PLETAL Tablet Ref.[49792] Active ingredients: Cilostazol
Source: FDA, National Drug Code (US) Revision Year: 2017
12.1. Mechanism of Action
PLETAL and several of its metabolites inhibit phosphodiesterase III activity and suppress cAMP degradation with a resultant increase in cAMP in platelets and blood vessels, leading to inhibition of platelet aggregation and vasodilation, respectively.
PLETAL reversibly inhibits platelet aggregation induced by a variety of stimuli, including thrombin, ADP, collagen, arachidonic acid, epinephrine, and shear stress.
Cardiovascular effects
Cilostazol affects both vascular beds and cardiovascular function. It produces heterogeneous dilation of vascular beds, with greater dilation in femoral beds than in vertebral, carotid or superior mesenteric arteries. Renal arteries were not responsive to the effects of cilostazol.
In dogs or cynomolgus monkeys, cilostazol increased heart rate, myocardial contractile force, and coronary blood flow as well as ventricular automaticity, as would be expected for a PDE III inhibitor. Left ventricular contractility was increased at doses required to inhibit platelet aggregation. A-V conduction was accelerated. In humans, heart rate increased in a dose-proportional manner by a mean of 5.1 and 7.4 beats per minute in patients treated with 50 and 100 mg twice daily, respectively.
12.2. Pharmacodynamics
Cilostazol's effects on platelet aggregation were evaluated in both healthy subjects and in patients with stable symptoms of cerebral thrombosis, cerebral embolism, transient ischemic attack, or cerebral arteriosclerosis over a range of doses from 50 mg every day to 100 mg three times a day. Cilostazol significantly inhibited platelet aggregation in a dose-dependent manner. The effects were observed as early as 3 hours post-dose and lasted up to 12 hours following a single dose. Following chronic administration and withdrawal of cilostazol, the effects on platelet aggregation began to subside 48 hours after withdrawal and returned to baseline by 96 hours with no rebound effect. A cilostazol dosage of 100 mg twice daily consistently inhibited platelet aggregation induced with arachidonic acid, collagen and adenosine diphosphate (ADP). Bleeding time was not affected by cilostazol administration.
Effects on circulating plasma lipids have been examined in patients taking PLETAL. After 12 weeks, as compared to placebo, PLETAL 100 mg twice daily produced a reduction in triglycerides of 29.3 mg/dL (15%) and an increase in HDLcholesterol of 4.0 mg/dL (≅ 10%).
Drug Interactions
Aspirin
Short-term (less than or equal to 4 days) coadministration of aspirin with PLETAL increased the inhibition of ADPinduced ex vivo platelet aggregation by 22% - 37% when compared to either aspirin or PLETAL alone. Short-term (less than or equal to 4 days) coadministration of aspirin with PLETAL increased the inhibition of arachidonic acid-induced ex vivo platelet aggregation by 20% compared to PLETAL alone and by 48% compared to aspirin alone. However, shortterm coadministration of aspirin with PLETAL had no clinically significant impact on PT, aPTT, or bleeding time compared to aspirin alone. Effects of long-term coadministration in the general population are unknown.
In eight randomized, placebo-controlled, double-blind clinical trials, aspirin was coadministered with cilostazol to 201 patients. The most frequent doses and mean durations of aspirin therapy were 75-81 mg daily for 137 days (107 patients) and 325 mg daily for 54 days (85 patients). There was no apparent increase in frequency of hemorrhagic adverse effects in patients taking cilostazol and aspirin compared to patients taking placebo and equivalent doses of aspirin.
Warfarin
Cilostazol did not inhibit the pharmacologic effects (PT, aPTT, bleeding time, or platelet aggregation) of R- and S-warfarin after a single 25-mg dose of warfarin. The effect of concomitant multiple dosing of warfarin and PLETAL on the pharmacodynamics of both drugs is unknown.
12.3. Pharmacokinetics
PLETAL is absorbed after oral administration. A high fat meal increases absorption, with an approximately 90% increase in Cmax and a 25% increase in AUC. Absolute bioavailability is not known. Cilostazol is extensively metabolized by hepatic cytochrome P-450 enzymes, mainly 3A4, and, to a lesser extent, 2C19, with metabolites largely excreted in urine. Two metabolites are active, with one metabolite appearing to account for at least 50% of the pharmacologic (PDE III inhibition) activity after administration of PLETAL.
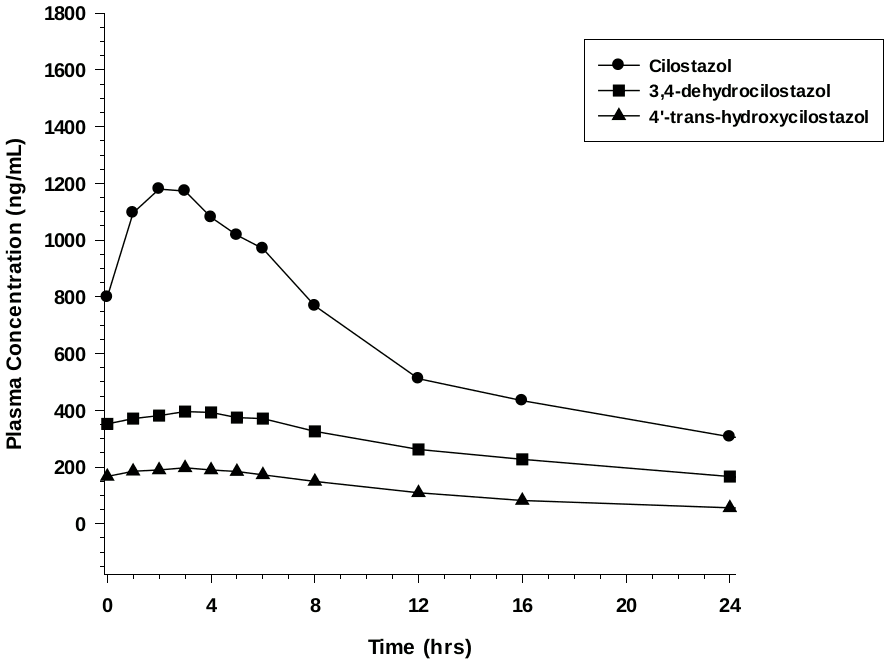
Pharmacokinetics are approximately dose proportional. Cilostazol and its active metabolites have apparent elimination half-lives of about 11-13 hours. Cilostazol and its active metabolites accumulate about 2-fold with chronic administration and reach steady state blood levels within a few days. The pharmacokinetics of cilostazol and its two major active metabolites were similar in healthy subjects and patients with intermittent claudication due to peripheral arterial disease (PAD). Figure 1 shows the mean plasma concentration-time profile at steady state after multiple dosing of PLETAL 100 mg twice daily.
Figure 1. Mean Plasma Concentration-time Profile at Steady State after Multiple Dosing of PLETAL 100 mg Twice Daily:
Distribution
Cilostazol is 95-98% protein bound, predominantly to albumin. The binding for 3,4-dehydro-cilostazol is 97.4% and for 4´-trans-hydroxy-cilostazol is 66%. Mild hepatic impairment did not affect protein binding. The free fraction of cilostazol was 27% higher in subjects with renal impairment than in healthy volunteers. The displacement of cilostazol from plasma proteins by erythromycin, quinidine, warfarin, and omeprazole was not clinically significant.
Metabolism
Cilostazol is eliminated predominantly by metabolism and subsequent urinary excretion of metabolites. Based on in vitro studies, the primary isoenzymes involved in cilostazol's metabolism are CYP3A4 and, to a lesser extent, CYP2C19. The enzyme responsible for metabolism of 3,4-dehydro-cilostazol, the most active of the metabolites, is unknown.
Following oral administration of 100 mg radiolabeled cilostazol, 56% of the total analytes in plasma was cilostazol, 15% was 3,4-dehydro-cilostazol (4-7 times as active as cilostazol), and 4% was 4´-trans-hydroxy-cilostazol (20% as active as cilostazol).
Elimination
The primary route of elimination was via the urine (74%), with the remainder excreted in feces (20%). No measurable amount of unchanged cilostazol was excreted in the urine, and less than 2% of the dose was excreted as 3,4-dehydrocilostazol. About 30% of the dose was excreted in urine as 4´-trans-hydroxy-cilostazol. The remainder was excreted as other metabolites, none of which exceeded 5%. There was no evidence of induction of hepatic microenzymes.
Special Populations
Age and Gender
The total and unbound oral clearances, adjusted for body weight, of cilostazol and its metabolites were not significantly different with respect to age (50 to 80 years) or gender.
Smokers
Population pharmacokinetic analysis suggests that smoking decreased cilostazol exposure by about 20%.
Hepatic Impairment
The pharmacokinetics of cilostazol and its metabolites were similar in subjects with mild hepatic disease as compared to healthy subjects.
Patients with moderate or severe hepatic impairment have not been studied.
Renal Impairment
The total pharmacologic activity of cilostazol and its metabolites was similar in subjects with mild to moderate renal impairment and in healthy subjects. Severe renal impairment increases metabolite levels and alters protein binding of the parent. The expected pharmacologic activity, however, based on plasma concentrations and relative PDE III inhibiting potency of parent drug and metabolites, appeared little changed. Patients on dialysis have not been studied, but, it is unlikely that cilostazol can be removed efficiently by dialysis because of its high protein binding (95-98%).
Drug Interactions
Cilostazol does not appear to inhibit CYP3A4.
Warfarin
Cilostazol did not inhibit the metabolism of R- and S-warfarin after a single 25-mg dose of warfarin.
Clopidogrel
Multiple doses of clopidogrel do not significantly increase steady state plasma concentrations of cilostazol.
Strong Inhibitors of CYP3A4
A priming dose of ketoconazole 400 mg (a strong inhibitor of CYP3A4), was given one day prior to coadministration of single doses of ketoconazole 400 mg and cilostazol 100 mg. This regimen increased cilostazol Cmax by 94% and AUC by 117%. Other strong inhibitors of CYP3A4, such as itraconazole, voriconazole, clarithromycin, ritonavir, saquinavir, and nefazodone would be expected to have a similar effect [see Dosage and Administration (2.2), Drug Interactions (7.1)].
Moderate Inhibitors of CYP3A4
Erythromycin and other macrolide antibiotics: Erythromycin is a moderately strong inhibitor of CYP3A4. Coadministration of erythromycin 500 mg every 8h with a single dose of cilostazol 100 mg increased cilostazol Cmax by 47% and AUC by 73%. Inhibition of cilostazol metabolism by erythromycin increased the AUC of 4´-trans-hydroxycilostazol by 141% [see Dosage and Administration (2.2)].
Diltiazem
Diltiazem 180 mg decreased the clearance of cilostazol by ~30%. Cilostazol Cmax increased ~30% and AUC increased ~40% [see Dosage and Administration (2.2)].
Grapefruit Juice
Grapefruit juice increased the Cmax of cilostazol by ~50%, but had no effect on AUC.
Inhibitors of CYP2C19
Omeprazole: Coadministration of omeprazole did not significantly affect the metabolism of cilostazol, but the systemic exposure to 3,4-dehydro-cilostazol was increased by 69%, probably the result of omeprazole's potent inhibition of CYP2C19 [see Dosage and Administration (2.2)].
Quinidine
Concomitant administration of quinidine with a single dose of cilostazol 100 mg did not alter cilostazol pharmacokinetics.
Lovastatin
The concomitant administration of lovastatin with cilostazol decreases cilostazol Css,max and AUCτ by 15%. There is also a decrease, although nonsignificant, in cilostazol metabolite concentrations. Coadministration of cilostazol with lovastatin increases lovastatin and β-hydroxylovastatin AUC approximately 70% and is not expected to be clinically significant.
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Dietary administration of cilostazol to male and female rats and mice for up to 104 weeks, at doses up to 500 mg/kg/day in rats and 1000 mg/kg/day in mice, revealed no evidence of carcinogenic potential. The maximum doses administered in both rat and mouse studies were, on a systemic exposure basis, less than the human exposure at the MRHD of the drug. Cilostazol tested negative in bacterial gene mutation, bacterial DNA repair, mammalian cell gene mutation, and mouse in vivo bone marrow chromosomal aberration assays. It was, however, associated with a significant increase in chromosomal aberrations in the in vitro Chinese Hamster Ovary Cell assay.
In female mice, cilostazol caused a reversible contraceptive effect at a dose (300 mg/kg) that was approximately 7.4-fold greater than the Maximum Recommended Human Dose (MRHD) on a body surface area basis. These findings have not been demonstrated in other animal species.
Cilostazol did not affect fertility or mating performance of male and female rats at doses as high as 1000 mg/kg/day. At this dose, systemic exposures (AUCs) to unbound cilostazol were less than 1.5 times in males, and about 5 times in females, the exposure in humans at the MRHD.
13.2. Animal Toxicology and/or Pharmacology
Repeated oral administration of cilostazol to dogs (30 or more mg/kg/day for 52 weeks, 150 or more mg/kg/day for 13 weeks, and 450 mg/kg/day for 2 weeks), produced cardiovascular lesions that included endocardial hemorrhage, hemosiderin deposition and fibrosis in the left ventricle, hemorrhage in the right atrial wall, hemorrhage and necrosis of the smooth muscle in the wall of the coronary artery, intimal thickening of the coronary artery, and coronary arteritis and periarteritis. At the lowest dose associated with cardiovascular lesions in the 52-week study, systemic exposure (AUC) to unbound cilostazol was less than that seen in humans at the maximum recommended human dose (MRHD) of 100 mg twice daily. Similar lesions have been reported in dogs following the administration of other positive inotropic agents (including PDE III inhibitors) and/or vasodilating agents. No cardiovascular lesions were seen in rats following 5 or 13 weeks of administration of cilostazol at doses up to 1500 mg/kg/day. At this dose, systemic exposures (AUCs) to unbound cilostazol were only about 1.5 and 5 times (male and female rats, respectively) the exposure seen in humans at the MRHD. Cardiovascular lesions were also not seen in rats following 52 weeks of administration of cilostazol at doses up to 150 mg/kg/day. At this dose, systemic exposures (AUCs) to unbound cilostazol were about 0.5 and 5 times (male and female rats, respectively) the exposure in humans at the MRHD. In female rats, cilostazol AUCs were similar at 150 and 1500 mg/kg/day. Cardiovascular lesions were also not observed in monkeys after oral administration of cilostazol for 13 weeks at doses up to 1800 mg/kg/day. While this dose of cilostazol produced pharmacologic effects in monkeys, plasma cilostazol levels were less than those seen in humans given the MRHD, and those seen in dogs given doses associated with cardiovascular lesions.
14. Clinical Studies
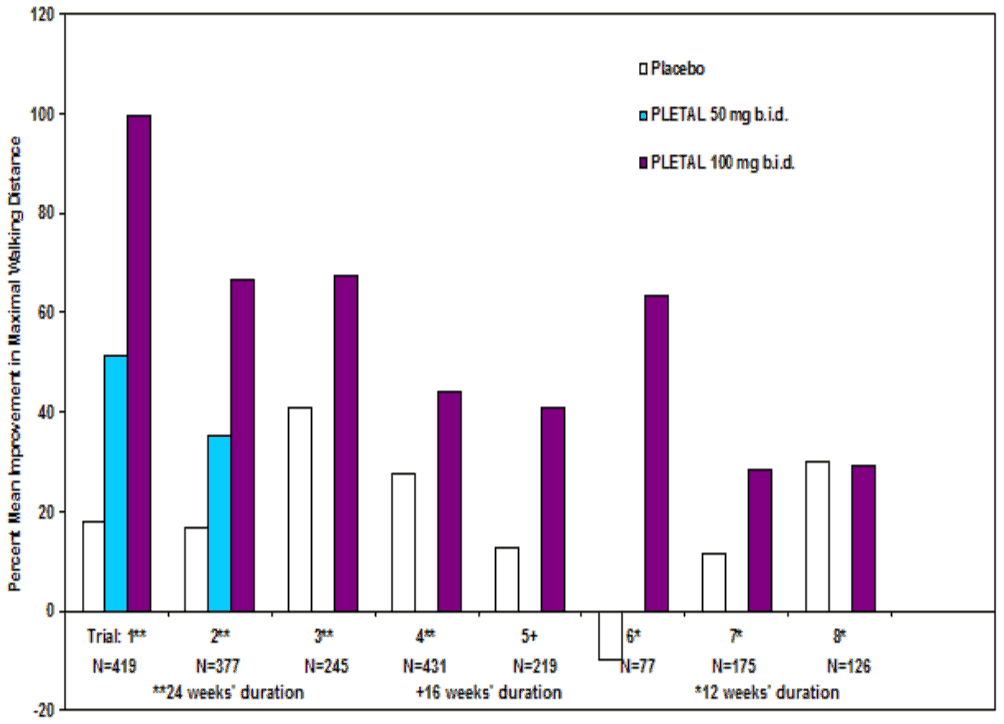
The ability of PLETAL to improve walking distance in patients with stable intermittent claudication was studied in eight, randomized, placebo-controlled, double-blind trials of 12 to 24 weeks' duration involving 2,274 patients using dosages of 50 mg twice daily (n=303), 100 mg twice daily (n=998), and placebo (n=973). Efficacy was determined primarily by the change in maximal walking distance from baseline (compared to change on placebo) on one of several standardized exercise treadmill tests.
Compared to patients treated with placebo, patients treated with PLETAL 50 or 100 mg twice daily experienced statistically significant improvements in walking distances both for the distance before the onset of claudication pain and the distance before exercise-limiting symptoms supervened (maximal walking distance). The effect of PLETAL on walking distance was seen as early as the first on-therapy observation point of two or four weeks.
Figure 2 depicts the percent mean improvement in maximal walking distance, at study end for each of the eight studies.
Figure 2. Percent Mean Improvement in Maximal Walking Distance at Study End for the Eight Randomized, Double-Blind, Placebo-Controlled Clinical Trials:
Across the eight clinical trials, the range of improvement in maximal walking distance in patients treated with PLETAL 100 mg twice daily, expressed as the change from baseline, was 28% to 100%.
The corresponding changes in the placebo group were –10% to 41%.
The Walking Impairment Questionnaire, which was administered in six of the eight clinical trials, assesses the impact of a therapeutic intervention on walking ability. In a pooled analysis of the six trials, patients treated with either PLETAL 100 mg twice daily or 50 mg twice daily reported improvements in their walking speed and walking distance as compared to placebo. Improvements in walking performance were seen in the various subpopulations evaluated, including those defined by gender, smoking status, diabetes mellitus, duration of peripheral artery disease, age, and concomitant use of beta blockers or calcium channel blockers. PLETAL has not been studied in patients with rapidly progressing claudication or in patients with leg pain at rest, ischemic leg ulcers, or gangrene. Its long-term effects on limb preservation and hospitalization have not been evaluated.
A randomized, double-blind, placebo-controlled Phase IV study was conducted to assess the long-term effects of cilostazol, with respect to mortality and safety, in 1,439 patients with intermittent claudication and no heart failure. The trial stopped early due to enrollment difficulties and a lower than expected overall death rate. With respect to mortality, the observed 36-month Kaplan-Meier event rate for deaths on study drug with a median time on study drug of 18 months was 5.6% (95% CI of 2.8 to 8.4%) on cilostazol and 6.8% (95% CI of 1.9 to 11.5%) on placebo. These data appear to be sufficient to exclude a 75% increase in the risk of mortality on cilostazol, which was the a priori study hypothesis.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.