RIGEVIDON Coated tablet Ref.[49643] Active ingredients: 17 alpha-Ethinylestradiol Levonorgestrel
Source: Web Search Revision Year: 2020 Publisher: Gedeon Richter Plc., Gyömrői út 19-21, 1103 Budapest, Hungary
4.3. Contraindications
Combined oral contraceptives (COCs) must not be used in the presence of the conditions mentioned below. If such a condition should occur for the first time during use of COCs, the use must be discontinued immediately:
- Presence or risk of venous thromboembolism (VTE)
- Venous thromboembolism – current VTE (on anticoagulants) or history of (e.g. deep venous thrombosis [DVT] or pulmonary embolism [PE])
- Known hereditary or acquired predisposition for venous thromboembolism, such as APCresistance, (including Factor V Leiden), antithrombin-III-deficiency, protein C deficiency, protein S deficiency
- Major surgery with prolonged immobilisation (see section 4.4)
- A high risk of venous thromboembolism due to the presence of multiple risk factors (see section 4.4)
- Presence or risk of arterial thromboembolism (ATE)
- Arterial thromboembolism – current arterial thromboembolism, history of arterial thromboembolism (e.g. myocardial infarction) or prodromal condition (e.g. angina pectoris)
- Cerebrovascular disease – current stroke, history of stroke or prodromal condition (e.g. transient ischaemic attack, TIA)
- Known hereditary or acquired predisposition for arterial thromboembolism, such as hyperhomocysteinaemia and anti-phospholipid antibodies (anticardiolipin-antibodies, lupus anticoagulant)
- History of migraine with focal neurological symptoms.
- A high risk of arterial thromboembolism due to multiple risk factors (see section 4.4) or to the presence of one serious risk factor such as:
- diabetes mellitus with vascular symptoms
- severe hypertension
- severe dyslipoproteinaemia.
- Severe hepatic disease, current or previous, as long as liver function values have not returned to normal.
- Presence or history of liver tumours (benign or malignant).
- Known or suspected hormone-dependent malignant tumour (e.g. genital organ or breast tumours).
- Undiagnosed vaginal bleeding.
- Hypersensitivity to the active substances levonorgestrel, ethinylestradiol or to any of the excipients listed in section 6.1.
Rigevidon is contraindicated for concomitant use with medicinal products containing ombitasvir/paritaprevir/ritonavir, dasabuvir, glecaprevir/pibrentasvir and sofosbuvir/velpatasvir/voxilaprevir (see sections 4.4 and 4.5).
4.4. Special warnings and precautions for use
Warnings
If any of the conditions or risk factors mentioned below is present, the suitability of Rigevidon should be discussed with the woman.
In the event of aggravation, or first appearance of any of these conditions or risk factors, the woman should be advised to contact her doctor to determine whether the use of Rigevidon should be discontinued.
Circulatory disorders
Risk of venous thromboembolism (VTE)
The use of any combined hormonal contraceptive (CHC) increases the risk of venous thromboembolism (VTE) compared with no use. Products that contain levonorgestrel, such as Rigevidon, norgestimate or norethisterone are associated with the lowest risk of VTE. The decision to use Rigevidon should be taken after a discussion with the woman to ensure she understands the risk of VTE with Rigevidon, how her current risk factors influence this risk, and that her VTE risk is highest in the first ever year of use. There is also some evidence that the risk is increased when a CHC is re-started after a break in use of 4 weeks or more.
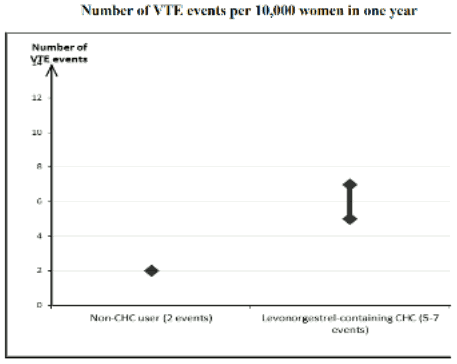
In women who do not use a CHC and are not pregnant, about 2 out of 10,000 will develop a VTE over the period of one year. However, in any individual woman the risk may be far higher, depending on her underlying risk factors (see below).
It is estimated that out of 10,000 women who use a CHC that contains levonorgestrel, about 61 will develop a VTE in one year.
This number of VTEs per year is fewer than the number expected in women during pregnancy or in the postpartum period.
VTE is fatal in 1% to 2% of the cases.
1 Mid-point of range of 5-7 per 10,000 WY, based on a relative risk for CHCs containing levonorgestrel versus non-use of approximately 2.3 to 3.6
Thrombosis in other blood vessels has very rarely been reported, i.e. hepatic, mesenteric, renal, cerebral or retinal veins and arteries, in users of oral contraceptives.
Risk factors for VTE
The risk for venous thromboembolic complications in COC users may increase substantially in a woman with additional risk factors, particularly if there are multiple risk factors (see table).
Rigevidon is contraindicated if a woman has multiple risk factors that put her at high risk of venous thrombosis (see section 4.3). If a woman has more than one risk factor, it is possible that the increase in risk is greater than the sum of the individual factors – in this case her total risk of VTE should be considered. If the balance of benefits and risks is considered to be negative a COC should not be prescribed (see section 4.3).
Table. Risk factors for VTE:
| Risk factor | Comment |
|---|---|
| Obesity (body mass index over 30 kg/m²) | Risk increases substantially as BMI rises. Particularly important to consider if other risk factors also present. |
| Prolonged immobilisation, major surgery, any surgery to the legs or pelvis, neurosurgery, or major trauma Note: temporary immobilisation including air travel >4 hours can also be a risk factor for VTE, particularly in women with other risk factors | In these situations it is advisable to discontinue use of the patch/pill/ring (in the case of elective surgery at least four weeks in advance) and not resume until two weeks after complete remobilisation. Another method of contraception should be used to avoid unintentional pregnancy. Antithrombotic treatment should be considered if Rigevidon has not been discontinued in advance. |
| Positive family history (venous thromboembolism ever in a sibling or parent especially at a relatively early age e.g. before 50). | If a hereditary predisposition is suspected, the woman should be referred to a specialist for advice before deciding about any CHC use. |
| Other medical conditions associated with VTE | Cancer, systemic lupus erythematosus, haemolytic uraemic syndrome, chronic inflammatory bowel disease (Crohn’s disease or ulcerative colitis) and sickle cell disease |
| Increasing age | Particularly above 35 years. |
There is no consensus about the possible role of varicose veins and superficial thrombophlebitis in the onset or progression of venous thrombosis.
The increased risk of thromboembolism in pregnancy, and particularly the 6 week period of the puerperium, must be considered (for information on “Fertility, pregnancy and lactation” see section 4.6).
Symptoms of VTE (deep vein thrombosis and pulmonary embolism)
In the event of symptoms women should be advised to seek urgent medical attention and to inform the healthcare professional that she is taking a CHC.
Symptoms of deep vein thrombosis (DVT) can include:
- unilateral swelling of the leg and/or foot or along a vein in the leg;
- pain or tenderness in the leg which may be felt only when standing or walking,
- increased warmth in the affected leg; red or discoloured skin on the leg.
Symptoms of pulmonary embolism (PE) can include:
- sudden onset of unexplained shortness of breath or rapid breathing;
- sudden coughing which may be associated with haemoptysis;
- sharp chest pain;
- severe light headedness or dizziness;
- rapid or irregular heartbeat.
Some of these symptoms (e.g. “shortness of breath”, “coughing”) are non-specific and might be misinterpreted as more common or less severe events (e.g. respiratory tract infections). Other signs of vascular occlusion can include: sudden pain, swelling and slight blue discoloration of an extremity.
If the occlusion occurs in the eye symptoms can range from painless blurring of vision which can progress to loss of vision. Sometimes loss of vision can occur almost immediately.
Risk of arterial thromboembolism (ATE)
Epidemiological studies have associated the use of CHCs with an increased risk for arterial thromboembolism (myocardial infarction) or for cerebrovascular accident (e.g. transient ischaemic attack, stroke). Arterial thromboembolic events may be fatal.
Risk factors for ATE
The risk of arterial thromboembolic complications or of a cerebrovascular accident in CHC users increases in women with risk factors (see table).
Rigevidon is contraindicated if a woman has one serious or multiple risk factors for ATE that puts her at high risk of arterial thrombosis (see section 4.3). If a woman has more than one risk factor, it is possible that the increase in risk is greater than the sum of the individual factors – in this case her total risk should be considered. If the balance of benefits and risks is considered to be negative a CHC should not be prescribed (see section 4.3).
Table. Risk factors for ATE:
| Risk factor | Comment |
|---|---|
| Increasing age | Particularly above 35 years. |
| Smoking | Women should be advised not to smoke if they wish to use a CHC. Women over 35 who continue to smoke should be strongly advised to use a different method of contraception. |
| Hypertension | |
| Obesity (body mass index over 30 kg/m²) | Risk increases substantially as BMI increases. Particularly important in women with additional risk factors. |
| Positive family history (arterial thromboembolism ever in a sibling or parent especially at relatively early age e.g. below 50). | If a hereditary predisposition is suspected, the woman should be referred to a specialist for advice before deciding about any CHC use. |
| Migraine | An increase in frequency or severity of migraine during CHC use (which may be prodromal of a cerebrovascular event) may be a reason for immediate discontinuation. |
| Other medical conditions associated with adverse vascular events | Diabetes mellitus, hyperhomocysteinaemia, valvular heart disease and atrial fibrillation, dyslipoproteinaemia and systemic lupus erythematosus. |
Symptoms of ATE
In the event of symptoms women should be advised to seek urgent medical attention and to inform the healthcare professional that she is taking a CHC.
Symptoms of a cerebrovascular accident can include:
- sudden numbness or weakness of the face, arm or leg, especially on one side of the body;
- sudden trouble walking, dizziness, loss of balance or coordination;
- sudden confusion, trouble speaking or understanding;
- sudden trouble seeing in one or both eyes;
- sudden, severe or prolonged headache with no known cause;
- loss of consciousness or fainting with or without seizure.
Temporary symptoms suggest the event is a transient ischaemic attack (TIA).
Symptoms of myocardial infarction (MI) can include:
- pain, discomfort, pressure, heaviness, sensation of squeezing or fullness in the chest, arm, or below the breastbone;
- discomfort radiating to the back, jaw, throat, arm, stomach;
- feeling of being full, having indigestion or choking;
- sweating, nausea, vomiting or dizziness;
- extreme weakness, anxiety, or shortness of breath;
- rapid or irregular heartbeats.
Tumours
An increased risk of cervical cancer in long-term users of COCs has been reported in some epidemiological studies, but there continues to be controversy about the extent to which this finding is attributable to the confounding effects of sexual behavior and other factors such as human papilloma virus (HPV).
A meta-analysis of 54 epidemiological studies showed that there is a slightly increased relative risk (RR = 1.24) of having breast cancer diagnosed in women who are currently using COCs. The excess risk gradually disappears during the course of the 10 years after cessation of COC use. Because breast cancer is rare in women under 40 years of age, the excess number of breast cancer diagnoses in current and recent COC users is small in relation to the overall risk of breast cancer. These studies do not provide evidence for causation.
The observed pattern of increased risk may be due to an earlier diagnosis of breast cancer in COC users, the biological effects of COCs or a combination of both. The breast cancers diagnosed in ever-users tend to be less advanced clinically than the cancers diagnosed in never-users.
In rare cases, benign liver tumors, and even more rarely, malignant liver tumors have been reported in users of COCs. In isolated cases, these tumors have led to life-threatening intra-abdominal hemorrhages. A hepatic tumor should be considered in the differential diagnosis when severe upper abdominal pain, liver enlargement or signs of intra-abdominal hemorrhage occur in women taking COCs.
Other conditions
Depression
Depressed mood and depression are well-known undesirable effects of hormonal contraceptive use (see section 4.8). Depression can be serious and is a well-known risk factor for suicidal behaviour and suicide. Women should be advised to contact their physician in case of mood changes and depressive symptoms, including shortly after initiating the treatment.
Hypertriglyceridaemia
Women with hypertriglyceridaemia, or a family history thereof, may be at increased risk of pancreatitis when taking COCs.
Liver conditions
Acute or chronic disturbances of liver function may necessitate the discontinuation of COC use until the liver function values returned to normal. Recurrence of cholestatic jaundice and/or cholestasisrelated pruritus which occurred during pregnancy or previous use of sex steroids necessitates the discontinuation of COCs.
Hypertension
Although small increases in blood pressure have been reported in many women taking COCs, clinically important increases are rare. Only in these rare cases an immediate discontinuation of COC use is justified. If, during the use of a COC in preexisting hypertension, constantly elevated blood pressure values or a significant increase in blood pressure do not respond adequately to antihypertensive treatment, the COC must be withdrawn. Where considered appropriate, COC use may be resumed if normotensive values can be achieved with antihypertensive therapy.
Angioedema
Exogenous estrogens may induce or exacerbate symptoms of hereditary and aquired angioedema.
Glucose intolerance / diabetes
Although COCs may have an effect on peripheral insulin resistance and glucose tolerance, there is no evidence for a need to alter the therapeutic regimen in diabetics using low-dose COCs (containing less than 0.05 mg of ethinylestradiol). Therefore, diabetics should be closely monitored during COC use.
Others
The relapse of a cholestatic jaundice or pruritus related to cholestasis that occurred during a previous pregnancy or prior intake of steroid hormones should lead to discontinuation of the COC.
The occurrence or exacerbation of the following pathologies has been observed during pregnancy or in women taking COCs, although the liability of the COC has not been set out: jaundice and/or pruritus because of a cholestasis, biliary lithiasis, porphyria, disseminated lupus erythematosus, haemolyticuraemic syndrome, Sydenham’s Chorea, gestational herpes, hearing loss because of otosclerosis.
Some cases of aggravation of endogenous depression, Crohn’s disease and ulcerative colitis have been observed when taking COCs.
Chloasma may occur, in particular in women with a medical history of chloasma gravidarum. Women with a predisposition to chloasma under COCs should avoid exposing themselves to sun or ultra-violet rays.
Women who get severely depressed during the use of COCs should discontinue use and be advised to use an alternative contraceptive method while trying to determine if the symptoms are due to the COC preparation. Women who have previously suffered from episodes of major depression should be closely monitored and stop the use of the COC if the symptoms of depression relapse.
Medical examination / consultation
Prior to the initiation or reinstitution of Rigevidon a complete medical history (including family history) should be taken and pregnancy must be ruled out. Blood pressure should be measured and a physical examination should be performed guided by the contraindications (see section 4.3) and warnings (see section 4.4). It is important to draw a woman’s attention to the information on venous and arterial thrombosis, including the risk of Rigevidon compared with other COCs, the symptoms of VTE and ATE, the known risk factors and what to do in the event of a suspected thrombosis. The woman should also be instructed to carefully read the user leaflet and to adhere to the advice given. The frequency and nature of examinations should be based on established practice guidelines and be adapted to the individual woman.
Women should be advised that oral contraceptives do not protect against HIV infections (AIDS) and other sexually transmitted diseases (STD).
Reduced efficacy
The efficacy of oral contraceptives may be reduced in the case of missed tablets (see section 4.2) vomiting or diarrhoea (see section 4.2) or concomitant medication (see section 4.5).
Reduced cycle control
With all combined oral contraceptives, irregular bleeding (spotting or break through bleeding) may occur, especially during the first months. Hence, the evaluation of any irregular bleeding should be considered after a period of adaptation of approximately 3 cycles.
If bleeding irregularities occur after previously regular cycles, then non-hormonal causes should be considered, and adequate diagnostic measures are indicated to exclude malignancy or pregnancy. These may include curettage.
Occasionally withdrawal bleeding during the tablet-free interval may not occur at all. If the tablets have been taken according to the instructions described in section 4.2, it is unlikely that the woman is pregnant. However, if the tablets have not been taken according to the instructions, before the first absent withdrawal bleeding, or if two withdrawal bleedings are overdue, pregnancy should be excluded before COC use is continued.
ALT elevations
During clinical trials with patients treated for hepatitis C virus infections (HCV) with the medicinal products containing ombitasvir/paritaprevir/ritonavir and dasabuvir with or without ribavirin, transaminase (ALT) elevations higher than 5 times the upper limit of normal (ULN) occurred significantly more frequent in women using ethinylestradiol-containing medications such as combined hormonal contraceptives (CHCs). ALT elevations have also been observed with HCV anti-viral medicinal products containing glecaprevir/pibrentasvir and sofosbuvir/velpatasvir/voxilaprevir (see sections 4.3 and 4.5).
Rigevidon contains lactose, sucrose and sodium
Patients with rare hereditary problems of galactose intolerance, total lactase deficiency or glucosegalactose malabsorption should not take this medicine.
Patients with rare hereditary problems of fructose intolerance, glucosegalactose malabsorption or sucrase-isomaltase insufficiency should not take this medicine.
This medicinal product contains less than 1 mmol sodium (23 mg) per tablet, that is to say essentially ‘sodium-free’.
4.5. Interaction with other medicinal products and other forms of interaction
Note: The prescribing information of concomitant medications should be consulted to identify potential interactions.
Pharmacodynamic interactions
Concomitant use with medicinal products containing ombitasvir/paritaprevir/ritonavir, dasabuvir, with or without ribavirin, glecaprevir/pibrentasvir and sofosbuvir/velpatasvir/voxilaprevir may increase the risk of ALT elevations (see sections 4.3 and 4.4). Therefore, Rigevidon users must switch to an alternative method of contraception (e.g., progestagen-only contraception or non-hormonal methods) prior to starting therapy with these drug regimens. Rigevidon can be restarted 2 weeks following completion of treatment with these drug regimens.
Pharmacokinetic interactions
Effects of other medicinal products on Rigevidon
Interactions can occur with drugs that induce microsomal enzymes which can result in increased clearance of sex hormones and which may lead to breakthrough bleeding and/or contraceptive failure.
Management
Enzyme induction can already be observed after a few days of treatment. Maximal enzyme induction is generally seen within a few weeks. After the cessation of drug therapy enzyme induction may be sustained for about 4 weeks.
Short-term treatment
Women on treatment with enzyme inducing drugs should temporarily use a barrier method or another method of contraception in addition to the COC. The barrier method must be used during the whole time of the concomitant drug therapy and for 28 days after its discontinuation.
If the drug therapy runs beyond the end of the tablets in the COC pack containing 21 tablets, the next COC pack should be started right after the previous one without the usual tablet-free interval.
Long-term treatment
In women on long-term treatment with enzyme-inducing active substances, another reliable, nonhormonal, method of contraception is recommended.
The following interactions have been reported in the literature
Substances increasing the clearance of COCs (diminished efficacy of COCs by enzyme-induction), e.g.
Barbiturates, bosentan, carbamazepine, phenytoin, primidone, rifampicin, and HIV medication ritonavir, nevirapine and efavirenz and possibly also felbamate, griseofulvin, oxcarbazepine, topiramate and products containing the herbal remedy St. John’s Wort (Hypericum perforatum).
Substances with variable effects on the clearance of COCs
When co-administered with COCs, many combinations of HIV protease inhibitors and non-nucleoside reverse transcriptase inhibitors, including combinations with HCV inhibitors can increase or decrease plasma concentrations of estrogen or progestins. The net effect of these changes may be clinically relevant in some cases.
Therefore, the prescribing information of concomitant HIV/HCV medications should be consulted to identify potential interactions and any related recommendations. In case of any doubt, an additional barrier contraceptive method should be used by women on protease inhibitor or non-nucleoside reverse transcriptase inhibitor therapy.
Substances decreasing the clearance of COCs (enzyme inhibitors)
The clinical relevance of potential interactions with enzyme inhibitors remains unknown. Concomitant administration of strong CYP3A4 inhibitors can increase plasma concentrations of the estrogen or the progestin or both.
Etoricoxib doses of 60 to 120 mg/day have been shown to increase plasma concentrations of ethinylestradiol 1.4 to 1.6-fold, respectively when taken concomitantly with a combined hormonal contraceptive containing 0.035 mg ethinylestradiol.
Effects of Rigevidon on other medicinal products
COCs may affect the metabolism of certain other active substances. Accordingly, plasma and tissue concentrations may either increase (e.g. ciclosporin) or decrease (e.g. lamotrigine).
Clinical data suggests that ethinylestradiol is inhibiting the clearance of CYP1A2 substrates leading to a weak (e.g. theophylline) or moderate (e.g. tizanidine) increase in their plasma concentration.
Laboratory tests
The use of contraceptive steroids may influence the results of certain laboratory tests, including biochemical parameters of liver, thyroid, adrenal and renal function; plasma levels of (carrier) proteins, e.g. corticosteroid-binding globulin and lipid/lipoprotein fractions; parameters of carbohydrate metabolism and parameters of blood coagulation and fibrinolysis. The changes generally remain within the normal laboratory range.
4.6. Fertility, pregnancy and lactation
Pregnancy
Rigevidon is not indicated during pregnancy.
If pregnancy occurs during medication with ehtinylestradiol/levonorgestrel, treatment should be withdrawn immediately.
Extensive epidemiological studies have revealed neither an increased risk of birth defects in children born to women who used COCs prior to pregnancy, nor a teratogenic effect at unintentional intake of contraceptive pills in early pregnancy.
The increased risk of VTE during the postpartum period should be considered when re-starting Rigevidon (see section 4.2 and 4.4).
Breast-feeding
Lactation may be influenced by contraceptive pills as they may reduce the amount of breast milk and change its composition. Thus, the use of combined oral contraceptives generally not be recommended until the nursing mother weaned her child off breast milk. Small amounts of contraceptive steroids and/or their metabolites may be excreted in the milk. These amounts may affect the child. If the woman wishes to breastfeed, another means of contraception should be proposed.
4.7. Effects on ability to drive and use machines
No study on the ability to drive and use machines has been performed. No effects on the ability to drive and use machines in COC users have been observed.
4.8. Undesirable effects
The following adverse effects have been reported during combined oral contraceptive treatment:
| System Organ Class 17.1 | Common (1/100 to <1/10) | Uncommon (1/1,000 to <1/100) | Rare (1/10,000 to <1/1,000) | Very rare (<1/10,000) | Not known (frequency cannot be estimated from the available data) |
|---|---|---|---|---|---|
| Neoplasms benign, malignant and unspecified (incl cysts and polyps) | Hepatocellular carcinoma, benign liver tumours (e.g. focal nodular hyperplasia, hepatic adenoma) | ||||
| Infections and infestations | Vaginitis including vaginal candidiasis | ||||
| Immune system disorders | Anaphylactic reactions with very rare cases of urticaria, angioedema, circulatory and severe respiratory disorders | Exacerbation of disseminated lupus erythematosus. | |||
| Metabolism and nutrition disorders | Altered appetite (increase or decrease) | Glucose intolerance | Exacerbation of a porphyria | ||
| Psychiatric disorders | Mood swings including depression, Altered libido | ||||
| Nervous system disorders | Nervousness, Dizziness | Exacerbated chorea | |||
| Eye disorders | Irritation by contact lenses | Optic neuritis, Retinal vascular thrombosis | |||
| Vascular disorders | Hypertension | Aggravated varicose veins | |||
| Gastrointestinal disorders | Nausea, Vomiting Abdominal pain | Abdominal cramps, bloating | Ischaemic colitis | Inflammatory bowel disease (Crohn’s disease, ulcerative colitis) | |
| Hepatobiliary disorders | Cholestatic jaundice | Pancreatitis, Cholelithiasis, Cholestasis | Hepatocellular condition (e.g. hepatitis, abnormal liver function) | ||
| Skin and subcutaneous tissue disorders | Acne | Rashes, Chloasma (melasma) with risk of persisting, hirsutism, hair loss | Erythema nodosum | Erythema multiforme | |
| Renal and urinary disorders | Haemolyticuraemic syndrome | ||||
| Reproductive system and breast disorders | Breast pain, stress, swelling and secretions, Dysmenorrhoea, Altered periods, Altered ectropion and vaginal secretions, Amennorrhoea | ||||
| General disorders and administration site conditions | Water retention/oedema, Altered weight (increase or decrease) | ||||
| Investigations | Modified plasma lipids, including hypertriglycerida emia, hypertension |
Description of selected adverse reactions
An increased risk of arterial and venous thrombotic and thromboembolic events, including myocardial infarction, stroke, transient ischemic attacks, venous thrombosis and pulmonary embolism has been observed in women using CHCs, which are discussed in more detail in section 4.4.
The following serious adverse events have been reported in women using COCs, which are discussed in section 4.4 Special warnings and precautions for use.
- Venous thromboembolic disorders, i.e. deep leg or pelvic venous thrombosis and pulmonary embolism.
- Arterial thromboembolic disorders
- Hypertension
- Cervical cancer
- Liver tumours
- Skin and subcutaeous disorders: chloasma; erythema nodosum.
- Crohn’s disease, ulcerative colitis, porphyria, systemic lupus erythematosus, herpes gestationis, Sydenham’s chorea, haemolytic uremic syndrome, cholestatic jaundice.
The frequency of diagnosis of breast cancer is very slightly increased among COC-users. As breast cancer is rare in women under 40 years of age the excess number is small in relation to the overall risk of breast cancer. Causation with COC use is unknown. For further information, see sections 4.3 and 4.4.
Exogenous estrogens may induce or exacerbate symptoms of hereditary and aquired angioedema.
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the Yellow Card Scheme (website: www.mhra.gov.uk/yellowcard) or search for MHRA Yellow Card in the Google Play or Apple App Store.
6.2. Incompatibilities
Not applicable.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.