 0.5 mg/day for 12 months, semen dutasteride concentrations averaged 3.4 ng/mL (range: 0.4 to 14 ng/mL) at 12 months and, similar to serum, achieved steady-state concentrations at 6 months. On average, at 12 months 11.5% of serum dutasteride concentrations partitioned into semen.
Tamsulosin: The mean steady-state apparent volume of distribution of tamsulosin after intravenous administration to 10 healthy male adults was 16 L, which is suggestive of distribution into extracellular fluids in the body.
Tamsulosin is extensively bound to human plasma proteins (94% to 99%), primarily AAG, with linear binding over a wide concentration range (20 to 600 ng/mL). The results of 2-way in vitro studies indicate that the binding of tamsulosin to human plasma proteins is not affected by amitriptyline, diclofenac, glyburide, simvastatin plus simvastatin-hydroxy acid metabolite, warfarin, diazepam, or propranolol. Likewise, tamsulosin had no effect on the extent of binding of these drugs.
Metabolism
Dutasteride: Dutasteride is extensively metabolized in humans. In vitro studies showed that dutasteride is metabolized by the CYP3A4 and CYP3A5 isoenzymes. Both of these isoenzymes produced the 4′-hydroxydutasteride, 6-hydroxydutasteride, and the 6,4′-dihydroxydutasteride metabolites. In addition, the 15-hydroxydutasteride metabolite was formed by CYP3A4. Dutasteride is not metabolized in vitro by human cytochrome P450 isoenzymes CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, and CYP2E1. In human serum following dosing to steady state, unchanged dutasteride, 3 major metabolites (4′-hydroxydutasteride, 1,2-dihydrodutasteride, and 6-hydroxydutasteride), and 2 minor metabolites (6,4′-dihydroxydutasteride and 15-hydroxydutasteride), as assessed by mass spectrometric response, have been detected. The absolute stereochemistry of the hydroxyl additions in the 6 and 15 positions is not known. In vitro, the 4′-hydroxydutasteride and 1,2-dihydrodutasteride metabolites are much less potent than dutasteride against both isoforms of human 5α-reductase. The activity of 6β-hydroxydutasteride is comparable to that of dutasteride.
Tamsulosin: There is no enantiomeric bioconversion from tamsulosin [R(-) isomer] to the S(+) isomer in humans. Tamsulosin is extensively metabolized by cytochrome P450 enzymes in the liver and less than 10% of the dose is excreted in urine unchanged. However, the pharmacokinetic profile of the metabolites in humans has not been established. In vitro studies indicate that CYP3A4 and CYP2D6 are involved in metabolism of tamsulosin as well as some minor participation of other CYP isoenzymes. Inhibition of hepatic drug-metabolizing enzymes may lead to increased exposure to tamsulosin [see Drug Interactions (7.1)]. The metabolites of tamsulosin undergo extensive conjugation to glucuronide or sulfate prior to renal excretion.
Incubations with human liver microsomes showed no evidence of clinically significant metabolic interactions between tamsulosin and amitriptyline, albuterol, glyburide, and finasteride. However, results of the in vitro testing of the tamsulosin interaction with diclofenac and warfarin were equivocal.
Excretion
Dutasteride: Dutasteride and its metabolites were excreted mainly in feces. As a percent of dose, there was approximately 5% unchanged dutasteride (approximately 1% to approximately 15%) and 40% as dutasteride-related metabolites (approximately 2% to approximately 90%). Only trace amounts of unchanged dutasteride were found in urine (<1%). Therefore, on average, the dose unaccounted for approximated 55% (range: 5% to 97%). The terminal elimination half-life of dutasteride is approximately 5 weeks at steady state. The average steady-state serum dutasteride concentration was 40 ng/mL following 0.5 mg/day for 1 year. Following daily dosing, dutasteride serum concentrations achieve 65% of steady-state concentration after 1 month and approximately 90% after 3 months. Due to the long half-life of dutasteride, serum concentrations remain detectable (greater than 0.1 ng/mL) for up to 4 to 6 months after discontinuation of treatment.
Tamsulosin: On administration of the radiolabeled dose of tamsulosin to 4 healthy volunteers, 97% of the administered radioactivity was recovered, with urine (76%) representing the primary route of excretion compared with feces (21%) over 168 hours.
Following intravenous or oral administration of an immediate-release formulation, the elimination half-life of tamsulosin in plasma ranges from 5 to 7 hours. Because of absorption rate-controlled pharmacokinetics with tamsulosin hydrochloride capsules, the apparent half-life of tamsulosin is approximately 9 to 13 hours in healthy volunteers and 14 to 15 hours in the target population.
Tamsulosin undergoes restrictive clearance in humans, with a relatively low systemic clearance (2.88 L/h).
Specific Populations
Pediatric: The pharmacokinetics of dutasteride and tamsulosin administered together have not been investigated in subjects younger than 18 years.
Geriatric: Dutasteride and tamsulosin pharmacokinetics using JALYN have not been studied in geriatric patients. The following text reflects information for the individual components.
Dutasteride: No dosage adjustment is necessary in the elderly. The pharmacokinetics and pharmacodynamics of dutasteride were evaluated in 36 healthy male subjects aged between 24 and 87 years following administration of a single 5-mg dose of dutasteride. In this single-dose trial, dutasteride half-life increased with age (approximately 170 hours in men aged 20 to 49 years, approximately 260 hours in men aged 50 to 69 years, and approximately 300 hours in men older than 70 years).
Tamsulosin: Cross-study comparison of tamsulosin overall exposure (AUC) and half-life indicate that the pharmacokinetic disposition of tamsulosin may be slightly prolonged in geriatric males compared with young, healthy male volunteers. Intrinsic clearance is independent of tamsulosin binding to AAG, but diminishes with age, resulting in a 40% overall higher exposure (AUC) in subjects aged 55 to 75 years compared with subjects aged 20 to 32 years.
Gender: Dutasteride: Dutasteride is contraindicated in pregnancy and women of childbearing potential and is not indicated for use in other women [see Contraindications (4), Warnings and Precautions (5.6)]. The pharmacokinetics of dutasteride in women have not been studied.
Tamsulosin: Tamsulosin is not indicated for use in women. No information is available on the pharmacokinetics of tamsulosin in women.
Race: The effect of race on pharmacokinetics of dutasteride and tamsulosin administered together or separately has not been studied.
Renal Impairment: The effect of renal impairment on dutasteride and tamsulosin pharmacokinetics has not been studied using JALYN. The following text reflects information for the individual components.
Dutasteride: The effect of renal impairment on dutasteride pharmacokinetics has not been studied. However, less than 0.1% of a steady-state 0.5-mg dose of dutasteride is recovered in human urine, so no adjustment in dosage is anticipated for patients with renal impairment.
Tamsulosin: The pharmacokinetics of tamsulosin have been compared in 6 subjects with mild-moderate (30≤ CLcr <70 mL/min/1.73 m 2) or moderate-severe (10≤ CLcr <30 mL/min/1.73 m 2) renal impairment and 6 normal subjects (CLcr >90 mL/min/1.73 m 2). While a change in the overall plasma concentration of tamsulosin was observed as the result of altered binding to AAG, the unbound (active) concentration of tamsulosin, as well as the intrinsic clearance, remained relatively constant. Therefore, patients with renal impairment do not require an adjustment in tamsulosin dosing. However, patients with end-stage renal disease (CLcr <10 mL/min/1.73 m 2) have not been studied.
Hepatic Impairment: The effect of hepatic impairment on dutasteride and tamsulosin pharmacokinetics has not been studied using JALYN. The following text reflects information available for the individual components.
Dutasteride: The effect of hepatic impairment on dutasteride pharmacokinetics has not been studied. Because dutasteride is extensively metabolized, exposure could be higher in hepatically impaired patients.
Tamsulosin: The pharmacokinetics of tamsulosin have been compared in 8 subjects with moderate hepatic impairment (Child-Pugh classification: Grades A and B) and 8 normal subjects. While a change in the overall plasma concentration of tamsulosin was observed as the result of altered binding to AAG, the unbound (active) concentration of tamsulosin does not change significantly with only a modest (32%) change in intrinsic clearance of unbound tamsulosin. Therefore, patients with moderate hepatic impairment do not require an adjustment in tamsulosin dosage. Tamsulosin has not been studied in patients with severe hepatic impairment.
Drug Interactions
There have been no drug interaction studies using JALYN. The following text reflects information available for the individual components.
Cytochrome P450 Inhibitors: Dutasteride: No clinical drug interaction trials have been performed to evaluate the impact of CYP3A enzyme inhibitors on dutasteride pharmacokinetics. However, based on in vitro data, blood concentrations of dutasteride may increase in the presence of inhibitors of CYP3A4/5 such as ritonavir, ketoconazole, verapamil, diltiazem, cimetidine, troleandomycin, and ciprofloxacin.
Dutasteride does not inhibit the in vitro metabolism of model substrates for the major human cytochrome P450 isoenzymes (CYP1A2, CYP2C9, CYP2C19, CYP2D6, and CYP3A4) at a concentration of 1,000 ng/mL, 25 times greater than steady-state serum concentrations in humans.
Tamsulosin: Strong and Moderate Inhibitors of CYP3A4 or CYP2D6: The effects of ketoconazole (a strong inhibitor of CYP3A4) at 400 mg once daily for 5 days on the pharmacokinetics of a single tamsulosin hydrochloride capsule 0.4-mg dose was investigated in 24 healthy volunteers (age range: 23 to 47 years). Concomitant treatment with ketoconazole resulted in increases in the Cmax and AUC of tamsulosin by factors of 2.2 and 2.8, respectively. The effects of concomitant administration of a moderate CYP3A4 inhibitor (e.g., erythromycin) on the pharmacokinetics of tamsulosin have not been evaluated.
The effects of paroxetine (a strong inhibitor of CYP2D6) at 20 mg once daily for 9 days on the pharmacokinetics of a single tamsulosin capsule 0.4-mg dose was investigated in 24 healthy volunteers (age range: 23 to 47 years). Concomitant treatment with paroxetine resulted in increases in the Cmax and AUC of tamsulosin by factors of 1.3 and 1.6, respectively. A similar increase in exposure is expected in poor metabolizers (PM) of CYP2D6 as compared with extensive metabolizers (EM). A fraction of the population (about 7% of whites and 2% of African-Americans) are CYP2D6 PMs. Since CYP2D6 PMs cannot be readily identified and the potential for significant increase in tamsulosin exposure exists when tamsulosin 0.4 mg is coadministered with strong CYP3A4 inhibitors in CYP2D6 PMs, tamsulosin 0.4-mg capsules should not be used in combination with strong inhibitors of CYP3A4 (e.g., ketoconazole).
The effects of concomitant administration of a moderate CYP2D6 inhibitor (e.g., terbinafine) on the pharmacokinetics of tamsulosin have not been evaluated.
The effects of coadministration of both a CYP3A4 and a CYP2D6 inhibitor with tamsulosin capsules have not been evaluated. However, there is a potential for significant increase in tamsulosin exposure when tamsulosin 0.4 mg is coadministered with a combination of both CYP3A4 and CYP2D6 inhibitors.
Cimetidine: The effects of cimetidine at the highest recommended dose (400 mg every 6 hours for 6 days) on the pharmacokinetics of a single tamsulosin capsule 0.4-mg dose was investigated in 10 healthy volunteers (age range: 21 to 38 years). Treatment with cimetidine resulted in a significant decrease (26%) in the clearance of tamsulosin hydrochloride, which resulted in a moderate increase in tamsulosin hydrochloride AUC (44%).
Alpha-adrenergic Antagonists: Dutasteride: In a single-sequence, crossover trial in healthy volunteers, the administration of tamsulosin or terazosin in combination with dutasteride had no effect on the steady-state pharmacokinetics of either alpha-adrenergic antagonist. Although the effect of administration of tamsulosin or terazosin on dutasteride pharmacokinetic parameters was not evaluated, the percent change in DHT concentrations was similar for dutasteride, alone or in combination with tamsulosin or terazosin.
Warfarin: Dutasteride: In a trial of 23 healthy volunteers, 3 weeks of treatment with dutasteride 0.5 mg/day did not alter the steady-state pharmacokinetics of the S- or R-warfarin isomers or alter the effect of warfarin on prothrombin time when administered with warfarin.
Tamsulosin: A definitive drug-drug interaction trial between tamsulosin and warfarin was not conducted. Results from limited in vitro and in vivo studies are inconclusive. Therefore, caution should be exercised with concomitant administration of warfarin and tamsulosin.
Nifedipine, Atenolol, Enalapril: Tamsulosin: In 3 trials in hypertensive subjects (age range: 47 to 79 years) whose blood pressure was controlled with stable doses of nifedipine extended-release, atenolol, or enalapril for at least 3 months, tamsulosin hydrochloride capsules 0.4 mg for 7 days followed by tamsulosin hydrochloride capsules 0.8 mg for another 7 days (n=8 per trial) resulted in no clinically significant effects on blood pressure and pulse rate compared with placebo (n=4 per trial). Therefore, dosage adjustments are not necessary when tamsulosin is administered concomitantly with nifedipine extended-release, atenolol, or enalapril.
Digoxin and Theophylline: Dutasteride: In a trial of 20 healthy volunteers, dutasteride did not alter the steady-state pharmacokinetics of digoxin when administered concomitantly at a dose of 0.5 mg/day for 3 weeks.
Tamsulosin: In 2 trials in healthy volunteers (n=10 per trial; age range: 19 to 39 years) receiving tamsulosin capsules 0.4 mg/day for 2 days, followed by tamsulosin capsules 0.8 mg/day for 5 to 8 days, single intravenous doses of digoxin 0.5 mg or theophylline 5 mg/kg resulted in no change in the pharmacokinetics of digoxin or theophylline. Therefore, dosage adjustments are not necessary when a tamsulosin capsule is administered concomitantly with digoxin or theophylline.
Furosemide: Tamsulosin: The pharmacokinetic and pharmacodynamic interaction between tamsulosin hydrochloride capsules 0.8 mg/day (steady-state) and furosemide 20 mg intravenously (single dose) was evaluated in 10 healthy volunteers (age range: 21 to 40 years). Tamsulosin had no effect on the pharmacodynamics (excretion of electrolytes) of furosemide. While furosemide produced an 11% to 12% reduction in tamsulosin Cmax and AUC, these changes are expected to be clinically insignificant and do not require dose adjustment for tamsulosin.
Calcium Channel Antagonists: Dutasteride: In a population pharmacokinetics analysis, a decrease in clearance of dutasteride was noted when coadministered with the CYP3A4 inhibitors verapamil (-37%, n=6) and diltiazem (-44%, n=5). In contrast, no decrease in clearance was seen when amlodipine, another calcium channel antagonist that is not a CYP3A4 inhibitor, was coadministered with dutasteride (+7%, n=4). The decrease in clearance and subsequent increase in exposure to dutasteride in the presence of verapamil and diltiazem is not considered to be clinically significant. No dosage adjustment is recommended.
Cholestyramine: Dutasteride: Administration of a single 5-mg dose of dutasteride followed 1 hour later by 12 g cholestyramine did not affect the relative bioavailability of dutasteride in 12 normal volunteers.
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
No non-clinical studies have been conducted with JALYN. The following information is based on studies performed with dutasteride or tamsulosin.
Carcinogenesis
Dutasteride
A 2-year carcinogenicity study was conducted in B6C3F1 mice at doses of 3, 35, 250, and 500 mg/kg/day for males and 3, 35, and 250 mg/kg/day for females; an increased incidence of benign hepatocellular adenomas was noted at 250 mg/kg/day (290-fold the MRHD of a 0.5-mg daily dose) in female mice only. Two of the 3 major human metabolites have been detected in mice. The exposure to these metabolites in mice is either lower than in humans or is not known.
In a 2-year carcinogenicity study in Han Wistar rats, at doses of 1.5, 7.5, and 53 mg/kg/day in males and 0.8, 6.3, and 15 mg/kg/day in females, there was an increase in Leydig cell adenomas in the testes at 135-fold the MRHD (53 mg/kg/day and greater). An increased incidence of Leydig cell hyperplasia was present at 52-fold the MRHD (male rat doses of 7.5 mg/kg/day and greater). A positive correlation between proliferative changes in the Leydig cells and an increase in circulating luteinizing hormone levels has been demonstrated with 5-alpha-reductase inhibitors and is consistent with an effect on the hypothalamic-pituitary-testicular axis following 5-alpha-reductase inhibition. At tumorigenic doses, luteinizing hormone levels in rats were increased by 167%. In this study, the major human metabolites were tested for carcinogenicity at approximately 1 to 3 times the expected clinical exposure.
Tamsulosin
In a rat carcinogenicity assay, no increases in tumor incidence was observed in rats administered up to 3 times the MRHD of 0.8 mg/day (based on AUC of animal doses up to 43 mg/kg/day in males and up to 52 mg/kg/day in females), with the exception of a modest increase in the frequency of mammary gland fibroadenomas in female rats receiving doses of 5.4 mg/kg or greater.
In a carcinogenicity assay, mice were administered up to 8 times the MRHD of tamsulosin (oral doses up to 127 mg/kg/day in males and 158 mg/kg/day in females). There were no significant tumor findings in male mice. Female mice treated for 2 years with the 2 highest doses of 45 and 158 mg/kg/day had statistically significant increases in the incidence of mammary gland fibroadenomas (P <0.0001) and adenocarcinomas.
The increased incidences of mammary gland neoplasms in female rats and mice were considered secondary to tamsulosin-induced hyperprolactinemia. It is not known if tamsulosin elevates prolactin in humans. The relevance for human risk of the findings of prolactin-mediated endocrine tumors in rodents is not known.
Mutagenesis
Dutasteride
Dutasteride was tested for genotoxicity in a bacterial mutagenesis assay (Ames test), a chromosomal aberration assay in Chinese hamster ovary (CHO) cells, and a micronucleus assay in rats. The results did not indicate any genotoxic potential of the parent drug. Two major human metabolites were also negative in either the Ames test or an abbreviated Ames test.
Tamsulosin
Tamsulosin produced no evidence of mutagenic potential in vitro in the Ames reverse mutation test, mouse lymphoma thymidine kinase assay, unscheduled DNA repair synthesis assay, and chromosomal aberration assays in CHO cells or human lymphocytes. There were no mutagenic effects in the in vivo sister chromatid exchange and mouse micronucleus assay.
Impairment of Fertility
Dutasteride
Treatment of sexually mature male rats with dutasteride at 0.1- to 110-fold the MRHD (animal doses of 0.05, 10, 50, and 500 mg/kg/day for up to 31 weeks) resulted in dose- and time-dependent decreases in fertility; reduced cauda epididymal (absolute) sperm counts but not sperm concentration (at 50 and 500 mg/kg/day); reduced weights of the epididymis, prostate, and seminal vesicles; and microscopic changes in the male reproductive organs. The fertility effects were reversed by recovery week 6 at all doses, and sperm counts were normal at the end of a 14-week recovery period. The 5-alpha-reductase–related changes consisted of cytoplasmic vacuolation of tubular epithelium in the epididymides and decreased cytoplasmic content of epithelium, consistent with decreased secretory activity in the prostate and seminal vesicles. The microscopic changes were no longer present at recovery week 14 in the low-dose group and were partly recovered in the remaining treatment groups. Low levels of dutasteride (0.6 to 17 ng/mL) were detected in the serum of untreated female rats mated to males dosed at 10, 50, or 500 mg/kg/day for 29 to 30 weeks.
In a fertility study in female rats, oral administration of dutasteride at doses of 0.05, 2.5, 12.5, and 30 mg/kg/day resulted in reduced litter size, increased embryo resorption and feminization of male fetuses (decreased anogenital distance) at 2- to 10-fold the MRHD (animal doses of 2.5 mg/kg/day or greater). Fetal body weights were also reduced at less than 0.02-fold the MRHD in rats (0.5 mg/kg/day).
Tamsulosin
Studies in rats revealed significantly reduced fertility in males at approximately 50 times the MRHD based on AUC (single or multiple daily doses of 300 mg/kg/day of tamsulosin hydrochloride). The mechanism of decreased fertility in male rats is considered to be an effect of the compound on the vaginal plug formation possibly due to changes of semen content or impairment of ejaculation. The effects on fertility were reversible showing improvement by 3 days after a single dose and 4 weeks after multiple dosing. Effects on fertility in males were completely reversed within nine weeks of discontinuation of multiple dosing. Multiple doses of 0.2 and 16 times the MRHD (animal doses of 10 and 100 mg/kg/day tamsulosin hydrochloride) did not significantly alter fertility in male rats. Effects of tamsulosin on sperm counts or sperm function have not been evaluated.
Studies in female rats revealed significant reductions in fertility after single or multiple dosing with 300 mg/kg/day of the R-isomer or racemic mixture of tamsulosin hydrochloride, respectively. In female rats, the reductions in fertility after single doses were considered to be associated with impairments in fertilization. Multiple dosing with 10 or 100 mg/kg/day of the racemic mixture did not significantly alter fertility in female rats.
Estimates of exposure multiples comparing animal studies with the MRHD for dutasteride are based on clinical serum concentration at steady state.
Estimates of exposure multiples comparing animal studies with the MRHD for tamsulosin are based on AUC.
13.2. Animal Toxicology and/or Pharmacology
Central Nervous System Toxicology Studies
Dutasteride
In rats and dogs, repeated oral administration of dutasteride resulted in some animals showing signs of non-specific, reversible, centrally-mediated toxicity without associated histopathological changes at exposures 425- and 315-fold the expected clinical exposure (of parent drug), respectively.
14. Clinical Studies
The trial supporting the efficacy of JALYN was a 4-year multicenter, randomized, double-blind, parallel-group trial (CombAT trial) investigating the efficacy of the coadministration of dutasteride 0.5 mg/day and tamsulosin hydrochloride 0.4 mg/day (n=1,610) compared with dutasteride alone (n=1,623) or tamsulosin alone (n=1,611). Subjects were at least 50 years of age with a serum PSA ≥1.5 ng/mL and <10 ng/mL and BPH diagnosed by medical history and physical examination, including enlarged prostate (≥30 cc) and BPH symptoms that were moderate to severe according to the International Prostate Symptom Score (IPSS). Eighty-eight percent (88%) of the enrolled trial population was white. Approximately 52% of subjects had previous exposure to 5-alpha-reductase inhibitor or alpha-adrenergic antagonist treatment. Of the 4,844 subjects randomly assigned to receive treatment, 69% of subjects in the coadministration group, 67% in the dutasteride group, and 61% in the tamsulosin group completed 4 years of double-blind treatment.
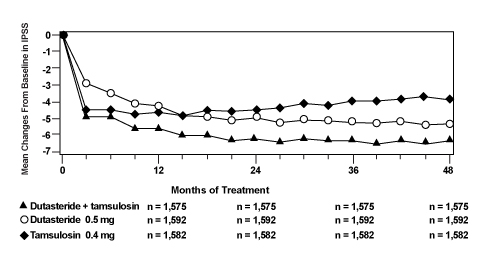
Effect on Symptom Score
Symptoms were quantified using the first 7 questions of the International Prostate Symptom Score (IPSS). The baseline score was approximately 16.4 units for each treatment group. Coadministration therapy was statistically superior to each of the monotherapy treatments in decreasing symptom score at Month 24, the primary time point for this endpoint. At Month 24, the mean changes from baseline (±SD) in IPSS total symptom scores were -6.2 (±7.14) for the coadministration group, -4.9 (±6.81) for dutasteride, and -4.3 (±7.01) for tamsulosin, with a mean difference between coadministration and dutasteride of -1.3 units (P <0.001; [95% CI: -1.69, -0.86]), and between coadministration and tamsulosin of -1.8 units (P <0.001; [95% CI: -2.23, -1.40]). A significant difference was seen by Month 9 and continued through Month 48. At Month 48 the mean changes from baseline (±SD) in IPSS total symptom scores were -6.3 (±7.40) for coadministration, -5.3 (±7.14) for dutasteride, and -3.8 (±7.74) for tamsulosin, with a mean difference between coadministration and dutasteride of -0.96 units (P <0.001; [95% CI: -1.40, -0.52]), and between coadministration and tamsulosin of -2.5 units (P <0.001; [95% CI: -2.96, -2.07]). See Figure 1.
Figure 1. International Prostate Symptom Score Change from Baseline over a 48-Month Period (Randomized, Double-blind, Parallel-group Trial [CombAT Trial]):
Effect on Acute Urinary Retention (AUR) or the Need for BPH-related Surgery
After 4 years of treatment, coadministration therapy with dutasteride and tamsulosin did not provide benefit over dutasteride monotherapy in reducing the incidence of AUR or BPH-related surgery.
In separate 2-year randomized, double-blind trials, compared with placebo, dutasteride monotherapy was associated with a statistically significantly lower incidence of AUR (1.8% for dutasteride versus 4.2% for placebo; 57% reduction in risk) and with a statistically significantly lower incidence of BPH-related surgery (2.2% for dutasteride versus. 4.1% for placebo; 48% reduction in risk).
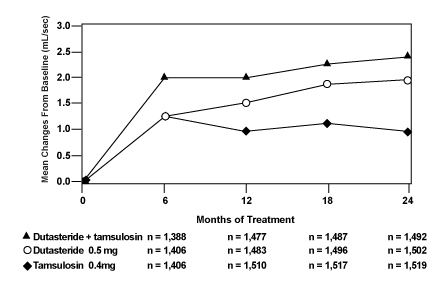
Effect on Maximum Urine Flow Rate
The baseline Qmax was approximately 10.7 mL/sec for each treatment group. Coadministration therapy was statistically superior to each of the monotherapy treatments in increasing Qmax at Month 24, the primary time point for this endpoint. At Month 24, the mean increases from baseline (±SD) in Qmax were 2.4 (±5.26) mL/sec for coadministration group, 1.9 (±5.10) mL/sec for dutasteride, and 0.9 (±4.57) mL/sec for tamsulosin, with a mean difference between coadministration and dutasteride of 0.5 mL/sec (P=0.003; [95% CI: 0.17, 0.84]), and between coadministration and tamsulosin of 1.5 mL/sec (P <0.001; [95% CI: 1.19, 1.86]). This difference was seen by Month 6 and continued through Month 24. See Figure 2.
The additional improvement in Qmax of coadministration therapy over dutasteride monotherapy was no longer statistically significant at Month 48.
Figure 2. Qmax Change from Baseline over a 24-Month Period (Randomized, Double-blind, Parallel-group Trial [CombAT Trial]):
Effect on Prostate Volume
The mean prostate volume at trial entry was approximately 55 cc. At Month 24, the primary time point for this endpoint, the mean percent changes from baseline (±SD) in prostate volume were -26.9% (±22.57) for coadministration therapy, -28.0% (±24.88) for dutasteride, and 0% (±31.14) for tamsulosin, with a mean difference between coadministration and dutasteride of 1.1% (P=NS; [95% CI: -0.6, 2.8]), and between coadministration and tamsulosin of -26.9% (P <0.001; [95% CI: -28.9, -24.9]). Similar changes were seen at Month 48: -27.3% (±24.91) for coadministration therapy, -28.0% (±25.74) for dutasteride, and +4.6% (±35.45) for tamsulosin.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.