STELARA Solution for injection Ref.[108324] Active ingredients: Ustekinumab
Source: FDA, National Drug Code (US) Revision Year: 2022
12.1. Mechanism of Action
Ustekinumab is a human IgG1қ monoclonal antibody that binds with specificity to the p40 protein subunit used by both the IL-12 and IL-23 cytokines. IL-12 and IL-23 are naturally occurring cytokines that are involved in inflammatory and immune responses, such as natural killer cell activation and CD4+ T-cell differentiation and activation. In in vitro models, ustekinumab was shown to disrupt IL-12 and IL-23 mediated signaling and cytokine cascades by disrupting the interaction of these cytokines with a shared cell-surface receptor chain, IL-12Rβ1. The cytokines IL-12 and IL-23 have been implicated as important contributors to the chronic inflammation that is a hallmark of Crohn’s disease and ulcerative colitis. In animal models of colitis, genetic absence or antibody blockade of the p40 subunit of IL-12 and IL-23, the target of ustekinumab, was shown to be protective.
12.2. Pharmacodynamics
Psoriasis
In a small exploratory study, a decrease was observed in the expression of mRNA of its molecular targets IL-12 and IL-23 in lesional skin biopsies measured at baseline and up to two weeks post-treatment in subjects with psoriasis.
Ulcerative Colitis
In both study UC-1 (induction) and study UC-2 (maintenance), a positive relationship was observed between exposure and rates of clinical remission, clinical response, and endoscopic improvement. The response rate approached a plateau at the ustekinumab exposures associated with the recommended dosing regimen for maintenance treatment [see Clinical Studies (14.5)].
12.3. Pharmacokinetics
Absorption
In adult subjects with psoriasis, the median time to reach the maximum serum concentration (Tmax) was 13.5 days and 7 days, respectively, after a single subcutaneous administration of 45 mg (N=22) and 90 mg (N=24) of ustekinumab. In healthy subjects (N=30), the median Tmax value (8.5 days) following a single subcutaneous administration of 90 mg of ustekinumab was comparable to that observed in subjects with psoriasis.
Following multiple subcutaneous doses of STELARA in adult subjects with psoriasis, steady-state serum concentrations of ustekinumab were achieved by Week 28. The mean (±SD) steady-state trough serum ustekinumab concentrations were 0.69 ± 0.69 mcg/mL for patients less than or equal to 100 kg receiving a 45 mg dose and 0.74 ± 0.78 mcg/mL for patients greater than 100 kg receiving a 90 mg dose. There was no apparent accumulation in serum ustekinumab concentration over time when given subcutaneously every 12 weeks.
Following the recommended intravenous induction dose, mean ±SD peak serum ustekinumab concentration was 125.2 ± 33.6 mcg/mL in patients with Crohn’s disease, and 129.1 ± 27.6 mcg/mL in patients with ulcerative colitis. Starting at Week 8, the recommended subcutaneous maintenance dosing of 90 mg ustekinumab was administered every 8 weeks. Steady state ustekinumab concentration was achieved by the start of the second maintenance dose. There was no apparent accumulation in ustekinumab concentration over time when given subcutaneously every 8 weeks. Mean ±SD steady-state trough concentration was 2.5 ± 2.1 mcg/mL in patients with Crohn’s disease, and 3.3 ± 2.3 mcg/mL in patients with ulcerative colitis for 90 mg ustekinumab administered every 8 weeks.
Distribution
Population pharmacokinetic analyses showed that the volume of distribution of ustekinumab in the central compartment was 2.7 L (95% CI: 2.69, 2.78) in patients with Crohn’s disease and 3.0 L (95% CI: 2.96, 3.07) in patients with ulcerative colitis. The total volume of distribution at steady-state was 4.6 L in patients with Crohn’s disease and 4.4 L in patients with ulcerative colitis.
Elimination
The mean (±SD) half-life ranged from 14.9 ± 4.6 to 45.6 ± 80.2 days across all psoriasis studies following subcutaneous administration. Population pharmacokinetic analyses showed that the clearance of ustekinumab was 0.19 L/day (95% CI: 0.185, 0.197) in patients with Crohn’s disease and 0.19 L/day (95% CI: 0.179, 0.192) in patients with ulcerative colitis with an estimated median terminal half-life of approximately 19 days for both IBD (Crohn’s disease and ulcerative colitis) populations.
These results indicate the pharmacokinetics of ustekinumab were similar between patients with Crohn’s disease and ulcerative colitis.
Metabolism
The metabolic pathway of ustekinumab has not been characterized. As a human IgG1κ monoclonal antibody, ustekinumab is expected to be degraded into small peptides and amino acids via catabolic pathways in the same manner as endogenous IgG.
Specific Populations
Weight
When given the same dose, subjects with psoriasis or psoriatic arthritis weighing more than 100 kg had lower median serum ustekinumab concentrations compared with those subjects weighing 100 kg or less. The median trough serum concentrations of ustekinumab in subjects of higher weight (greater than 100 kg) in the 90 mg group were comparable to those in subjects of lower weight (100 kg or less) in the 45 mg group.
Age: Geriatric Population
A population pharmacokinetic analysis (N=106/1937 patients with psoriasis greater than or equal to 65 years old) was performed to evaluate the effect of age on the pharmacokinetics of ustekinumab. There were no apparent changes in pharmacokinetic parameters (clearance and volume of distribution) in subjects older than 65 years old.
Age: Pediatric Population
Following multiple recommended doses of STELARA in pediatric subjects 6 to 17 years of age with psoriasis, steady-state serum concentrations of ustekinumab were achieved by Week 28. At Week 28, the mean ±SD steady-state trough serum ustekinumab concentrations were 0.36 ± 0.26 mcg/mL and 0.54 ± 0.43 mcg/mL, respectively, in pediatric subjects 6 to 11 years of age and adolescent subjects 12 to 17 years of age.
Overall, the observed steady-state ustekinumab trough concentrations in pediatric patients with psoriasis were within the range of those observed for adult patients with psoriasis and adult patients with PsA after administration of STELARA.
Drug Interaction Studies
The effects of IL-12 or IL-23 on the regulation of CYP450 enzymes were evaluated in an in vitro study using human hepatocytes, which showed that IL-12 and/or IL-23 at levels of 10 ng/mL did not alter human CYP450 enzyme activities (CYP1A2, 2B6, 2C9, 2C19, 2D6, or 3A4). However, the clinical relevance of in vitro data has not been established [see Drug Interactions (7.3)].
No in vivo drug interaction studies have been conducted with STELARA.
Population pharmacokinetic analyses indicated that the clearance of ustekinumab was not impacted by concomitant MTX, NSAIDs, and oral corticosteroids, or prior exposure to a TNF blocker in patients with psoriatic arthritis.
In patients with Crohn’s disease and ulcerative colitis, population pharmacokinetic analyses did not indicate changes in ustekinumab clearance with concomitant use of corticosteroids or immunomodulators (AZA, 6-MP, or MTX); and serum ustekinumab concentrations were not impacted by concomitant use of these medications.
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Animal studies have not been conducted to evaluate the carcinogenic or mutagenic potential of STELARA. Published literature showed that administration of murine IL-12 caused an anti-tumor effect in mice that contained transplanted tumors and IL-12/IL-23p40 knockout mice or mice treated with anti-IL-12/IL-23p40 antibody had decreased host defense to tumors. Mice genetically manipulated to be deficient in both IL-12 and IL-23 or IL-12 alone developed UV-induced skin cancers earlier and more frequently compared to wild-type mice. The relevance of these experimental findings in mouse models for malignancy risk in humans is unknown.
No effects on fertility were observed in male cynomolgus monkeys that were administered ustekinumab at subcutaneous doses up to 45 mg/kg twice weekly (45 times the MRHD on a mg/kg basis) prior to and during the mating period. However, fertility and pregnancy outcomes were not evaluated in mated females.
No effects on fertility were observed in female mice that were administered an analogous IL-12/IL-23p40 antibody by subcutaneous administration at doses up to 50 mg/kg, twice weekly, prior to and during early pregnancy.
13.2. Animal Toxicology and/or Pharmacology
In a 26-week toxicology study, one out of 10 monkeys subcutaneously administered 45 mg/kg ustekinumab twice weekly for 26 weeks had a bacterial infection.
14. Clinical Studies
14.1 Psoriasis
Two multicenter, randomized, double-blind, placebo-controlled studies (Ps STUDY 1 and Ps STUDY 2) enrolled a total of 1996 subjects 18 years of age and older with plaque psoriasis who had a minimum body surface area involvement of 10%, and Psoriasis Area and Severity Index (PASI) score ≥12, and who were candidates for phototherapy or systemic therapy. Subjects with guttate, erythrodermic, or pustular psoriasis were excluded from the studies.
Ps STUDY 1 enrolled 766 subjects and Ps STUDY 2 enrolled 1230 subjects. The studies had the same design through Week 28. In both studies, subjects were randomized in equal proportion to placebo, 45 mg or 90 mg of STELARA . Subjects randomized to STELARA received 45 mg or 90 mg doses, regardless of weight, at Weeks 0, 4, and 16. Subjects randomized to receive placebo at Weeks 0 and 4 crossed over to receive STELARA (either 45 mg or 90 mg) at Weeks 12 and 16.
In both studies, the endpoints were the proportion of subjects who achieved at least a 75% reduction in PASI score (PASI 75) from baseline to Week 12 and treatment success (cleared or minimal) on the Physician’s Global Assessment (PGA). The PGA is a 6-category scale ranging from 0 (cleared) to 5 (severe) that indicates the physician’s overall assessment of psoriasis focusing on plaque thickness/induration, erythema, and scaling.
In both studies, subjects in all treatment groups had a median baseline PASI score ranging from approximately 17 to 18. Baseline PGA score was marked or severe in 44% of subjects in Ps STUDY 1 and 40% of subjects in Ps STUDY 2. Approximately two-thirds of all subjects had received prior phototherapy, 69% had received either prior conventional systemic or biologic therapy for the treatment of psoriasis, with 56% receiving prior conventional systemic therapy and 43% receiving prior biologic therapy. A total of 28% of subjects had a history of psoriatic arthritis.
Clinical Response
The results of Ps STUDY 1 and Ps STUDY 2 are presented in Table 8 below.
Table 8. Clinical Outcomes Ps STUDY 1 and Ps STUDY 2:
| Week 12 | Ps STUDY 1 | Ps STUDY 2 | ||||
|---|---|---|---|---|---|---|
| STELARA | STELARA | |||||
| Placebo | 45 mg | 90 mg | Placebo | 45 mg | 90 mg | |
| Subjects randomized | 255 | 255 | 256 | 410 | 409 | 411 |
| PASI 75 response | 8 (3%) | 171 (67%) | 170 (66%) | 15 (4%) | 273 (67%) | 311 (76%) |
| PGA of Cleared or Minimal | 10 (4%) | 151 (59%) | 156 (61%) | 18 (4%) | 277 (68%) | 300 (73%) |
Examination of age, gender, and race subgroups did not identify differences in response to STELARA among these subgroups.
In subjects who weighed 100 kg or less, response rates were similar with both the 45 mg and 90 mg doses; however, in subjects who weighed greater than 100 kg, higher response rates were seen with 90 mg dosing compared with 45 mg dosing (Table 9 below).
Table 9. Clinical Outcomes by Weight Ps STUDY 1 and Ps STUDY 2:
| Ps STUDY 1 | Ps STUDY 2 | |||||
|---|---|---|---|---|---|---|
| STELARA | STELARA | |||||
| Placebo | 45 mg | 90 mg | Placebo | 45 mg | 90 mg | |
| Subjects randomized | 255 | 255 | 256 | 410 | 409 | 411 |
| PASI 75 response at Week 12* | ||||||
| ≤100 kg | 4% | 74% | 65% | 4% | 73% | 78% |
| 6/166 | 124/168 | 107/164 | 12/290 | 218/297 | 225/289 | |
| >100 kg | 2% | 54% | 68% | 3% | 49% | 71% |
| 2/89 | 47/87 | 63/92 | 3/120 | 55/112 | 86/121 | |
| PGA of Cleared or Minimal at Week 12* | ||||||
| ≤100 kg | 4% | 64% | 63% | 5% | 74% | 75% |
| 7/166 | 108/168 | 103/164 | 14/290 | 220/297 | 216/289 | |
| >100 kg | 3% | 49% | 58% | 3% | 51% | 69% |
| 3/89 | 43/87 | 53/92 | 4/120 | 57/112 | 84/121 | |
* Patients were dosed with study medication at Weeks 0 and 4.
Subjects in Ps STUDY 1 who were PASI 75 responders at both Weeks 28 and 40 were re-randomized at Week 40 to either continued dosing of STELARA (STELARA at Week 40) or to withdrawal of therapy (placebo at Week 40). At Week 52, 89% (144/162) of subjects re-randomized to STELARA treatment were PASI 75 responders compared with 63% (100/159) of subjects re-randomized to placebo (treatment withdrawal after Week 28 dose). The median time to loss of PASI 75 response among the subjects randomized to treatment withdrawal was 16 weeks.
14.2 Adolescent Subjects with Plaque Psoriasis
A multicenter, randomized, double blind, placebo-controlled study (Ps STUDY 3) enrolled 110 adolescent subjects 12 to 17 years of age with a minimum BSA involvement of 10%, a PASI score greater than or equal to 12, and a PGA score greater than or equal to 3, who were candidates for phototherapy or systemic therapy and whose disease was inadequately controlled by topical therapy.
Subjects were randomized to receive placebo (n=37), the recommended dose of STELARA (n=36), or one-half the recommended dose of STELARA (n=37) by subcutaneous injection at Weeks 0 and 4 followed by dosing every 12 weeks (q12w). The recommended dose of STELARA was 0.75 mg/kg for subjects weighing less than 60 kg, 45 mg for subjects weighing 60 kg to 100 kg, and 90 mg for subjects weighing greater than 100 kg. At Week 12, subjects who received placebo were crossed over to receive STELARA at the recommended dose or one-half the recommended dose.
Of the adolescent subjects, approximately 63% had prior exposure to phototherapy or conventional systemic therapy and approximately 11% had prior exposure to biologics.
The endpoints were the proportion of patients who achieved a PGA score of cleared (0) or minimal (1), PASI 75, and PASI 90 at Week 12. Subjects were followed for up to 60 weeks following first administration of study agent.
Clinical Response
The efficacy results at Week 12 for Ps STUDY 3 are presented in Table 10.
Table 10. Summary of Efficacy Endpoints in the Adolescent Psoriasis Study at Week 12:
| Ps STUDY 3 | ||
|---|---|---|
| Placebo n (%) | STELARA* n (%) | |
| N | 37 | 36 |
| PGA | ||
| PGA of cleared (0) or minimal (1) | 2 (5.4%) | 25 (69.4%) |
| PASI | ||
| PASI 75 responders | 4 (10.8%) | 29 (80.6%) |
| PASI 90 responders | 2 (5.4%) | 22 (61.1%) |
14.3 Psoriatic Arthritis
The safety and efficacy of STELARA was assessed in 927 patients (PsA STUDY 1, n=615; PsA STUDY 2, n=312), in two randomized, double-blind, placebo-controlled studies in adult patients 18 years of age and older with active PsA (≥5 swollen joints and ≥5 tender joints) despite non-steroidal anti-inflammatory (NSAID) or disease modifying antirheumatic (DMARD) therapy. Patients in these studies had a diagnosis of PsA for at least 6 months. Patients with each subtype of PsA were enrolled, including polyarticular arthritis with the absence of rheumatoid nodules (39%), spondylitis with peripheral arthritis (28%), asymmetric peripheral arthritis (21%), distal interphalangeal involvement (12%) and arthritis mutilans (0.5%). Over 70% and 40% of the patients, respectively, had enthesitis and dactylitis at baseline.
Patients were randomized to receive treatment with STELARA 45 mg, 90 mg, or placebo subcutaneously at Weeks 0 and 4 followed by every 12 weeks (q12w) dosing. Approximately 50% of patients continued on stable doses of MTX (≤25 mg/week). The primary endpoint was the percentage of patients achieving ACR 20 response at Week 24.
In PsA STUDY 1 and PsA STUDY 2, 80% and 86% of the patients, respectively, had been previously treated with DMARDs. In PsA STUDY 1, previous treatment with anti-tumor necrosis factor (TNF)-α agent was not allowed. In PsA STUDY 2, 58% (n=180) of the patients had been previously treated with TNF blocker, of whom over 70% had discontinued their TNF blocker treatment for lack of efficacy or intolerance at any time.
Clinical Response
In both studies, a greater proportion of patients achieved ACR 20, ACR 50 and PASI 75 response in the STELARA 45 mg and 90 mg groups compared to placebo at Week 24 (see Table 11). ACR 70 responses were also higher in the STELARA 45 mg and 90 mg groups, although the difference was only numerical (p=NS) in STUDY 2. Responses were consistent in patients treated with STELARA alone or in combination with methotrexate. Responses were similar in patients regardless of prior TNFα exposure.
Table 11. ACR 20, ACR 50, ACR 70 and PASI 75 responses in PsA STUDY 1 and PsA STUDY 2 at Week 24:
| PsA STUDY 1 | PsA STUDY 2 | |||||
|---|---|---|---|---|---|---|
| STELARA | STELARA | |||||
| Placebo | 45 mg | 90 mg | Placebo | 45 mg | 90 mg | |
| Number of patients randomized | 206 | 205 | 204 | 104 | 103 | 105 |
| ACR 20 response, N (%) | 47 (23%) | 87 (42%) | 101 (50%) | 21 (20%) | 45 (44%) | 46 (44%) |
| ACR 50 response, N (%) | 18 (9%) | 51 (25%) | 57 (28%) | 7 (7%) | 18 (17%) | 24 (23%) |
| ACR 70 response, N (%) | 5 (2%) | 25 (12%) | 29 (14%) | 3 (3%) | 7 (7%) | 9 (9%) |
| Number of patients with ≥3% BSA* | 146 | 145 | 149 | 80 | 80 | 81 |
| PASI 75 response, N (%) | 16 (11%) | 83 (57%) | 93 (62%) | 4 (5%) | 41 (51%) | 45 (56%) |
* Number of patients with ≥3% BSA psoriasis skin involvement at baseline
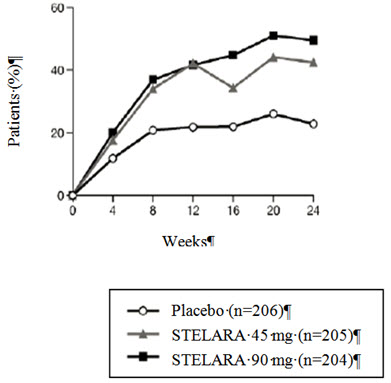
The percent of patients achieving ACR 20 responses by visit is shown in Figure 1.
Figure 1. Percent of patients achieving ACR 20 response through Week 24:
PsA STUDY 1
The results of the components of the ACR response criteria are shown in Table 12.
Table 12. Mean change from baseline in ACR components at Week 24:
| PsA STUDY 1 | |||
|---|---|---|---|
| STELARA | |||
| Placebo (N=206) | 45 mg (N=205) | 90 mg (N=204) | |
| Number of swollen joints* | |||
| Baseline | 15 | 12 | 13 |
| Mean Change at Week 24 | -3 | -5 | -6 |
| Number of tender joints† | |||
| Baseline | 25 | 22 | 23 |
| Mean Change at Week 24 | -4 | -8 | -9 |
| Patient’s assessment of pain‡ | |||
| Baseline | 6.1 | 6.2 | 6.6 |
| Mean Change at Week 24 | -0.5 | -2.0 | -2.6 |
| Patient global assessment‡ | |||
| Baseline | 6.1 | 6.3 | 6.4 |
| Mean Change at Week 24 | -0.5 | -2.0 | -2.5 |
| Physician global assessment‡ | |||
| Baseline | 5.8 | 5.7 | 6.1 |
| Mean Change at Week 24 | -1.4 | -2.6 | -3.1 |
| Disability index (HAQ)§ | |||
| Baseline | 1.2 | 1.2 | 1.2 |
| Mean Change at Week 24 | -0.1 | -0.3 | -0.4 |
| CRP (mg/dL)¶ | |||
| Baseline | 1.6 | 1.7 | 1.8 |
| Mean Change at Week 24 | 0.01 | -0.5 | -0.8 |
* Number of swollen joints counted (0–66)
† Number of tender joints counted (0–68)
‡ Visual analogue scale; 0 = best, 10 = worst.
§ Disability Index of the Health Assessment Questionnaire; 0 = best, 3 = worst, measures the patient’s ability to perform the following: dress/groom, arise, eat, walk, reach, grip, maintain hygiene, and maintain daily activity.
¶ CRP: (Normal Range 0.0–1.0 mg/dL)
An improvement in enthesitis and dactylitis scores was observed in each STELARA group compared with placebo at Week 24.
Physical Function
STELARA-treated patients showed improvement in physical function compared to patients treated with placebo as assessed by HAQ-DI at Week 24. In both studies, the proportion of HAQ-DI responders (≥0.3 improvement in HAQ-DI score) was greater in the STELARA 45 mg and 90 mg groups compared to placebo at Week 24.
14.4 Crohn’s Disease
STELARA was evaluated in three randomized, double-blind, placebo-controlled clinical studies in adult patients with moderately to severely active Crohn’s disease (Crohn’s Disease Activity Index [CDAI] score of 220 to 450). There were two 8-week intravenous induction studies (CD-1 and CD-2) followed by a 44-week subcutaneous randomized withdrawal maintenance study (CD-3) representing 52 weeks of therapy. Patients in CD-1 had failed or were intolerant to treatment with one or more TNF blockers, while patients in CD-2 had failed or were intolerant to treatment with immunomodulators or corticosteroids, but never failed treatment with a TNF blocker.
Studies CD-1 and CD-2
In studies CD-1 and CD-2, 1409 patients were randomized, of whom 1368 (CD-1, n=741; CD-2, n=627) were included in the final efficacy analysis. Induction of clinical response (defined as a reduction in CDAI score of greater than or equal to 100 points or CDAI score of less than 150) at Week 6 and clinical remission (defined as a CDAI score of less than 150) at Week 8 were evaluated. In both studies, patients were randomized to receive a single intravenous administration of STELARA at either approximately 6 mg/kg, placebo (see Table 4), or 130 mg (a lower dose than recommended).
In Study CD-1, patients had failed or were intolerant to prior treatment with a TNF blocker: 29% patients had an inadequate initial response (primary non-responders), 69% responded but subsequently lost response (secondary non-responders) and 36% were intolerant to a TNF blocker. Of these patients, 48% failed or were intolerant to one TNF blocker and 52% had failed 2 or 3 prior TNF blockers. At baseline and throughout the study, approximately 46% of the patients were receiving corticosteroids and 31% of the patients were receiving immunomodulators (AZA, 6-MP, MTX). The median baseline CDAI score was 319 in the STELARA approximately 6 mg/kg group and 313 in the placebo group.
In Study CD-2, patients had failed or were intolerant to prior treatment with corticosteroids (81% of patients), at least one immunomodulator (6-MP, AZA, MTX; 68% of patients), or both (49% of patients). Additionally, 69% never received a TNF blocker and 31% previously received but had not failed a TNF blocker. At baseline, and throughout the study, approximately 39% of the patients were receiving corticosteroids and 35% of the patients were receiving immunomodulators (AZA, 6-MP, MTX). The median baseline CDAI score was 286 in the STELARA and 290 in the placebo group.
In these induction studies, a greater proportion of patients treated with STELARA (at the recommended dose of approximately 6 mg/kg dose) achieved clinical response at Week 6 and clinical remission at Week 8 compared to placebo (see Table 13 for clinical response and remission rates). Clinical response and remission were significant as early as Week 3 in STELARA-treated patients and continued to improve through Week 8.
Table 13. Induction of Clinical Response and Remission in CD-1* and CD-2†:
| CD-1 n=741 | CD-2 n=627 | |||||
|---|---|---|---|---|---|---|
| Placebo N=247 | STELARA‡ N=249 | Treatment difference and 95% CI | Placebo N=209 | STELARA‡ N=209 | Treatment difference and 95% CI | |
| Clinical Response (100 point), Week 6 | 53 (21%) | 84 (34%)§ | 12% (4%, 20%) | 60 (29%) | 116 (56%)¶ | 27% (18%, 36%) |
| Clinical Remission, Week 8 | 18 (7%) | 52 (21%)¶ | 14% (8%, 20%) | 41 (20%) | 84 (40%)¶ | 21% (12%, 29%) |
| Clinical Response (100 point), Week 8 | 50 (20%) | 94 (38%)¶ | 18% (10%, 25%) | 67 (32%) | 121 (58%)¶ | 26% (17%, 35%) |
| 70 Point Response, Week 6 | 75 (30%) | 109 (44%)§ | 13% (5%, 22%) | 81 (39%) | 135 (65%)¶ | 26% (17%, 35%) |
| 70 Point Response, Week 3 | 67 (27%) | 101 (41%)§ | 13% (5%, 22%) | 66 (32%) | 106 (51%)¶ | 19% (10%, 28%) |
Clinical remission is defined as CDAI score <150; Clinical response is defined as reduction in CDAI score by at least 100 points or being in clinical remission: 70 point response is defined as reduction in CDAI score by at least 70 points.
* Patient population consisted of patients who failed or were intolerant to TNF blocker therapy
† Patient population consisted of patients who failed or were intolerant to corticosteroids or immunomodulators (e.g., 6-MP, AZA, MTX) and previously received but not failed a TNF blocker or were never treated with a TNF blocker.
‡ Infusion dose of STELARA using the weight-based dosage regimen specified in Table 4.
§ 0.001 ≤ p < 0.01
¶ p<0.001
Study CD-3
The maintenance study (CD-3), evaluated 388 patients who achieved clinical response (≥100 point reduction in CDAI score) at Week 8 with either induction dose of STELARA in studies CD-1 or CD-2. Patients were randomized to receive a subcutaneous maintenance regimen of either 90 mg STELARA every 8 weeks or placebo for 44 weeks (see Table 14).
Table 14. Clinical Response and Remission in CD-3 (Week 44; 52 weeks from initiation of the induction dose):
| Placebo* | 90 mg STELARA every 8 weeks | Treatment difference and 95% CI | |
|---|---|---|---|
| N=131† | N=128† | ||
| Clinical Remission | 47 (36%) | 68 (53%)‡ | 17% (5%, 29%) |
| Clinical Response | 58 (44%) | 76 (59%)§ | 15% (3%, 27%) |
| Clinical Remission in patients in remission at the start of maintenance therapy¶ | 36/79 (46%) | 52/78 (67%)‡ | 21% (6%, 36%) |
Clinical remission is defined as CDAI score <150; Clinical response is defined as reduction in CDAI of at least 100 points or being in clinical remission
* The placebo group consisted of patients who were in response to STELARA and were randomized to receive placebo at the start of maintenance therapy.
† Patients who achieved clinical response to STELARA at the end of the induction study.
‡ p<0.01
§ 0.01 ≤ p < 0.05
¶ Patients in remission at the end of maintenance therapy who were in remission at the start of maintenance therapy. This does not account for any other time point during maintenance therapy.
At Week 44, 47% of patients who received STELARA were corticosteroid-free and in clinical remission, compared to 30% of patients in the placebo group.
At Week 0 of Study CD-3, 34/56 (61%) STELARA-treated patients who previously failed or were intolerant to TNF blocker therapies were in clinical remission and 23/56 (41%) of these patients were in clinical remission at Week 44. In the placebo arm, 27/61 (44%) patients were in clinical remission at Week 0 while 16/61 (26%) of these patients were in remission at Week 44.
At Week 0 of Study CD-3, 46/72 (64%) STELARA-treated patients who had previously failed immunomodulator therapy or corticosteroids (but not TNF blockers) were in clinical remission and 45/72 (63%) of these patients were in clinical remission at Week 44. In the placebo arm, 50/70 (71%) of these patients were in clinical remission at Week 0 while 31/70 (44%) were in remission at Week 44. In the subset of these patients who were also naïve to TNF blockers, 34/52 (65%) of STELARA-treated patients were in clinical remission at Week 44 as compared to 25/51 (49%) in the placebo arm.
Patients who were not in clinical response 8 weeks after STELARA induction were not included in the primary efficacy analyses for Study CD-3; however, these patients were eligible to receive a 90 mg subcutaneous injection of STELARA upon entry into Study CD-3. Of these patients, 102/219 (47%) achieved clinical response eight weeks later and were followed for the duration of the study.
14.5 Ulcerative Colitis
STELARA was evaluated in two randomized, double-blind, placebo-controlled clinical studies [UC-1 and UC-2 (NCT02407236)] in adult patients with moderately to severely active ulcerative colitis who had an inadequate response to or failed to tolerate a biologic (i.e., TNF blocker and/or vedolizumab), corticosteroids, and/or 6-MP or AZA therapy. The 8-week intravenous induction study (UC-1) was followed by the 44-week subcutaneous randomized withdrawal maintenance study (UC-2) for a total of 52 weeks of therapy.
Disease assessment was based on the Mayo score, which ranged from 0 to 12 and has four subscores that were each scored from 0 (normal) to 3 (most severe): stool frequency, rectal bleeding, findings on centrally-reviewed endoscopy, and physician global assessment. Moderately to severely active ulcerative colitis was defined at baseline (Week 0) as Mayo score of 6 to 12, including a Mayo endoscopy subscore ≥2. An endoscopy score of 2 was defined by marked erythema, absent vascular pattern, friability, erosions; and a score of 3 was defined by spontaneous bleeding, ulceration. At baseline, patients had a median Mayo score of 9, with 84% of patients having moderate disease (Mayo score 6–10) and 15% having severe disease (Mayo score 11–12).
Patients in these studies may have received other concomitant therapies including aminosalicylates, immunomodulatory agents (AZA, 6-MP, or MTX), and oral corticosteroids (prednisone).
Study UC-1
In UC-1, 961 patients were randomized at Week 0 to a single intravenous administration of STELARA of approximately 6 mg/kg, 130 mg (a lower dose than recommended), or placebo. Patients enrolled in UC-1 had to have failed therapy with corticosteroids, immunomodulators or at least one biologic. A total of 51% had failed at least one biologic and 17% had failed both a TNF blocker and an integrin receptor blocker. Of the total population, 46% had failed corticosteroids or immunomodulators but were biologic-naïve and an additional 3% had previously received but had not failed a biologic. At induction baseline and throughout the study, approximately 52% patients were receiving oral corticosteroids, 28% patients were receiving immunomodulators (AZA, 6-MP, or MTX) and 69% patients were receiving aminosalicylates.
The primary endpoint was clinical remission at Week 8. Clinical remission with a definition of: Mayo stool frequency subscore of 0 or 1, Mayo rectal bleeding subscore of 0 (no rectal bleeding), and Mayo endoscopy subscore of 0 or 1 (Mayo endoscopy subscore of 0 defined as normal or inactive disease and Mayo subscore of 1 defined as presence of erythema, decreased vascular pattern and no friability) is provided in Table 15.
The secondary endpoints were clinical response, endoscopic improvement, and histologic-endoscopic mucosal improvement. Clinical response with a definition of (≥ 2 points and ≥ 30% decrease in modified Mayo score, defined as 3-component Mayo score without the Physician’s Global Assessment, with either a decrease from baseline in the rectal bleeding subscore ≥1 or a rectal bleeding subscore of 0 or 1), endoscopic improvement with a definition of Mayo endoscopy subscore of 0 or 1, and histologic-endoscopic mucosal improvement with a definition of combined endoscopic improvement and histologic improvement of the colon tissue [neutrophil infiltration in <5% of crypts, no crypt destruction, and no erosions, ulcerations, or granulation tissue]) are provided in Table 15.
In UC-1, a significantly greater proportion of patients treated with STELARA (at the recommended dose of approximately 6 mg/kg dose) were in clinical remission and response and achieved endoscopic improvement and histologic-endoscopic mucosal improvement compared to placebo (see Table 15).
Table 15. Proportion of Patients Meeting Efficacy Endpoints at Week 8 in UC-1:
| Endpoint | Placebo N=319 | STELARA* N=322 | Treatment difference and 97.5% CI† | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Clinical Remission‡ | 22 | 7% | 62 | 19% | 12% (7%, 18%)§ |
| Bio-naïve¶ | 14/151 | 9% | 36/147 | 24% | |
| Prior biologic failure | 7/161 | 4% | 24/166 | 14% | |
| Endoscopic Improvement# | 40 | 13% | 80 | 25% | 12% (6%, 19%)§ |
| Bio-naïve¶ | 28/151 | 19% | 43/147 | 29% | |
| Prior biologic failure | 11/161 | 7% | 34/166 | 20% | |
| Clinical ResponseÞ | 99 | 31% | 186 | 58% | 27% (18%, 35%)§ |
| Bio-naïve¶ | 55/151 | 36% | 94/147 | 64% | |
| Prior biologic failure | 42/161 | 26% | 86/166 | 52% | |
| Histologic-Endoscopic Mucosal Improvementß | 26 | 8% | 54 | 17% | 9% (3%, 14%)§ |
| Bio-naïve¶ | 19/151 | 13% | 30/147 | 20% | |
| Prior biologic failure | 6/161 | 4% | 21/166 | 13% | |
* Infusion dose of STELARA using the weight-based dosage regimen specified in Table 4.
† Adjusted treatment difference (97.5% CI)
‡ Clinical remission was defined as Mayo stool frequency subscore of 0 or 1, Mayo rectal bleeding subscore of 0, and Mayo endoscopy subscore of 0 or 1 (modified so that 1 does not include friability).
§ p<0.001
¶ An additional 7 patients on placebo and 9 patients on STELARA (6 mg/kg) had been exposed to, but had not failed, biologics.
# Endoscopic improvement was defined as Mayo endoscopy subscore of 0 or 1 (modified so that 1 does not include friability).
Þ Clinical response was defined as a decrease from baseline in the modified Mayo score by ≥30% and ≥2 points, with either a decrease from baseline in the rectal bleeding subscore ≥1 or a rectal bleeding subscore of 0 or 1.
ß Histologic-endoscopic mucosal improvement was defined as combined endoscopic improvement (Mayo endoscopy subscore of 0 or 1) and histologic improvement of the colon tissue (neutrophil infiltration in <5% of crypts, no crypt destruction, and no erosions, ulcerations, or granulation tissue).
The relationship of histologic-endoscopic mucosal improvement, as defined in UC-1, at Week 8 to disease progression and long-term outcomes was not evaluated during UC-1.
Rectal Bleeding and Stool Frequency Subscores
Decreases in rectal bleeding and stool frequency subscores were observed as early as Week 2 in STELARA-treated patients.
Study UC-2
The maintenance study (UC-2) evaluated 523 patients who achieved clinical response 8 weeks following the intravenous administration of either induction dose of STELARA in UC-1. These patients were randomized to receive a subcutaneous maintenance regimen of either 90 mg STELARA every 8 weeks, or every 12 weeks (a lower dose than recommended), or placebo for 44 weeks.
The primary endpoint was the proportion of patients in clinical remission at Week 44. The secondary endpoints included the proportion of patients maintaining clinical response at Week 44, the proportion of patients with endoscopic improvement at Week 44, the proportion of patients with corticosteroid-free clinical remission at Week 44, and the proportion of patients maintaining clinical remission at Week 44 among patients who achieved clinical remission 8 weeks after induction.
Results of the primary and secondary endpoints at Week 44 in patients treated with STELARA at the recommended dosage (90 mg every 8 weeks) compared to the placebo are shown in Table 16.
Table 16. Efficacy Endpoints of Maintenance at Week 44 in UC-2 (52 Weeks from Initiation of the Induction Dose):
| Endpoint | Placebo* N=175† | 90 mg STELARA every 8 weeks N=176 | Treatment difference and 95% CI | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Clinical Remission‡ | 46 | 26% | 79 | 45% | 19% (9%, 28%)§ |
| Bio-naïve¶ | 30/84 | 36% | 39/79 | 49% | |
| Prior biologic failure | 16/88 | 18% | 37/91 | 41% | |
| Maintenance of Clinical Response at Week 44† | 84 | 48% | 130 | 74% | 26% (16%, 36%)§ |
| Bio-naïve¶ | 49/84 | 58% | 62/79 | 78% | |
| Prior biologic failure | 35/88 | 40% | 64/91 | 70% | |
| Endoscopic Improvement# | 47 | 27% | 83 | 47% | 20% (11%, 30%)§ |
| Bio-naïve¶ | 29/84 | 35% | 42/79 | 53% | |
| Prior biologic failure | 18/88 | 20% | 38/91 | 42% | |
| Corticosteroid-free Clinical RemissionÞ | 45 | 26% | 76 | 43% | 17% (8%, 27%)§ |
| Bio-naïve¶ | 30/84 | 36% | 38/79 | 48% | |
| Prior biologic failure | 15/88 | 17% | 35/91 | 38% | |
| Maintenance of Clinical Remission at Week 44 in patients who achieved clinical remission 8 weeks after induction | 18/50 | 36% | 27/41 | 66% | 31% (12%, 50%)ß |
| Bio-naïve¶ | 12/27 | 44% | 14/20 | 70% | |
| Prior biologic failure | 6/23 | 26% | 12/18 | 67% | |
* The placebo group consisted of patients who were in response to STELARA and were randomized to receive placebo at the start of maintenance therapy.
† Clinical response was defined as a decrease from baseline in the modified Mayo score by ≥30% and ≥2 points, with either a decrease from baseline in the rectal bleeding subscore ≥1 or a rectal bleeding subscore of 0 or 1.
‡ Clinical remission was defined as Mayo stool frequency subscore of 0 or 1, Mayo rectal bleeding subscore of 0, and Mayo endoscopy subscore of 0 or 1 (modified so that 1 does not include friability).
§ p= <0.001
¶ An additional 3 patients on placebo and 6 patients on STELARA had been exposed to, but had not failed, biologics.
# Endoscopic improvement was defined as Mayo endoscopy subscore of 0 or 1 (modified so that 1 does not include friability).
Þ Corticosteroid-free clinical remission was defined as patients in clinical remission and not receiving corticosteroids at Week 44.
ß p=0.004
Other Endpoints
Week 16 Responders to Ustekinumab Induction
Patients who were not in clinical response 8 weeks after induction with STELARA in UC-1 were not included in the primary efficacy analyses for Study UC-2; however, these patients were eligible to receive a 90 mg subcutaneous injection of STELARA at Week 8. Of these patients, 55/101 (54%) achieved clinical response eight weeks later (Week 16) and received STELARA 90 mg subcutaneously every 8 weeks during the UC-2 trial. At Week 44, there were 97/157 (62%) patients who maintained clinical response and there were 51/157 (32%) who achieved clinical remission.
Histologic-Endoscopic Mucosal Improvement at Week 44
The proportion of patients achieving histologic-endoscopic mucosal improvement during maintenance treatment in UC-2 was 75/172 (44%) among patients on STELARA and 40/172 (23%) in patients on placebo at Week 44. The relationship of histologic-endoscopic mucosal improvement, as defined in UC-2, at Week 44 to progression of disease or long-term outcomes was not evaluated in UC-2.
Endoscopic Normalization
Normalization of endoscopic appearance of the mucosa was defined as a Mayo endoscopic subscore of 0. At Week 8 in UC-1, endoscopic normalization was achieved in 25/322 (8%) of patients treated with STELARA and 12/319 (4%) of patients in the placebo group. At Week 44 of UC-2, endoscopic normalization was achieved in 51/176 (29%) of patients treated with STELARA and in 32/175 (18%) of patients in placebo group.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.