SOLU-MEDRONE Powder for injection Ref.[7317] Active ingredients: Methylprednisolone
Source: Medicines & Healthcare Products Regulatory Agency (GB) Revision Year: 2018 Publisher: Pfizer Limited, Ramsgate Road, Sandwich, Kent, CT13 9NJ, United Kingdom
Contraindications
Solu-Medrone is contraindicated:
- In patients who have systemic fungal infections unless specific anti-infective therapy is employed and in cerebral oedema in malaria.
- In patients with known hypersensitivity to methylprednisolone or to any of the excipients listed in section 6.1.
- For use by the intrathecal route of administration.
Administration of live or live, attenuated vaccines is contraindicated in patients receiving immunosuppressive doses of corticosteroids.
Special warnings and precautions for use
Immunosuppressant Effects/Increased Susceptibility to Infections
Corticosteroids may increase susceptibility to infection, may mask some signs of infection, and new infections may appear during their use. Suppression of the inflammatory response and immune function increases the susceptibility to fungal, viral and bacterial infections and their severity. The clinical presentation may often be atypical and may reach an advanced stage before being recognised.
Persons who are on drugs which suppress the immune system are more susceptible to infections than healthy individuals. Chicken pox and measles, for example, can have a more serious or even fatal course in non-immune children or adults on corticosteroids.
Chickenpox is of serious concern since this normally minor illness may be fatal in immunosuppressed patients. Patients (or parents of children) without a definite history of chickenpox should be advised to avoid close personal contact with chickenpox or herpes zoster and if exposed they should seek urgent medical attention. Passive immunization with varicella/zoster immunoglobin (VZIG) is needed by exposed non-immune patients who are receiving systemic corticosteroids or who have used them within the previous 3 months; this should be given within 10 days of exposure to chickenpox. If a diagnosis of chickenpox is confirmed, the illness warrants specialist care and urgent treatment. Corticosteroids should not be stopped and the dose may need to be increased.
Exposure to measles should be avoided. Medical advice should be sought immediately if exposure occurs. Prophylaxis with normal intramuscular immunoglobulin may be needed.
Similarly, corticosteroids should be used with great care in patients with known or suspected parasitic infections such as Strongyloides (threadworm) infestation, which may lead to Strongyloides hyperinfection and dissemination with widespread larval migration, often accompanied by severe enterocolitis and potentially fatal gram-negative septicaemia.
Live vaccines should not be given to individuals with impaired immune responsiveness. The antibody response to other vaccines may be diminished.
The use of corticosteroids in active tuberculosis should be restricted to those cases of fulminating or disseminated tuberculosis in which the corticosteroid is used for the management of the disease in conjunction with an appropriate anti-tuberculous regimen.
If corticosteroids are indicated in patients with latent tuberculosis or tuberculin reactivity, close observation is necessary as reactivation of the disease may occur. During prolonged corticosteroid therapy, these patients should receive chemoprophylaxis.
Kaposi’s sarcoma has been reported to occur in patients receiving corticosteroid therapy. Discontinuation of corticosteroids may result in clinical remission.
Although Solu-Medrone is not approved in the UK for use in any shock indication, the following warning statement should be adhered to. Data from a clinical study conducted to establish the efficacy of Solu-Medrone in septic shock, suggest that a higher mortality occurred in subsets of patients who entered the study with elevated serum creatinine levels or who developed a secondary infection after therapy began. Therefore this product should not be used in the treatment of septic syndrome or septic shock.
The role of corticosteroids in septic shock has been controversial, with early studies reporting both beneficial and detrimental effects. More recently, supplemental corticosteroids have been suggested to be beneficial in patients with established septic shock who exhibit adrenal insufficiency. However, their routine use in septic shock is not recommended. A systematic review of short-course, high-dose corticosteroids did not support their use. However, meta- analyses, and a review suggest that longer courses (5-11 days) of low-dose corticosteroids might reduce mortality, especially in patients with vasopressor-dependent septic shock.
Immune System Effects
Allergic reactions may occur. Rarely skin reactions and anaphylactic/anaphylactoid reactions have been reported following parenteral Solu-Medrone therapy. Physicians using the drug should be prepared to deal with such a possibility. Appropriate precautionary measures should be taken prior to administration, especially when the patient has a history of drug allergy.
Endocrine Effects
In patients on corticosteroid therapy subjected to unusual stress, increased dosage of rapidly acting corticosteroids before, during and after the stressful situation is indicated.
Pharmacologic doses of corticosteroids administered for prolonged periods may result in hypothalamic-pituitary-adrenal (HPA) suppression (secondary adrenocortical insufficiency). The degree and duration of adrenocortical insufficiency produced is variable among patients and depends on the dose, frequency, time of administration, and duration of glucocorticoid therapy. This effect may be minimized by use of alternate-day therapy.
In addition, acute adrenal insufficiency leading to a fatal outcome may occur if glucocorticoids are withdrawn abruptly.
In patients who have received more than physiological doses of systemic corticosteroids (approximately 6 mg methylprednisolone) for greater than 3 weeks, withdrawal should not be abrupt.
Drug-induced secondary adrenocortical insufficiency may therefore be minimized by gradual reduction of dosage. How dose reduction should be carried out depends largely on whether the disease is likely to relapse as the dose of systemic corticosteroids is reduced. Clinical assessment of disease activity may be needed during withdrawal. If the disease is unlikely to relapse on withdrawal of systemic corticosteroids, but there is uncertainty about HPA suppression, the dose of systemic corticosteroid may be reduced rapidly to physiological doses. Once a daily dose of 6 mg methylprednisolone is reached, dose reduction should be slower to allow the HPA-axis to recover.
Abrupt withdrawal of systemic corticosteroid treatment, which has continued up to 3 weeks is appropriate if it considered that the disease is unlikely to relapse. Abrupt withdrawal of doses up to 32 mg daily of methylprednisolone for 3 weeks is unlikely to lead to clinically relevant HPA-axis suppression, in the majority of patients. In the following patient groups, gradual withdrawal of systemic corticosteroid therapy should be considered even after courses lasting 3 weeks or less:
- Patients who have had repeated courses of systemic corticosteroids, particularly if taken for greater than 3 weeks.
- When a short course has been prescribed within one year of cessation of long-term therapy (months or years).
- Patients who may have reasons for adrenocortical insufficiency other than exogenous corticosteroid therapy.
- Patients receiving doses of systemic corticosteroid greater than 32 mg daily of methylprednisolone.
- Patients repeatedly taking doses in the evening.
Patients should carry ‘Steroid Treatment’ cards which give clear guidance on the precautions to be taken to minimise risk and which provide details of prescriber, drug, dosage and the duration of treatment.
This type of relative insufficiency may persist for months after discontinuation of therapy; therefore, in any situation of stress occurring during that period, hormone therapy should be reinstituted.
A steroid “withdrawal syndrome”, seemingly unrelated to adrenocortical insufficiency, may also occur following abrupt discontinuance of glucocorticoids. This syndrome includes symptoms such as: anorexia, nausea, vomiting, lethargy, headache, fever, joint pain, desquamation, myalgia, weight loss, and/or hypotension. These effects are thought to be due to the sudden change in glucocorticoid concentration rather than to low corticosteroid levels.
Because glucocorticoids can produce or aggravate Cushing’s syndrome, glucocorticoids should be avoided in patients with Cushing’s disease.
There is an enhanced effect of corticosteroids on patients with hypothyroidism. Frequent patient monitoring is necessary in patients with hypothyroidism.
Metabolism and Nutrition
Frequent patient monitoring is necessary in patients with diabetes mellitus (or a family history of diabetes). Corticosteroids, including methylprednisolone, can increase blood glucose, worsen pre-existing diabetes, and predispose those on long-term corticosteroid therapy to diabetes mellitus.
Psychiatric Effects
Patients and/or carers should be warned that potentially severe psychiatric adverse reactions may occur with systemic steroids (see section 4.8). Symptoms typically emerge within a few days or weeks of starting treatment. Risks may be higher with high doses/systemic exposure (see also section 4.5), although dose levels do not allow prediction of the onset, type, severity or duration of reactions. Most reactions recover after either dose reduction or withdrawal, although specific treatment may be necessary. Patients/carers should be encouraged to seek medical advice if worrying psychological symptoms develop, especially if depressed mood or suicidal ideation is suspected. Patients/carers should be alert to possible psychiatric disturbances that may occur either during or immediately after dose tapering/withdrawal of systemic steroids, although such reactions have been reported infrequently.
Particular care is required when considering the use of systemic corticosteroids in patients with existing or previous history of severe affective disorders in themselves or in their first degree relatives. These would include depressive or manic-depressive illness and previous steroid psychosis.
Frequent patient monitoring is necessary in patients with existing or previous history of severe affective disorders (especially previous steroid psychosis).
Nervous System Effects
Corticosteroids should be used with caution in patients with seizure disorders. Frequent patient monitoring is necessary in patients with epilepsy.
Corticosteroids should be used with caution in patients with myasthenia gravis. (Also see myopathy statement in Musculoskeletal Effects section). Frequent patient monitoring is necessary in patients with myasthenia gravis.
Severe medical events have been reported in association with the intrathecal/epidural routes of administration (see section 4.8).
There have been reports of epidural lipomatosis in patients taking corticosteroids, typically with long-term use at high doses.
Ocular Effects
Visual disturbance may be reported with systemic and topical corticosteroid use. If a patient presents with symptoms such as blurred vision or other visual disturbances, the patient should be considered for referral to an ophthalmologist for evaluation of possible causes which may include cataract, glaucoma or rare diseases such as central serous chorioretinopathy (CSCR) which have been reported after use of systemic and topical corticosteroids. Central serous chorioretinopathy, may lead to retinal detachment.
Frequent patient monitoring is necessary in patients with glaucoma (or a family history of glaucoma) and in patients with ocular herpes simplex, for fear of corneal perforation.
Prolonged use of corticosteroids may produce posterior subcapsular cataracts and nuclear cataracts (particularly in children), exophthalmos, or increased intraocular pressure, which may result in glaucoma with possible damage to the optic nerves. Establishment of secondary fungal and viral infections of the eye may also be enhanced in patients receiving glucocorticoids.
Cardiac Effects
Adverse effects of glucocorticoids on the cardiovascular system, such as dyslipidaemia and hypertension, may predispose treated patients with existing cardiovascular risk factors to additional cardiovascular effects, if high doses and prolonged courses are used. Accordingly, corticosteroids should be employed judiciously in such patients and attention should be paid to risk modification and additional cardiac monitoring if needed. Low dose and alternate day therapy may reduce the incidence of complications in corticosteroid therapy.
There have been a few reports of cardiac arrhythmias and/or circulatory collapse and/or cardiac arrest associated with the rapid intravenous administration of large doses of Solu-Medrone (greater than 500 mg administered over a period of less than 10 minutes). Bradycardia has been reported during or after the administration of large doses of methylprednisolone sodium succinate, and may be unrelated to the speed and duration of infusion.
Systemic corticosteroids should be used with caution, and only if strictly necessary, in cases of congestive heart failure.
Care should be taken for patients receiving cardioactive drugs such as digoxin because of steroid induced electrolyte disturbance/potassium loss (see section 4.8).
Frequent patient monitoring is necessary in patients with congestive heart failure or recent myocardial infarction (myocardial rupture has been reported).
Vascular Effects
Steroids should be used with caution in patients with hypertension. Frequent patient monitoring is necessary.
Thrombosis including venous thromboembolism has been reported to occur with corticosteroids. As a result, corticosteroids should be used with caution in patients who have or may be predisposed to thromboembolic disorders.
Gastrointestinal Effects
High doses of corticosteroids may produce acute pancreatitis.
There is no universal agreement on whether corticosteroids per se are responsible for peptic ulcers encountered during therapy; however, glucocorticoid therapy may mask the symptoms of peptic ulcer so that perforation or haemorrhage may occur without significant pain. Glucocorticoid therapy may mask peritonitis or other signs or symptoms associated with gastrointestinal disorders such as perforation, obstruction or pancreatitis.
In combination with NSAIDs, the risk of developing gastrointestinal ulcers is increased.
Particular care is required when considering the use of systemic corticosteroids in patients with the following conditions and frequent patient monitoring is necessary.
Ulcerative colitis
Perforation, Abscess or other pyogenic infections
Diverticulitis
Fresh intestinal anastomoses
Peptic ulceration
Hepatobiliary Effects
Drug induced liver injury including acute hepatitis or liver enzyme increase can result from cyclical pulsed IV methylprednisolone (usually at initial dose ≥1 g/day). Rare cases of hepatotoxicity have been reported. The time to onset can be several weeks or longer. In the majority of case reports resolution of the adverse events has been observed after treatment was discontinued. Therefore, appropriate monitoring is required.
Musculoskeletal Effects
Particular care is required when considering the use of systemic corticosteroids in patients with myasthenia gravis or osteoporosis (post-menopausal females are particularly at risk) and frequent patient monitoring is necessary.
Osteoporosis is a common but infrequently recognized adverse effect associated with a long-term use of large doses of glucocorticoid.
Renal and urinary disorders
Caution is required in patients with systemic sclerosis because an increased incidence of scleroderma renal crisis has been observed with corticosteroids, including methylprednisolone. Blood pressure and renal function (s-creatinine) should therefore be routinely checked. When renal crisis is suspected, blood pressure should be carefully controlled.
Particular care is required when considering the use of systemic corticosteroids in patients with renal insufficiency and frequent patient monitoring is necessary.
Investigations
Average and large doses of hydrocortisone or cortisone can cause elevation of blood pressure, salt and water retention, and increased excretion of potassium. These effects are less likely to occur with the synthetic derivatives except when used in large doses. Dietary salt restriction and potassium supplementation may be necessary. All corticosteroids increase calcium excretion.
Injury, poisoning and procedural complications
Systemic corticosteroids are not indicated for, and therefore should not be used to treat, traumatic brain injury, a multicentre study revealed an increased mortality at 2 weeks and 6 months after injury in patients administered methylprednisolone sodium succinate compared to placebo. A causal association with methylprednisolone sodium succinate treatment has not been established.
Other
Since complications of treatment with glucocorticoids are dependent on the size of the dose and the duration of treatment, a risk/benefit decision must be made in each individual case as to dose and duration of treatment as to whether daily or intermittent therapy should be used.
Co-treatment with CYP3A inhibitors, including cobicistat-containing products, is expected to increase the risk of systemic side-effects. The combination should be avoided unless the benefit outweighs the increased risk of systemic corticosteroid side-effects, in which case patients should be monitored for systemic corticosteroid side-effects (see section 4.5).
The lowest possible dose of corticosteroid should be used to control the condition under treatment and when reduction in dosage is possible, the reduction should be gradual.
Aspirin and non-steroidal anti-inflammatory agents should be used cautiously in conjunction with corticosteroids.
Pheochromocytoma crisis, which can be fatal, has been reported after administration of systemic corticosteroids. Corticosteroids should only be administered to patients with suspected or identified pheochromocytoma after an appropriate risk/benefit evaluation.
Paediatric population
Growth and development of infants and children on prolonged corticosteroid therapy should be carefully observed. Growth may be suppressed in children receiving long-term, daily, divided-dose glucocorticoid therapy and use of such regimen should be restricted to the most urgent indications. Alternate-day glucocorticoid therapy usually avoids or minimizes this side effect.
Infants and children on prolonged corticosteroid therapy are at special risk from raised intracranial pressure.
High doses of corticosteroids may produce pancreatitis in children.
Interaction with other medicinal products and other forms of interaction
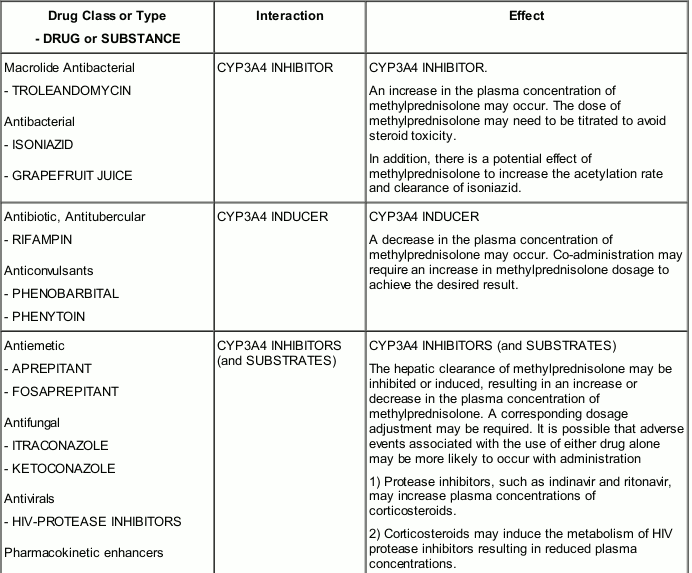
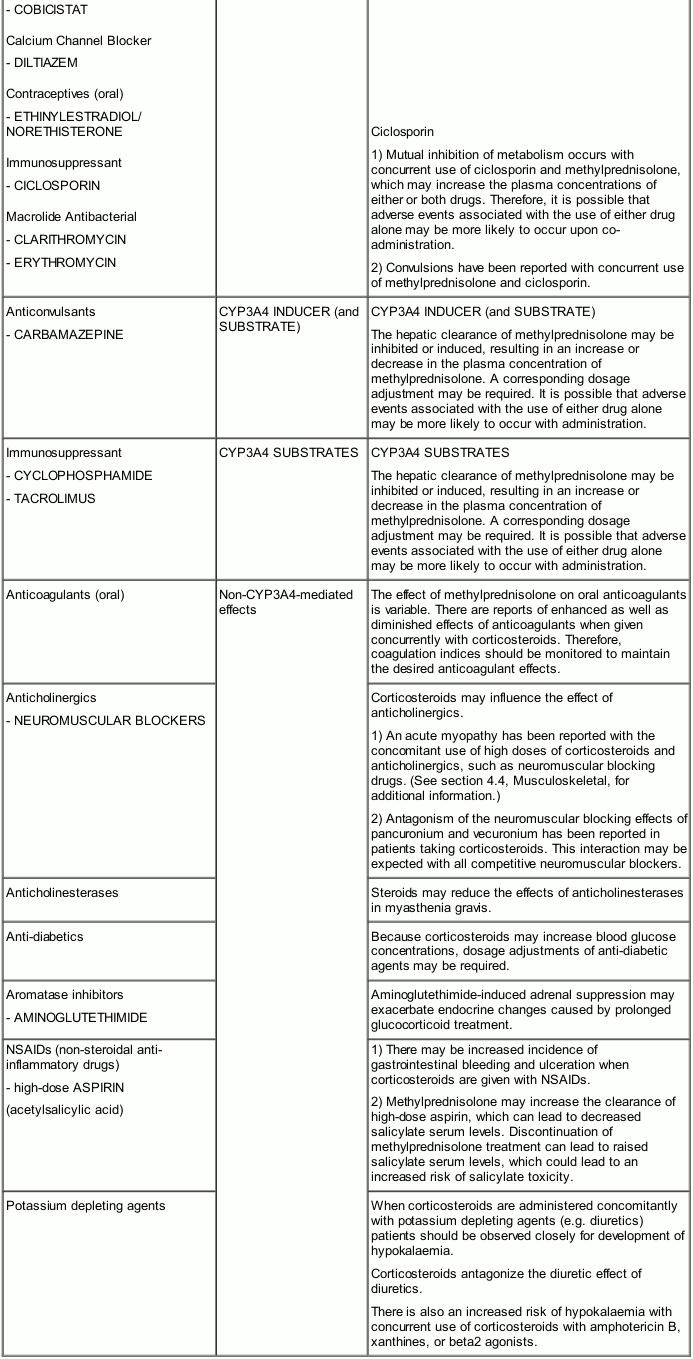
Methylprednisolone is a cytochrome P450 enzyme (CYP) substrate and is mainly metabolized by the CYP3A4 enzyme. CYP3A4 is the dominant enzyme of the most abundant CYP subfamily in the liver of adult humans. It catalyzes 6β-hydroxylation of steroids, the essential Phase I metabolic step for both endogenous and synthetic corticosteroids. Many other compounds are also substrates of CYP3A4, some of which (as well as other drugs) have been shown to alter glucocorticoid metabolism by induction (up-regulation) or inhibition of the CYP3A4 enzyme.
CYP3A4 inhibitors: Drugs that inhibit CYP3A4 activity generally decrease hepatic clearance and increase the plasma concentration of CYP3A4 substrate medications, such as methylprednisolone. In the presence of a CYP3A4 inhibitor, the dose of methylprednisolone may need to be titrated to avoid steroid toxicity.
CYP3A4 inducers: Drugs that induce CYP3A4 activity generally increase hepatic clearance, resulting in decreased plasma concentration of medications that are substrates for CYP3A4. Co-administration may require an increase in methylprednisolone dosage to achieve the desired result.
CYP3A4 substrates: In the presence of another CYP3A4 substrate, the hepatic clearance of methylprednisolone may be affected, with corresponding dosage adjustments required. It is possible that adverse events associated with the use of either drug alone may be more likely to occur with co-administration.
Non-CYP3A4-mediated effects: Other interactions and effects that occur with methylprednisolone are described in Table 1 below.
Table 1 provides a list and descriptions of the most common and/or clinically important drug interactions or effects with methylprednisolone.
Table 1. Important drug or substance interactions/effects with methylprednisolone:
Corticosteroids antagonize the hypotensive effect of all antihypertensives.
There is an increased risk of hypokalaemia when corticosteroids are given with cardiac glycosides.
The effects of corticosteroids may be reduced for 3-4 days after mifepristone.
Incompatibilities
To avoid compatibility and stability problems, it is recommended that methylprednisolone sodium succinate be administered separately from other compounds that are administered via the IV route of administration. Drugs that are physically incompatible in solution with methylprednisolone sodium succinate include allopurinol sodium, doxapram hydrochloride, tigecycline, diltiazem hydrochloride, calcium gluconate, vecuronium bromide, rocuronium bromide, cisatracurium besylate, glycopyrrolate and propofol. (See section 6.2 for additional information.)
Fertility, pregnancy and lactation
Fertility
Corticosteroids have been shown to impair fertility in animal studies (see section 5.3). In women treatment with corticosteroids can lead to menstrual irregularities.
Pregnancy
The ability of corticosteroids to cross the placenta varies between individual drugs, however, methylprednisolone does cross the placenta.
Administration of corticosteroids to pregnant animals can cause abnormalities of foetal development including cleft palate, intra-uterine growth retardation and affects on brain growth and development. There is no evidence that corticosteroids result in an increased incidence of congenital abnormalities, such as cleft palate in man, however, when administered for long periods or repeatedly during pregnancy, corticosteroids may increase the risk of intra-uterine growth retardation. Hypoadrenalism may, in theory, occur in the neonate following pre-natal exposure to corticosteroids but usually resolves spontaneously following birth and is rarely clinically important. Infants born to mothers, who have received substantial doses of corticosteroids during pregnancy must be carefully observed and evaluated for signs of adrenal insufficiency. As with all drugs, corticosteroids should only be prescribed when the benefits to the mother and child outweigh the risks. When corticosteroids are essential, however, patients with normal pregnancies may be treated as though they were in the non-gravid state.
Since adequate human reproductive studies have not been done with methylprednisolone sodium succinate, this medicinal product should be used during pregnancy only after a careful assessment of the benefit risk ratio to the mother and foetus.
In humans, the risk of low birth weight appears to be dose related and may be minimized by administering lower corticosteroid doses.
Cataracts have been observed in infants born to mothers undergoing long-term treatment with corticosteroids during pregnancy.
Breast-feeding
Corticosteroids are excreted in small amounts in breast milk, however, doses of up to 40 mg daily of methylprednisolone are unlikely to cause systemic effects in the infant. This medicinal product should be used during breast feeding only after a careful assessment of the benefit risk ratio to the mother and infant.
Effects on ability to drive and use machines
The effect of corticosteroids on the ability to drive or use machinery has not been systematically evaluated. Undesirable effects, such as dizziness, vertigo, visual disturbances, and fatigue are possible after treatment with corticosteroids. If affected, patients should not drive or operate machinery.
Undesirable effects
The following adverse reactions have been reported with the following routes of administration: Intrathecal/Epidural: Arachnoiditis, functional gastrointestinal disorder/bladder dysfunction, headache, meningitis, paraparesis/paraplegia, seizure and sensory disturbances.
Under normal circumstances Solu-Medrone therapy would be considered as short-term. However, the possibility of side-effects attributable to corticosteroid therapy should be recognised, particularly when high-dose therapy is being used (see section 4.4). Such side-effects include:
Frequency: Common (≥1/100 to <1/10); Uncommon (≥1/1,000 to <1/100); Rare (≥1/10,000 to <1/1,000); Not known (frequency cannot be estimated from the available data)
Infections and infestations
Not Known: Infection (including increased susceptibility and severity of infections with suppression of clinical symptoms and signs); Opportunistic infection; Recurrence of dormant tuberculosis (see section 4.4); Peritonitis#
Neoplasms benign, malignant and unspecified (including cysts and polyps
Not Known: Kaposi’s sarcoma has been reported to occur in patients receiving corticosteroid therapy. Discontinuation of corticosteroids may result in clinical remission.
Blood and lymphatic system disorders
Not Known: Leukocytosis.
Immune system disorders
Not Known: Drug hypersensitivity (Anaphylactic reaction; Anaphylactoid reaction).
Endocrine disorders
Not Known: Cushingoid; Hypopituitarism (including suppression of the hypothalamo-pituitary-adrenal axis); Steroid withdrawal syndrome (including, fever, myalgia, arthralgia, rhinitis, conjunctivitis, painful itchy skin nodules and loss of weight).
Metabolism and nutrition disorders
Not Known: Metabolic acidosis; Sodium retention; Fluid retention; Glucose tolerance impaired; Alkalosis hypokalaemic; Dyslipidemia; Increased insulin requirements (or oral hypoglycemic agents in diabetics); Lipomatosis; Increased appetite (which may result in weight increase); Epidural lipomatosis.
Psychiatric disorders
Not Known: A wide range of psychiatric reactions including affective disorders (such as irritable, euphoric, depressed and labile mood, drug dependence and suicidal thoughts), psychotic reactions (including mania, delusions, hallucinations and schizophrenia), behavioural disturbances, irritability, anxiety, sleep disturbances, and cognitive dysfunction including confusion and amnesia have been reported for all corticosteroids. Reactions may occur in both adults and children. In adults, the frequency of severe reactions was estimated to be 5%-6%. Psychological effects have been reported on withdrawal of corticosteroids; the frequency is unknown.
Nervous system disorders
Not Known: Increased intracranial pressure with Papilloedema [Benign intracranial hypertension]; Seizure; Amnesia; Cognitive disorder; Dizziness; Headache.
Eye disorders
Rare: Vision blurred (see also section 4.4).
Not Known: Posterior subcapsular cataracts; Exophthalmos; Glaucoma; Papilloedema with possible damage to the optic nerve; Corneal or scleral thinning; Exacerbation of ophthalmic viral or fungal disease; Chorioretinopathy.
Ear and labyrinth disorders
Not Known: Vertigo.
Cardiac disorders
Not Known: Congestive heart failure in susceptible patients; Arrhythmia.
Vascular disorders
Not Known: Hypertension; Hypotension; Thrombotic events.
Respiratory, thoracic and mediastinal disorders
Not Known: Hiccups; Pulmonary embolism.
Gastrointestinal disorders
Not Known: Peptic ulcer (with possible peptic ulcer perforation and peptic ulcer haemorrhage); Gastric haemorrhage; Intestinal perforation; Pancreatitis; Ulcerative oesophagitis; Oesophagitis; Oesophageal candidiasis; Abdominal pain; Abdominal distension; Diarrhoea; Dyspepsia; Nausea; Vomiting; Bad taste in mouth may occur especially with rapid administration.
Hepatobiliary disorders
Not Known: Hepatitis†; Increase of liver enzymes (e.g. alanine aminotransferase increased (ALT, SGPT), aspartate aminotransferase increased (AST, SGOT)).
Skin and subcutaneous tissue disorders
Not Known: Ecchymosis; Skin atrophy (thin fragile skin); Acne; Angioedema; Petechiae; Skin striae; Telangiectasia; Skin hypopigmentation or hyperpigmentation; Hirsutism; Rash; Erythema; Pruritus; Urticaria; Hyperhidrosis.
Musculoskeletal and connective tissue disorders
Not Known: Growth retardation; Osteoporosis; Muscular weakness; Osteonecrosis; Pathological fracture; Muscle atrophy; Myopathy; Neuropathic arthropathy; Arthralgia; Myalgia.
Reproductive system and breast disorders
Not Known: Irregular menstruation; Amenorrhoea.
General disorders and administration site conditions
Not Known: Impaired wound healing; Oedema peripheral; Injection site reaction; Fatigue; Malaise; Withdrawal symptoms – Too rapid a reduction of corticosteroid dosage following prolonged treatment can lead to acute adrenal insufficiency, hypotension and death. However, this is more applicable to corticosteroids with an indication where continuous therapy is given (see section 4.4).
Investigations
Not Known: Intraocular pressure increased; Carbohydrate tolerance decreased; Blood potassium decreased (potassium loss); Urine calcium increased; Blood alkaline phosphatase increased; Blood urea increased; Suppression of reactions to skin tests.
Injury, poisoning and procedural complications
Not Known: Tendon rupture (particularly of the Achilles tendon); Spinal compression fracture (vertebral compression fractures).
† Hepatitis has been reported with IV administration (see section 4.4).
# Peritonitis may be the primary presenting sign or symptom of a gastrointestinal disorder such as perforation, obstruction or pancreatitis (see section 4.4).
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the Yellow Card Scheme at www.mhra.gov.uk/yellowcard.
Incompatibilities
Not applicable.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.