SPRYCEL Film-coated tablet Ref.[8962] Active ingredients: Dasatinib
Source: European Medicines Agency (EU) Revision Year: 2020 Publisher: Bristol-Myers Squibb Pharma EEIG, Plaza 254, Blanchardstown Corporate Park 2, Dublin 15, D15 T867, Ireland
Pharmacodynamic properties
Pharmacotherapeutic group: antineoplastic agents, protein kinase inhibitors
ATC code: L01XE06
Pharmacodynamics
Dasatinib inhibits the activity of the BCR-ABL kinase and SRC family kinases along with a number of other selected oncogenic kinases including c-KIT, ephrin (EPH) receptor kinases, and PDGFβ receptor. Dasatinib is a potent, subnanomolar inhibitor of the BCR-ABL kinase with potency at concentration of 0.6-0.8 nM. It binds to both the inactive and active conformations of the BCR-ABL enzyme.
Mechanism of action
In vitro, dasatinib is active in leukaemic cell lines representing variants of imatinib-sensitive and resistant disease. These non-clinical studies show that dasatinib can overcome imatinib resistance resulting from BCR-ABL overexpression, BCR-ABL kinase domain mutations, activation of alternate signalling pathways involving the SRC family kinases (LYN, HCK), and multidrug resistance gene overexpression. Additionally, dasatinib inhibits SRC family kinases at subnanomolar concentrations.
In vivo, in separate experiments using murine models of CML, dasatinib prevented the progression of chronic CML to blast phase and prolonged the survival of mice bearing patient-derived CML cell lines grown at various sites, including the central nervous system.
Clinical efficacy and safety
In the Phase I study, haematologic and cytogenetic responses were observed in all phases of CML and in Ph+ ALL in the first 84 patients treated and followed for up to 27 months. Responses were durable across all phases of CML and Ph+ ALL.
Four single-arm, uncontrolled, open-label Phase II clinical studies were conducted to determine the safety and efficacy of dasatinib in patients with CML in chronic, accelerated, or myeloid blast phase, who were either resistant or intolerant to imatinib. One randomised non-comparative study was conducted in chronic phase patients who failed initial treatment with 400 or 600 mg imatinib. The starting dose was 70 mg dasatinib twice daily. Dose modifications were allowed for improving activity or management of toxicity (see section 4.2).
Two randomised, open-label Phase III studies were conducted to evaluate the efficacy of dasatinib administered once daily compared with dasatinib administered twice daily. In addition, one open-label, randomised, comparative Phase III study was conducted in adult patients with newly diagnosed chronic phase CML.
The efficacy of dasatinib is based on haematological and cytogenetic response rates. Durability of response and estimated survival rates provide additional evidence of dasatinib clinical benefit.
A total of 2,712 patients were evaluated in clinical studies; of these 23% were ≥ 65 years of age and 5% were ≥75 years of age.
Chronic phase CML – Newly diagnosed
An international open-label, multicentre, randomised, comparative Phase III study was conducted in adult patients with newly diagnosed chronic phase CML. Patients were randomised to receive either SPRYCEL 100 mg once daily or imatinib 400 mg once daily. The primary endpoint was the rate of confirmed complete cytogenetic response (cCCyR) within 12 months. Secondary endpoints included time in cCCyR (measure of durability of response), time to cCCyR, major molecular response (MMR) rate, time to MMR, progression free survival (PFS) and overall survival (OS). Other relevant efficacy results included CCyR and complete molecular response (CMR) rates. The study is ongoing.
A total of 519 patients were randomised to a treatment group: 259 to SPRYCEL and 260 to imatinib. Baseline characteristics were well balanced between the two treatment groups with respect to age (median age was 46 years for the SPRYCEL group and 49 years for the imatinib group with 10% and 11% of patients 65 years of age or older, respectively), gender (women 44% and 37%, respectively), and race (Caucasian 51% and 55%; Asian 42% and 37%, respectively). At baseline, the distribution of Hasford Scores was similar in the SPRYCEL and imatinib treatment groups (low risk: 33% and 34%; intermediate risk 48% and 47%; high risk: 19% and 19%, respectively).
With a minimum of 12 months follow-up, 85% of patients randomised to the SPRYCEL group and 81% of patients randomised to the imatinib group were still receiving first-line treatment. Discontinuation within 12 months due to disease progression occurred in 3% of SPRYCEL-treated patients and 5% of imatinib-treated patients.
With a minimum of 60 months follow-up, 60% of patients randomised to the SPRYCEL group and 63% of patients randomised to the imatinib group were still receiving first-line treatment. Discontinuation within 60 months due to disease progression occurred in 11% of SPRYCEL-treated patients and 14% of imatinib-treated patients.
Efficacy results are presented in Table 9. A statistically significantly greater proportion of patients in the SPRYCEL group achieved a cCCyR compared with patients in the imatinib group within the first 12 months of treatment. Efficacy of SPRYCEL was consistently demonstrated across different subgroups, including age, gender, and baseline Hasford score.
Table 9. Efficacy results from a phase 3 study of newly diagnosed patients with chronic phase CML:
| SPRYCEL n=259 | imatinib n=260 | p-value | |
|---|---|---|---|
| Response rate (95% CI) | |||
| Cytogenetic response | |||
| within 12 months | |||
| cCCyRa | 76.8% (71.2–81.8) | 66.2% (60.1-71.9) | p<0.007* |
| CCyRb | 85.3% (80.4-89.4) | 73.5% (67.7-78.7) | - |
| within 24 months | |||
| cCCyRa | 80.3% | 74.2% | - |
| CCyRb | 87.3% | 82.3% | - |
| within 36 months | |||
| cCCyRa | 82.6% | 77.3% | - |
| CCyRb | 88.0% | 83.5% | - |
| within 48 months | |||
| cCCyRa | 82.6% | 78.5% | - |
| CCyRb | 87.6% | 83.8% | - |
| within 60 months | |||
| cCCyRa | 83.0% | 78.5% | - |
| CCyRβ | 88.0% | 83.8% | - |
| Major molecular responsec | |||
| 12 months | 52.1% (45.9-58.3) | 33.8% (28.1-39.9) | p<0.00003* |
| 24 months | 64.5% (58.3-70.3) | 50% (43.8-56.2) | - |
| 36 months | 69.1% (63.1-74.7) | 56.2% (49.9-62.3) | - |
| 48 months | 75.7% (70.0-80.8) | 62.7% (56.5-68.6) | - |
| 60 months | 76.4% (70.8-81.5) | 64.2% (58.1-70.1) | p=0.0021 |
| Hazard ratio (HR) | |||
| within 12 months (99.99% CI) | |||
| Time-to cCCyR | 1.55 (1.0-2.3) | p<0.0001* | |
| Time-to MMR | 2.01 (1.2-3.4) | p<0.0001* | |
| Durability of cCCyR | 0.7 (0.4-1.4) | p<0.035 | |
| within 24 months (95% CI) | |||
| Time-to cCCyR | 1.49 (1.22-1.82) | - | |
| Time-to MMR | 1.69 (1.34-2.12) | - | |
| Durability of cCCyR | 0.77 (0.55-1.10) | - | |
| within 36 months (95% CI) | |||
| Time-to cCCyR | 1.48 (1.22-1.80) | - | |
| Time-to MMR | 1.59 (1.28-1.99) | - | |
| Durability of cCCyR | 0.77 (0.53-1.11) | - | |
| within 48 months (95% CI) | |||
| Time-to cCCyR | 1.45 (1.20-1.77) | - | |
| Time-to MMR | 1.55 (1.26-1.91) | - | |
| Durability of cCCyR | 0.81 (0.56-1.17) | - | |
| within 60 months (95% CI) | |||
| Time-to cCCyR | 1.46 (1.20-1.77) | p=0.0001 | |
| Time-to MMR | 1.54 (1.25-1.89) | p<0.0001 | |
| Durability of cCCyR | 0.79 (0.55-1.13) | p=0.1983 | |
a Confirmed complete cytogenetic response (cCCyR) is defined as a response noted on two consecutive occasions (at least 28 days apart).
b Complete cytogenetic response (CCyR) is based on a single bone marrow cytogenetic evaluation.
c Major molecular response (at any time) was defined as BCR ABL ratios ≤ 0.1% by RQ PCR in peripheral blood samples standardised on the International scale. These are cumulative rates representing minimum follow up for the timeframe specified.
* Adjusted for Hasford Score and indicated statistical significance at a pre-defined nominal level of significance.
CI = confidence interval
After 60 months of follow-up, median time to cCCyR was 3.1 months in the SPRYCEL group and 5.8 months in the imatinib group in patients with a confirmed CCyR. Median time to MMR after 60 months of follow-up was 9.3 months in the SPRYCEL group and 15.0 months in the imatinib group in patients with a MMR. These results are consistent with those seen at 12, 24 and 36 months.
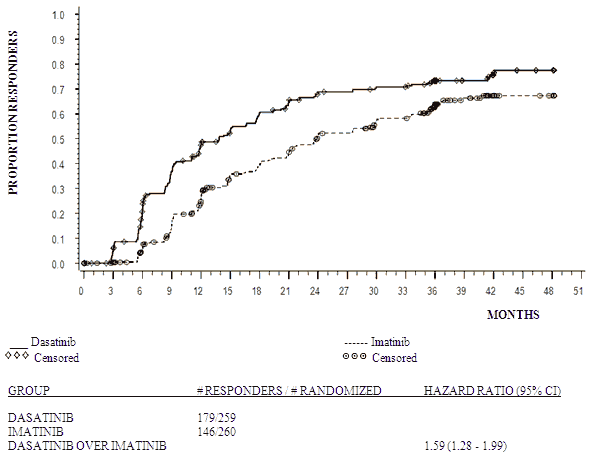
The time to MMR is displayed graphically in Figure 1. The time to MMR was consistently shorter in dasatinib-treated patients compared with imatinib-treated patients.
Figure 1. Kaplan-Meier estimate of time to major molecular response (MMR):
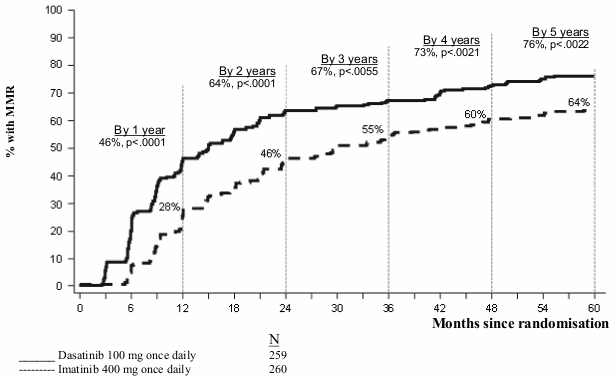
The rates of cCCyR in the SPRYCEL and imatinib treatment groups, respectively, within 3 months (54% and 30%), 6 months (70% and 56%), 9 months (75% and 63%), 24 months (80% and 74%), 36 months (83% and 77%), 48 months (83% and 79%) and 60 months (83% and 79%) were consistent with the primary endpoint. The rates of MMR in the SPRYCEL and imatinib treatment groups, respectively, within 3 months (8% and 0.4%), 6 months (27% and 8%), 9 months (39% and 18%), 12 months (46% and 28%), 24 months (64% and 46%), 36 months (67% and 55%), 48 months (73% and 60%) and 60 months (76% and 64%)were also consistent with the primary endpoint.
MMR rates by specific time point are displayed graphically in Figure 2. Rates of MMR were consistently higher in dasatinib-treated patients compared with imatinib-treated patients.
Figure 2. MMR rates over time – all randomised patients in a phase 3 study of newly diagnosed patients with chronic phase CML:
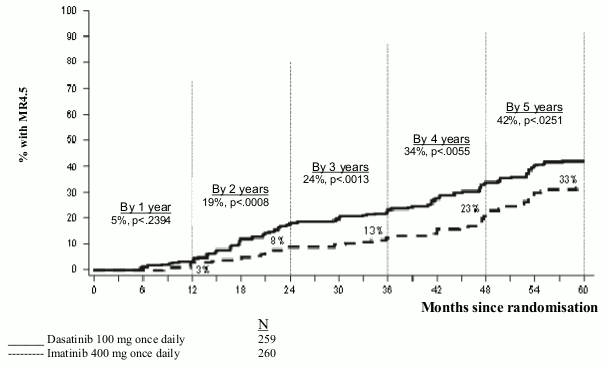
The proportion of patients achieving BCR-ABL ratio of ≤0.01% (4-log reduction) at any time was higher in the SPRYCEL group compared to the imatinib group (54.1% versus 45%). The proportion of patients achieving BCR-ABL ratio of ≤0.0032% (4.5-log reduction) at any time was higher in the SPRYCEL group compared to the imatinib group (44% versus 34%).
MR4.5 rates over time are displayed graphically in Figure 3. Rates of MR4.5 over time were consistently higher in dasatinib-treated patients compared with imatinib-treated patients.
Figure 3. MR4.5 rates over time – all randomised patients in a phase 3 study of newly diagnosed patients with chronic phase CML:
The rate of MMR at any time in each risk group determined by Hasford score was higher in the SPRYCEL group compared with the imatinib group (low risk: 90% and 69%; intermediate risk: 71% and 65%; high risk: 67% and 54%, respectively).
In an additional analysis, more dasatinib-treated patients (84%) achieved early molecular response (defined as BCR-ABL levels ≤ 10% at 3 months) compared with imatinib-treated patients (64%). Patients achieving early molecular response had a lower risk of transformation, higher rate of progression-free survival (PFS) and higher rate of overall survival (OS), as shown in Table 10.
Table 10. Dasatinib patients with BCR-ABL ≤10% and >10% at 3 months:*
| Dasatinib N=235 | Patients with BCR-ABL ≤10% at 3 months | Patients with BCR-ABL >10% at 3 months |
|---|---|---|
| Number of patients (%) | 198 (84.3) | 37 (15.7) |
| Transformation at 60 months, n/N (%) | 6/198 (3.0) | 5/37 (13.5) |
| Rate of PFS at 60 months (95% CI) | 92.0% (89.6, 95.2) | 73.8% (52.0, 86.8) |
| Rate of OS at 60 months (95% CI) | 93.8% (89.3, 96.4) | 80.6% (63.5, 90.2) |
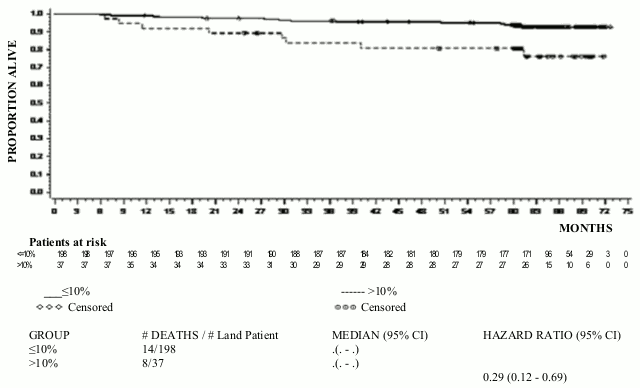
The OS rate by specific time point is displayed graphically in Figure 4. Rate of OS was consistently higher in dasatinib treated patients who achieved BCR-ABL level ≤10% at 3 months than those who did not.
Figure 4. Landmark plot for overall survival for dasatinib by BCR-ABL level (≤10% or >10%) at 3 months in a phase 3 study of newly diagnosed patients with chronic phase CML:
Disease progression was defined as increasing white blood cells despite appropriate therapeutic management, loss of CHR, partial CyR or CCyR, progression to accelerated phase or blast phase, or death. The estimated 60-month PFS rate was 88.9% (CI: 84% - 92.4%) for both the dasatinib and imatinib treatment groups. At 60 months, transformation to accelerated or blast phase occurred in fewer dasatinib-treated patients (n=8; 3%) compared with imatinib-treated patients (n=15; 5.8%). The estimated 60-month survival rates for dasatinib and imatinib-treated patients were 90.9% (CI: 86.6%-93.8%) and 89.6% (CI: 85.2%-92.8%), respectively. There was no difference in OS (HR 1.01, 95% CI: 0.58-1.73, p=0.9800) and PFS (HR 1.00, 95% CI: 0.58-1.72, p=0.9998) between dasatinib and imatinib.
In patients who report disease progression or discontinue dasatinib or imatinib therapy, BCR-ABL sequencing was performed on blood samples from patients where these are available. Similar rates of mutation were observed in both the treatment arms. The mutations detected among the dasatinib-treated patients were T315I, F317I/L and V299L. A different spectrum of mutation was detected in the imatinib treatment arm. Dasatinib does not appear to be active against the T315I mutation, based on in vitro data.
Chronic phase CML – Resistance or intolerance to prior imatinib therapy
Two clinical studies were conducted in patients resistant or intolerant to imatinib; the primary efficacy endpoint in these studies was Major Cytogenetic Response (MCyR).
Study 1
An open-label, randomised, non-comparative multicentre study was conducted in patients who failed initial treatment with 400 or 600 mg imatinib. They were randomised (2:1) to either dasatinib (70 mg twice daily) or imatinib (400 mg twice daily). Crossover to the alternative treatment arm was allowed if patients showed evidence of disease progression or intolerance that could not be managed by dose modification. The primary endpoint was MCyR at 12 weeks. Results are available for 150 patients: 101 were randomised to dasatinib and 49 to imatinib (all imatinib-resistant). The median time from diagnosis to randomisation was 64 months in the dasatinib group and 52 months in the imatinib group. All patients were extensively pretreated. Prior complete haematologic response (CHR) to imatinib was achieved in 93% of the overall patient population. A prior MCyR to imatinib was achieved in 28% and 29% of the patients in the dasatinib and imatinib arms, respectively.
Median duration of treatment was 23 months for dasatinib (with 44% of patients treated for >24 months to date) and 3 months for imatinib (with 10% of patients treated for >24 months to date). Ninety-three percent of patients in the dasatinib arm and 82% of patients in the imatinib arm achieved a CHR prior to crossover.
At 3 months, a MCyR occurred more often in the dasatinib arm (36%) than in the imatinib arm (29%). Notably, 22% of patients reported a complete cytogenetic response (CCyR) in the dasatinib arm while only 8% achieved a CCyR in the imatinib arm. With longer treatment and follow-up (median of 24 months), MCyR was achieved in 53% of the dasatinib-treated patients (CCyR in 44%) and 33% of the imatinib-treated patients (CCyR in 18%) prior to crossover. Among patients who had received imatinib 400 mg prior to study entry, MCyR was achieved in 61% of patients in the dasatinib arm and 50% in the imatinib arm.
Based on the Kaplan-Meier estimates, the proportion of patients who maintained MCyR for 1 year was 92% (95% CI: [85%-100%]) for dasatinib (CCyR 97%, 95% CI: [92%-100%]) and 74% (95% CI: [49%-100%]) for imatinib (CCyR 100%). The proportion of patients who maintained MCyR for 18 months was 90% (95% CI: [82%-98%]) for dasatinib (CCyR 94%, 95% CI: [87%-100%]) and 74% (95% CI: [49%-100%]) for imatinib (CCyR 100%). Based on the Kaplan-Meier estimates, the proportion of patients who had progression-free survival (PFS) for 1 year was 91% (95% CI: [85%-97%]) for dasatinib and 73% (95% CI: [54%-91%]) for imatinib. The proportion of patients who had PFS at 2 years was 86% (95% CI: [78%-93%]) for dasatinib and 65% (95% CI: [43%-87%]) for imatinib.
A total of 43% of the patients in the dasatinib arm, and 82% in the imatinib arm had treatment failure, defined as disease progression or cross-over to the other treatment (lack of response, intolerance of study medicinal product, etc.).
The rate of major molecular response (defined as BCR-ABL/control transcripts ≤ 0.1% by RQ-PCR in peripheral blood samples) prior to crossover was 29% for dasatinib and 12% for imatinib.
Study 2
An open-label, single-arm, multicentre study was conducted in patients resistant or intolerant to imatinib (i.e. patients who experienced significant toxicity during treatment with imatinib that precluded further treatment).
A total of 387 patients received dasatinib 70 mg twice daily (288 resistant and 99 intolerant). The median time from diagnosis to start of treatment was 61 months. The majority of the patients (53%) had received prior imatinib treatment for more than 3 years. Most resistant patients (72%) had received >600 mg imatinib. In addition to imatinib, 35% of patients had received prior cytotoxic chemotherapy, 65% had received prior interferon, and 10% had received a prior stem cell transplant. Thirty-eight percent of patients had baseline mutations known to confer imatinib resistance. Median duration of treatment on dasatinib was 24 months with 51% of patients treated for > 24 months to date. Efficacy results are reported in Table 11. MCyR was achieved in 55% of imatinib-resistant patients and 82% of imatinib-intolerant patients. With a minimum of 24 months follow-up, 21 of the 240 patients who had achieved a MCyR had progressed and the median duration of MCyR had not been reached.
Based on the Kaplan-Meier estimates, 95% (95% CI: [92%-98%]) of the patients maintained MCyR for 1 year and 88% (95% CI: [83%-93%]) maintained MCyR for 2 years. The proportion of patients who maintained CCyR for 1 year was 97% (95% CI: [94%-99%]) and for 2 years was 90% (95% CI: [86%-95%]). Forty-two percent of the imatinib-resistant patients with no prior MCyR to imatinib (n=188) achieved a MCyR with dasatinib.
There were 45 different BCR-ABL mutations in 38% of patients enrolled in this study. Complete haematologic response or MCyR was achieved in patients harbouring a variety of BCR-ABL mutations associated with imatinib resistance except T315I. The rates of MCyR at 2 years were similar whether patients had any baseline BCR-ABL mutation, P-loop mutation, or no mutation (63%, 61% and 62%, respectively).
Among imatinib-resistant patients, the estimated rate of PFS was 88% (95% CI: [84%-92%]) at 1 year and 75% (95% CI: [69%-81%]) at 2 years. Among imatinib-intolerant patients, the estimated rate of PFS was 98% (95% CI: [95%-100%]) at 1 year and 94% (95% CI: [88%-99%]) at 2 years.
The rate of major molecular response at 24 months was 45% (35% for imatinib-resistant patients and 74% for imatinib-intolerant patients).
Accelerated phase CML
An open-label, single-arm, multicentre study was conducted in patients intolerant or resistant to imatinib. A total of 174 patients received dasatinib 70 mg twice daily (161 resistant and 13 intolerant to imatinib). The median time from diagnosis to start of treatment was 82 months. Median duration of treatment on dasatinib was 14 months with 31% of patients treated for > 24 months to date. The rate of major molecular response (assessed in 41 patients with a CCyR) was 46% at 24 months. Further efficacy results are reported in Table 11.
Myeloid blast phase CML
An open-label, single-arm, multicentre study was conducted in patients intolerant or resistant to imatinib. A total of 109 patients received dasatinib 70 mg twice daily (99 resistant and 10 intolerant to imatinib). The median time from diagnosis to start of treatment was 48 months. Median duration of treatment on dasatinib was 3.5 months with 12% of patients treated for > 24 months to date. The rate of major molecular response (assessed in 19 patients with a CCyR) was 68% at 24 months. Further efficacy results are reported in Table 11.
Lymphoid blast phase CML and Ph+ ALL
An open-label, single-arm, multicentre study was conducted in patients with lymphoid blast phase CML or Ph+ ALL who were resistant or intolerant to prior imatinib therapy. A total of 48 patients with lymphoid blast CML received dasatinib 70 mg twice daily (42 resistant and 6 intolerant to imatinib). The median time from diagnosis to start of treatment was 28 months. Median duration of treatment on dasatinib was 3 months with 2% treated for >24 months to date. The rate of major molecular response (all 22 treated patients with a CCyR) was 50% at 24 months. In addition, 46 patients with Ph+ ALL received dasatinib 70 mg twice daily (44 resistant and 2 intolerant to imatinib). The median time from diagnosis to start of treatment was 18 months. Median duration of treatment on dasatinib was 3 months with 7% of patients treated for >24 months to date. The rate of major molecular response (all 25 treated patients with a CCyR) was 52% at 24 months. Further efficacy results are reported in Table 11. Of note, major haematologic responses (MaHR) were achieved quickly (most within 35 days of first dasatinib administration for patients with lymphoid blast CML, and within 55 days for patients with Ph+ ALL).
Table 11. Efficacy in phase II SPRYCEL single-arm clinical studiesa:
| Chronic (n=387) | Accelerated (n=174) | Myeloid blast (n=109) | Lymphoid blast (n=48) | Ph+ ALL (n=46) | |
|---|---|---|---|---|---|
| Haematologic response rateb (%) | |||||
| MaHR (95% CI) | n/a | 64% (57-72) | 33% (24-43) | 35% (22-51) | 41% (27-57) |
| CHR (95% CI) | 91% (88-94) | 50% (42-58) | 26% (18-35) | 29% (17-44) | 35% (21-50) |
| NEL (95% CI) | n/a | 14% (10-21) | 7% (3-14) | 6% (1-17) | 7% (1-18) |
| Duration of MaHR (%, Kaplan-Meier estimates) | |||||
| 1 year | n/a | 79% (71-87) | 71% (55-87) | 29% (3-56) | 32% (8-56) |
| 2 year | n/a | 60% (50-70) | 41% (21-60) | 10% (0-28) | 24% (2-47) |
| Cytogenetic responsec (%) | |||||
| MCyR (95% CI) | 62% (57-67) | 40% (33-48) | 34% (25-44) | 52% (37-67) | 57% (41-71) |
| CCyR (95% CI) | 54% (48-59) | 33% (26-41) | 27% (19-36) | 46% (31-61) | 54% (39-69) |
| Survival (%, Kaplan-Meier estimates) | |||||
| Progression-Free | |||||
| 1 year | 91% (88-94) | 64% (57-72) | 35% (25-45) | 14% (3-25) | 21% (9-34) |
| 2 year | 80% (75-84) | 46% (38-54) | 20% (11-29) | 5% (0-13) | 12% (2-23) |
| Overall | |||||
| 1 year | 97% (95-99) | 83% (77-89) | 48% (38-59) | 30% (14-47) | 35% (20-51) |
| 2 year | 94% (91-97) | 72% (64-79) | 38% (27-50) | 26% (10-42) | 31% (16-47) |
Data described in this table are from studies using a starting dose of 70 mg twice daily. See section 4.2 for the recommended starting dose.
a Numbers in bold font are the results of primary endpoints.
b Haematologic response criteria (all responses confirmed after 4 weeks): Major haematologic response (MaHR) = complete haematologic response (CHR) + no evidence of leukaemia (NEL).
CHR (chronic CML): WBC ≤ institutional ULN, platelets < 450,000/mm³, no blasts or promyelocytes in peripheral blood, <5% myelocytes plus metamyelocytes in peripheral blood, basophils in peripheral blood <20%, and no extramedullary involvement.
CHR (advanced CML/Ph+ ALL): WBC ≤ institutional ULN, ANC ≥1,000/mm³, platelets ≥100,000/mm³, no blasts or promyelocytes in peripheral blood, bone marrow blasts ≤5%, <5% myelocytes plus metamyelocytes in peripheral blood, basophils in peripheral blood <20%, and no extramedullary involvement.
NEL: same criteria as for CHR but ANC ≥500/mm³ and <1,000/mm³, or platelets ≥20,000/mm³ and ≤100,000/mm³.
c Cytogenetic response criteria: complete (0% Ph+ metaphases) or partial (>0%-35%). MCyR (0%-35%) combines both complete and partial responses.
n/a = not applicable; CI = confidence interval; ULN = upper limit of normal range.
The outcome of patients with bone marrow transplantation after dasatinib treatment has not been fully evaluated.
Phase III clinical studies in patients with CML in chronic, accelerated, or myeloid blast phase, and Ph+ ALL who were resistant or intolerant to imatinib
Two randomised, open-label studies were conducted to evaluate the efficacy of dasatinib administered once daily compared with dasatinib administered twice daily. Results described below are based on a minimum of 2 years and 7 years follow-up after the start of dasatinib therapy.
Study 1
In the study in chronic phase CML, the primary endpoint was MCyR in imatinib-resistant patients. The main secondary endpoint was MCyR by total daily dose level in the imatinib-resistant patients. Other secondary endpoints included duration of MCyR, PFS, and overall survival. A total of 670 patients, of whom 497 were imatinib-resistant, were randomised to the dasatinib 100 mg once daily, 140 mg once daily, 50 mg twice daily, or 70 mg twice daily group. The median duration of treatment for all patients still on therapy with a minimum of 5 years of follow-up (n=205) was 59 months (range 28-66 months). Median duration of treatment for all patients at 7 years of follow-up was 29.8 months (range <1-92.9 months).
Efficacy was achieved across all dasatinib treatment groups with the once daily schedule demonstrating comparable efficacy (non-inferiority) to the twice daily schedule on the primary efficacy endpoint (difference in MCyR 1.9%; 95% confidence interval [-6.8% - 10.6%]); however, the 100 mg once daily regimen demonstrated improved safety and tolerability. Efficacy results are presented in Tables 12 and 13.
Table 12. Efficacy of SPRYCEL in phase III dose-optimization study: imatinib resistant or intolerant chronic phase CML (2-year results)a:
| All patients | n=167 |
|---|---|
| Imatinib-resistant patients | n=124 |
| Haematologic response rateb () (95 CI) | |
| CHR | 92% (86-95) |
| Cytogenetic responsec () (95 CI) | |
| MCyR | |
| All patients | 63% (56-71) |
| Imatinib-resistant patients | 59% (50-68) |
| CCyR | |
| All patients | 50% (42-58) |
| Imatinib-resistant patients | 44% (35-53) |
| Major molecular response in patients achieving CCyRd () (95 CI) | |
| All patients | 69% (58-79) |
| Imatinib-resistant patients | 72% (58-83) |
a Results reported in recommended starting dose of 100 mg once daily.
b Haematologic response criteria (all responses confirmed after 4 weeks): Complete haematologic response (CHR) (chronic CML): WBC ≤ institutional ULN, platelets <450,000/mm³, no blasts or promyelocytes in peripheral blood, <5% myelocytes plus metamyelocytes in peripheral blood, basophils in peripheral blood <20%, and no extramedullary involvement.
c Cytogenetic response criteria: complete (0% Ph+ metaphases) or partial (>0%–35%). MCyR (0%–35%) combines both complete and partial responses.
d Major molecular response criteria: Defined as BCR-ABL/control transcripts ≤0.1% by RQ-PCR in peripheral blood samples
Table 13. Long term efficacy of SPRYCEL in phase 3 dose optimisation study: imatinib resistant or intolerant chronic phase CML patientsa:
| Minimum follow-up period | ||||
|---|---|---|---|---|
| 1 year | 2 years | 5 years | 7 years | |
| Major molecular response | ||||
| All patients | Μ/Δ | 37% (57/154) | 44% (71/160) | 46% (73/160) |
| Imatinib-resistant patients | Μ/Δ | 35% (41/117) | 42% (50/120) | 43% (51/120) |
| Imatinib-intolerant patients | Μ/Δ | 43% (16/37) | 53% (21/40) | 55% (22/40) |
| Progression-free survivalb | ||||
| All patients | 90% (86, 95) | 80% (73, 87) | 51% (41, 60) | 42% (33, 51) |
| Imatinib-resistant patients | 88% (82, 94) | 77% (68, 85) | 49% (39, 59) | 39% (29, 49) |
| Imatinib-intolerant patients | 97% (92, 100) | 87% (76, 99) | 56% (37, 76) | 51% (32, 67) |
| Overall survival | ||||
| All patients | 96% (93, 99) | 91% (86, 96) | 78% (72, 85) | 65% (56, 72) |
| Imatinib-resistant patients | 94% (90, 98) | 89% (84, 95) | 77% (69, 85) | 63% (53, 71) |
| Imatinib-intolerant patients | 100% (100, 100) | 95% (88, 100) | 82% (70, 94) | 70% (52, 82) |
a Results reported in recommended starting dose of 100 mg once daily.
b Progression was defined as increasing WBC count, loss of CHR or MCyR, ≥30% increase in Ph+ metaphases, confirmed AP/BP disease or death. PFS was analysed on an intent-to-treat principle and patients were followed to events including subsequent therapy.
Based on the Kaplan-Meier estimates, the proportion of patients treated with dasatinib 100 mg once daily who maintained MCyR for 18 months was 93% (95% CI: [88%-98%]).
Efficacy was also assessed in patients who were intolerant to imatinib. In this population of patients who received 100 mg once daily, MCyR was achieved in 77% and CCyR in 67%.
Study 2
In the study in advanced phase CML and Ph+ ALL, the primary endpoint was MaHR. A total of 611 patients were randomised to either the dasatinib 140 mg once daily or 70 mg twice daily group. Median duration of treatment was approximately 6 months (range 0.03-31 months).
The once daily schedule demonstrated comparable efficacy (non-inferiority) to the twice daily schedule on the primary efficacy endpoint (difference in MaHR 0.8%; 95% confidence interval [-7.1% - 8.7%]); however, the 140 mg once daily regimen demonstrated improved safety and tolerability. Response rates are presented in Table 14.
Table 14. Efficacy of SPRYCEL in phase III dose-optimisation study: advanced phase CML and Ph+ ALL (2 year results)a:
| Accelerated (n=158) | Myeloid blast (n=75) | Lymphoid blast (n=33) | Ph+ALL (n=40) | |
|---|---|---|---|---|
| MaHRb | 66% | 28% | 42% | 38% |
| (95% CI) | (59-74) | (18-40) | (26-61) | (23-54) |
| CHRb | 47% | 17% | 21% | 33% |
| (95% CI) | (40-56) | (10-28) | (9-39) | (19-49) |
| NELb | 19% | 11% | 21% | 5% |
| (95% CI) | (13-26) | (5-20) | (9-39) | (1-17) |
| MCyRc | 39% | 28% | 52% | 70% |
| (95% CI) | (31-47) | (18-40) | (34-69) | (54-83) |
| CCyR | 32% | 17% | 39% | 50% |
| (95% CI) | (25-40) | (10-28) | (23-58) | (34-66) |
a Results reported in recommended starting dose of 140 mg once daily (see section 4.2). Haematologic response criteria (all responses confirmed after 4 weeks): Major haematologic response (MaHR) = complete haematologic response (CHR) + no evidence of leukaemia (NEL).
CHR: WBC ≤ institutional ULN, ANC ≥1,000/mm³, platelets ≥100,000/mm³, no blasts or promyelocytes in peripheral blood, bone marrow blasts ≤5%, <5% myelocytes plus metamyelocytes in peripheral blood, basophils in peripheral blood < 20%, and no extramedullary involvement.
NEL: same criteria as for CHR but ANC ≥500/mm³ and <1,000/mm³, or platelets ≥20,000/mm³ and ≤100,000/mm³.
c MCyR combines both complete (0% Ph+ metaphases) and partial (>0%-35%) responses.
CI = confidence interval; ULN = upper limit of normal range.
In patients with accelerated phase CML treated with the 140 mg once daily regimen, the median duration of MaHR and the median overall survival was not reached and the median PFS was 25 months.
In patients with myeloid blast phase CML treated with the 140 mg once daily regimen, the median duration of MaHR was 8 months, the median PFS was 4 months, and the median overall survival was 8 months. In patients with lymphoid blast phase CML treated with the 140 mg once daily regimen, the median duration of MaHR was 5 months, the median PFS was 5 months, and the median overall survival was 11 months.
In patients with Ph+ ALL treated with the 140 mg once daily regimen, the median duration of MaHR was 5 months the median PFS was 4 months, and the median overall survival was 7 months.
Paediatric population
Paediatric patients with CML
Among 130 patients with chronic phase CML (CML-CP) treated in two paediatric studies, a Phase I, open-label, nonrandomized dose-ranging trial and a Phase II, open-label, nonrandomized trial, 84 patients (exclusively from the Phase II trial) were newly diagnosed with CML-CP and 46 patients (17 from the Phase I trial and 29 from the Phase II trial) were resistant or intolerant to previous treatment with imatinib. Ninety-seven of the 130 paediatric patients with CML-CP were treated with SPRYCEL tablets 60 mg/m² once daily (maximum dose of 100 mg once daily for patients with high BSA). Patients were treated until disease progression or unacceptable toxicity.
Key efficacy endpoints were: complete cytogenetic response (CCyR), major cytogenetic response (MCyR) and major molecular response (MMR). Results are shown in Table 15.
Table 15. Efficacy of SPRYCEL in paediatric patients with CML-CP:
| Cumulative response over time by minimum follow-up period | ||||
|---|---|---|---|---|
| 3 months | 6 months | 12 months | 24 months | |
| CCyR (95% CI) | ||||
| Newly diagnosed (N=51)a | 43.1% (29.3, 57.8) | 66.7% (52.1, 7.,2) | 96.1% (86.5, 99.5) | 96.1% (86.5, 99.5) |
| Prior imatinib (N=46)b | 45.7% (30.9, 61.0) | 71.7% (56.5, 8.,0) | 78.3% (63.6, 89.1) | 82.6% (68.6, 92.2) |
| MCyR (95% CI) | ||||
| Newly diagnosed (N=51)a | 60.8% (46.1, 74.2) | 90.2% (78.6, 9.,7) | 98.0% (89.6, 100) | 98.0% (89.6, 100) |
| Prior imatinib (N=46)b | 60.9% (45.4, 74.9) | 82.6% (68.6, 9.,2) | 89.1% (76.4, 96.4) | 89.1% (76.4, 96.4) |
| MMR (95% CI) | ||||
| Newly diagnosed (N=51)a | 7.8% (2.2, 18.9) | 31.4% (19.1, 45.9) | 56.9% (42.2, 70.7) | 74.5% (60.4, 85.7) |
| Prior imatinib (N=46)b | 15.2% (6.3, 28.9) | 26.1% (14.3, 41.1) | 39.1% (25.1, 54.6) | 52.2% (36.9, 67.1) |
a Patients from Phase II paediatric study of newly diagnosed CML-CP receiving oral tablet formulation
b Patients from Phase I and Phase II paediatric studies of imatinib-resistant or intolerant CML-CP receiving oral tablet formulation
In the Phase I paediatric study, after a minimum of 7 years of follow-up among the 17 patients with imatinib-resistant or intolerant CML-CP, the median duration of PFS was 53.6 months and the rate of OS was 82.4%.
In the Phase II paediatric study, in patients receiving the tablet formulation, estimated 24-month PFS rate among the 51 patients with newly diagnosed CML-CP was 94.0% (82.6, 98.0), and 81.7% (61.4, 92.0) among the 29 patients with imatinib-resistant/intolerant CML-CP. After 24 months of follow-up, OS in newly diagnosed patients was 100%, and 96.6% in imatinib-resistant or intolerant patients. In the Phase II paediatric study, 1 newly diagnosed patient and 2 imatinib-resistant or intolerant patients progressed to blast phase CML.
There were 33 newly diagnosed paediatric patients with CML-CP who received SPRYCEL powder for oral suspension at a dose of 72 mg/m². This dose represents 30% lower exposure compared to the recommended dose (see section 5.2. of Summary of Product Characteristics for SPRYCEL powder for oral suspension). In these patients, CCyR and MMR were CCyR: 87.9% [95% CI: (71.8-96.6)] and MMR: 45.5% [95% CI: (28.1-63.6)] at 12 months.
Among dasatinib-treated CML-CP paediatric patients previously exposed to imatinib, the mutations detected at the end of treatment were: T315A, E255K and F317L. However, E255K and F317L were also detected prior to treatment. There were no mutations detected in newly diagnosed CML-CP patients at the end of treatment.
Paediatric patients with ALL
The efficacy of SPRYCEL in combination with chemotherapy was evaluated in a pivotal study in paediatric patients over one year of age with newly diagnosed Ph+ ALL.
In this multicenter, historically-controlled Phase II study of dasatinib added to standard chemotherapy, 106 paediatric patients with newly diagnosed Ph+ ALL, of whom 104 patients had confirmed Ph+ ALL, received dasatinib at a daily dose of 60 mg/m² on a continuous dosing regimen for up to 24 months, in combination with chemotherapy. Eighty-two patients received dasatinib tablets exclusively and 24 patients received dasatinib powder for oral suspension at least once, 8 of whom received dasatinib powder for oral suspension exclusively. The backbone chemotherapy regimen was the same as used in the AIEOP-BFM ALL 2000 trial (chemotherapeutic standard multi-agent chemotherapy protocol). The primary efficacy endpoint was 3-year event-free survival (EFS), which was 65.5% (55.5, 73.7).
The minimal residual disease (MRD) negativity rate assessed by Ig/TCR rearrangement was 71.7% by the end of consolidation in all treated patients. When this rate was based on the 85 patients with evaluable Ig/TCR assessments, the estimate was 89.4%. The MRD negativity rates at the end of induction and consolidation as measured by flow cytometry were 66.0% and 84.0%, respectively.
Pharmacokinetic properties
The pharmacokinetics of dasatinib were evaluated in 229 adult healthy subjects and in 84 patients.
Absorption
Dasatinib is rapidly absorbed in patients following oral administration, with peak concentrations between 0.5-3 hours. Following oral administration, the increase in the mean exposure (AUCτ) is approximately proportional to the dose increment across doses ranging from 25 mg to 120 mg twice daily. The overall mean terminal half-life of dasatinib is approximately 5-6 hours in patients.
Data from healthy subjects administered a single 100 mg dose of dasatinib 30 minutes following a high-fat meal indicated a 14% increase in the mean AUC of dasatinib. A low-fat meal 30 minutes prior to dasatinib resulted in a 21% increase in the mean AUC of dasatinib. The observed food effects do not represent clinically relevant changes in exposure. Dasatinib exposure variability is higher under fasted conditions (47% CV) compared to light-fat meal (39% CV) and high-fat meal (32% CV) conditions.
Based on the patient population PK analysis, variability in dasatinib exposure was estimated to be mainly due to inter-occasion variability in bioavailability (44% CV) and, to a lesser extent, due to inter-individual variability in bioavailability and inter-individual variability in clearance (30% and 32% CV, respectively). The random inter-occasion variability in exposure is not expected to affect the cumulative exposure and efficacy or safety.
Distribution
In patients, dasatinib has a large apparent volume of distribution (2,505 L), coefficient of variation (CV% 93%), suggesting that the medicinal product is extensively distributed in the extravascular space. At clinically relevant concentrations of dasatinib, binding to plasma proteins was approximately 96% on the basis of in vitro experiments.
Biotransformation
Dasatinib is extensively metabolised in humans with multiple enzymes involved in the generation of the metabolites. In healthy subjects administered 100 mg of [ 14 C]-labelled dasatinib, unchanged dasatinib represented 29% of circulating radioactivity in plasma. Plasma concentration and measured in vitro activity indicate that metabolites of dasatinib are unlikely to play a major role in the observed pharmacology of the product. CYP3A4 is a major enzyme responsible for the metabolism of dasatinib.
Elimination
The mean terminal half-life of dasatinib is 3 hours to 5 hours. The mean apparent oral clearance is 363.8 L/hr (CV% 81.3%).
Elimination is predominantly in the faeces, mostly as metabolites. Following a single oral dose of [14C]-labelled dasatinib, approximately 89% of the dose was eliminated within 10 days, with 4% and 85% of the radioactivity recovered in the urine and faeces, respectively. Unchanged dasatinib accounted for 0.1% and 19% of the dose in urine and faeces, respectively, with the remainder of the dose as metabolites.
Hepatic and renal impairment
The effect of hepatic impairment on the single-dose pharmacokinetics of dasatinib was assessed in 8 moderately hepatic-impaired subjects who received a 50 mg dose and 5 severely hepatic-impaired subjects who received a 20 mg dose compared to matched healthy subjects who received a 70 mg dose of dasatinib. The mean C max and AUC of dasatinib adjusted for the 70 mg dose were decreased by 47% and 8%, respectively, in subjects with moderate hepatic impairment compared to subjects with normal hepatic function. In severely hepatic-impaired subjects, the mean C max and AUC adjusted for the 70 mg dose were decreased by 43% and 28%, respectively, compared to subjects with normal hepatic function (see sections 4.2 and 4.4).
Dasatinib and its metabolites are minimally excreted via the kidney.
Paediatric population
The pharmacokinetics of dasatinib have been evaluated in 104 paediatric patients with leukaemia or solid tumours (72 who received the tablet formulation and 32 who received the powder for oral suspension).
In a paediatric pharmacokinetics study, dose-normalized dasatinib exposure (Cavg, Cmin and Cmax) appears similar between 21 patients with CP-CML and 16 patients with Ph+ ALL.
Pharmacokinetics of the tablet formulation of dasatinib were evaluated for 72 paediatric patients with relapsed or refractory leukaemia or solid tumours at oral doses ranging from 60 to 120 mg/m² once daily and 50 to 110 mg/m² twice daily. Data was pooled across two studies and showed that dasatinib was rapidly absorbed. Mean Tmax was observed between 0.5 and 6 hours and mean half-life ranged from 2 to 5 hours across all dose levels and age groups. Dasatinib PK showed dose proportionality with a dose-related increase in exposure observed in paediatric patients. There was no significant difference of dasatinib PK between children and adolescents. The geometric means of dose-normalized dasatinib Cmax, AUC (0-T), and AUC (INF) appeared to be similar between children and adolescents at different dose levels. A PPK model-based simulation predicted that the body weight tiered dosing recommendation described for the tablet, in section 4.2, is expected to provide similar exposure to a tablet dose of 60 mg/m². These data should be considered if patients are to switch from tablets to powder for oral suspension or vice versa.
Preclinical safety data
The non-clinical safety profile of dasatinib was assessed in a battery of in vitro and in vivo studies in mice, rats, monkeys, and rabbits.
The primary toxicities occurred in the gastrointestinal, haematopoietic, and lymphoid systems. Gastrointestinal toxicity was dose-limiting in rats and monkeys, as the intestine was a consistent target organ. In rats, minimal to mild decreases in erythrocyte parameters were accompanied by bone marrow changes; similar changes occurred in monkeys at a lower incidence. Lymphoid toxicity in rats consisted of lymphoid depletion of the lymph nodes, spleen, and thymus, and decreased lymphoid organ weights. Changes in the gastrointestinal, haematopoietic and lymphoid systems were reversible following cessation of treatment.
Renal changes in monkeys treated for up to 9 months were limited to an increase in background kidney mineralisation. Cutaneous haemorrhage was observed in an acute, single-dose oral study in monkeys but was not observed in repeat-dose studies in either monkeys or rats. In rats, dasatinib inhibited platelet aggregation in vitro and prolonged cuticle bleeding time in vivo, but did not invoke spontaneous haemorrhage.
Dasatinib activity in vitro in hERG and Purkinje fiber assays suggested a potential for prolongation of cardiac ventricular repolarisation (QT interval). However, in an in vivo single-dose study in conscious telemetered monkeys, there were no changes in QT interval or ECG wave form.
Dasatinib was not mutagenic in in vitro bacterial cell assays (Ames test) and was not genotoxic in an in vivo rat micronucleus study. Dasatinib was clastogenic in vitro to dividing Chinese Hamster Ovary (CHO) cells.
Dasatinib did not affect male or female fertility in a conventional rat fertility and early embryonic development study, but induced embryolethality at dose levels approximating human clinical exposures. In embryofoetal development studies, dasatinib likewise induced embryolethality with associated decreases in litter size in rats, as well as foetal skeletal alterations in both rats and rabbits. These effects occurred at doses that did not produce maternal toxicity, indicating that dasatinib is a selective reproductive toxicant from implantation through the completion of organogenesis.
In mice, dasatinib induced immunosuppression, which was dose-related and effectively managed by dose reduction and/or changes in dosing schedule. Dasatinib had phototoxic potential in an in vitro neutral red uptake phototoxicity assay in mouse fibroblasts. Dasatinib was considered to be non-phototoxic in vivo after a single oral administration to female hairless mice at exposures up to 3-fold the human exposure following administration of the recommended therapeutic dose (based on AUC).
In a two-year carcinogenicity study, rats were administered oral doses of dasatinib at 0.3, 1, and 3 mg/kg/day. The highest dose resulted in a plasma exposure (AUC) level generally equivalent to the human exposure at the recommended range of starting doses from 100 mg to 140 mg daily. A statistically significant increase in the combined incidence of squamous cell carcinomas and papillomas in the uterus and cervix of high-dose females and of prostate adenoma in low-dose males was noted. The relevance of the findings from the rat carcinogenicity study for humans is not known.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.