STOCRIN Film-coated tablet Ref.[2777] Active ingredients: Efavirenz
Source: European Medicines Agency (EU) Revision Year: 2023 Publisher: Merck Sharp & Dohme B.V., Waarderweg 39, 2031 BN Haarlem, The Netherlands
Contraindications
Hypersensitivity to the active substance or to any of the excipients listed in section 6.1.
Patients with severe hepatic impairment (Child Pugh Class C) (see section 5.2).
Co-administration with terfenadine, astemizole, cisapride, midazolam, triazolam, pimozide, bepridil, or ergot alkaloids (for example, ergotamine, dihydroergotamine, ergonovine, and methylergonovine) because competition for CYP3A4 by efavirenz could result in inhibition of metabolism and create the potential for serious and/or life-threatening adverse reactions [for example, cardiac arrhythmias, prolonged sedation or respiratory depression] (see section 4.5).
Herbal preparations containing St. John’s wort (Hypericum perforatum) due to the risk of decreased plasma concentrations and reduced clinical effects of efavirenz (see section 4.5).
Patients with:
- a family history of sudden death or of congenital prolongation of the QTc interval on electrocardiograms, or with any other clinical condition known to prolong the QTc interval.
- a history of symptomatic cardiac arrythmias or with clinically relevant bradycardia or with congestive cardiac failure accompanied by reduced left ventricle ejection fraction.
- severe disturbances of electrolyte balance e.g., hypokalaemia or hypomagnesaemia.
Patients taking drugs that are known to prolong the QTc interval (proarrhythmic).
These drugs include:
- antiarrhythmics of classes IA and III,
- neuroleptics, antidepressive agents,
- certain antibiotics including some agents of the following classes: macrolides, fluoroquinolones, imidazole and triazole antifungal agents,
- certain non-sedating antihistamines (terfenadine, astemizole),
- cisapride,
- flecainide,
- certain antimalarials,
- methadone.
Co-administration with elbasvir/grazoprevir due to the expected significant decreases in elbasvir and grazoprevir plasma concentrations (see section 4.5). This effect is due to an induction of CYP3A4 or P-gp by efavirenz and is expected to result in the loss of virologic response of elbasvir/grazoprevir.
Special warnings and precautions for use
Efavirenz must not be used as a single agent to treat HIV or added on as a sole agent to a failing regimen. Resistant virus emerges rapidly when efavirenz is administered as monotherapy. The choice of new antiretroviral agent(s) to be used in combination with efavirenz should take into consideration the potential for viral cross-resistance (see section 5.1).
Co-administration of efavirenz with a fixed combination tablet containing efavirenz, emtricitabine, and tenofovir disoproxil, is not recommended unless needed for dose adjustment (for example, with rifampicin).
Co-administration of glecaprevir/pibrentasvir with efavirenz may significantly decrease plasma concentrations of glecaprevir and pibrentasvir, leading to reduced therapeutic effect. Co-administration of glecaprevir/pibrentasvir with efavirenz is not recommended (see section 4.5).
Concomitant use of Ginkgo biloba extracts is not recommended (see section 4.5).
When prescribing medicinal products concomitantly with efavirenz, physicians should refer to the corresponding Summary of Product Characteristics.
While effective viral suppression with antiretroviral therapy has been proven to substantially reduce the risk of sexual transmission, a residual risk cannot be excluded. Precautions to prevent transmission should be taken in accordance with national guidelines.
If any antiretroviral medicinal product in a combination regimen is interrupted because of suspected intolerance, serious consideration should be given to simultaneous discontinuation of all antiretroviral medicinal products. The antiretroviral medicinal products should be restarted at the same time upon resolution of the intolerance symptoms. Intermittent monotherapy and sequential reintroduction of antiretroviral agents is not advisable because of the increased potential for selection of resistant virus.
Rash
Mild-to-moderate rash has been reported in clinical studies with efavirenz and usually resolves with continued therapy. Appropriate antihistamines and/or corticosteroids may improve the tolerability and hasten the resolution of rash. Severe rash associated with blistering, moist desquamation or ulceration has been reported in less than 1% of patients treated with efavirenz. The incidence of erythema multiforme or Stevens-Johnson syndrome was approximately 0.1%. Efavirenz must be discontinued in patients developing severe rash associated with blistering, desquamation, mucosal involvement or fever. If therapy with efavirenz is discontinued, consideration should also be given to interrupting therapy with other antiretroviral agents to avoid development of resistant virus (see section 4.8).
Experience with efavirenz in patients who discontinued other antiretroviral agents of the NNRTI class is limited (see section 4.8). Efavirenz is not recommended for patients who have had a life-threatening cutaneous reaction (e.g., Stevens-Johnson syndrome) while taking another NNRTI.
Psychiatric symptoms
Psychiatric adverse reactions have been reported in patients treated with efavirenz. Patients with a prior history of psychiatric disorders appear to be at greater risk of these serious psychiatric adverse reactions. In particular, severe depression was more common in those with a history of depression. There have also been post-marketing reports of severe depression, death by suicide, delusions, psychosis-like behaviour and catatonia. Patients should be advised that if they experience symptoms such as severe depression, psychosis or suicidal ideation, they should contact their doctor immediately to assess the possibility that the symptoms may be related to the use of efavirenz, and if so, to determine whether the risks of continued therapy outweigh the benefits (see section 4.8).
Nervous system symptoms
Symptoms including, but not limited to, dizziness, insomnia, somnolence, impaired concentration and abnormal dreaming are frequently reported adverse reactions in patients receiving efavirenz 600 mg daily in clinical studies (see section 4.8). Nervous system symptoms usually begin during the first one or two days of therapy and generally resolve after the first 2-4 weeks. Patients should be informed that if they do occur, these common symptoms are likely to improve with continued therapy and are not predictive of subsequent onset of any ofthe less frequent psychiatric symptoms.
Late-onset neurotoxicity, including ataxia and encephalopathy (impaired consciousness, confusion, psychomotor slowing, psychosis, delirium), may occur months to years after beginning efavirenz therapy. Some events of late-onset neurotoxicity have occurred in patients with CYP2B6 genetic polymorphisms, which are associated with increased efavirenz levels despite standard dosing of STOCRIN. Patients presenting with signs and symptoms of serious neurologic adverse experiences should be evaluated promptly to assess the possibility that these events may be related to efavirenz use, and whether discontinuation of STOCRIN is warranted.
Seizures
Convulsions have been observed in patients receiving efavirenz, generally in the presence of known medical history of seizures. Patients who are receiving concomitant anticonvulsant medicinal products primarily metabolised by the liver, such as phenytoin, carbamazepine and phenobarbital, may require periodic monitoring of plasma levels. In a drug interaction study, carbamazepine plasma concentrations were decreased when carbamazepine was co-administered with efavirenz (see section 4.5). Caution must be taken in any patient with a history of seizures.
Hepatic events
A few of the postmarketing reports of hepatic failure occurred in patients with no pre-existing hepatic disease or other identifiable risk factors (see section 4.8). Liver enzyme monitoring should be considered for patients without pre-existing hepatic dysfunction or other risk factors.
QTc Prolongation
QTc prolongation has been observed with the use of efavirenz (see sections 4.5 and 5.1).
Consider alternatives to efavirenz for co-administration with a drug with a known risk of Torsade de Pointes or when to be administered to patients at higher risk of Torsade de Pointes.
Effect of food
The administration of efavirenz with food may increase efavirenz exposure (see section 5.2) and may lead to an increase in the frequency of adverse reactions (see section 4.8). It is recommended that efavirenz be taken on an empty stomach, preferably at bedtime.
Immune Reactivation Syndrome
In HIV infected patients with severe immune deficiency at the time of institution of combination antiretroviral therapy (CART), an inflammatory reaction to asymptomatic or residual opportunistic pathogens may arise and cause serious clinical conditions, or aggravation of symptoms. Typically, such reactions have been observed within the first few weeks or months of initiation of CART. Relevant examples are cytomegalovirus retinitis, generalised and/or focal mycobacterial infections, and pneumonia caused by Pneumocystis jiroveci (formerly known as Pneumocystis carinii). Any inflammatory symptoms should be evaluated and treatment instituted when necessary. Autoimmune disorders (such as Graves' disease and autoimmune hepatitis) have also been reported to occur in the setting of immune reactivation; however, the reported time to onset is more variable and these events can occur many months after initiation of treatment.
Weight and metabolic parameters
An increase in weight and in levels of blood lipids and glucose may occur during antiretroviral therapy. Such changes may in part be linked to disease control and life style. For lipids, there is in some cases evidence for a treatment effect, while for weight gain there is no strong evidence relating this to any particular treatment. For monitoring of blood lipids and glucose reference is made to established HIV treatment guidelines. Lipid disorders should be managed as clinically appropriate.
Osteonecrosis
Although the aetiology is considered to be multifactorial (including corticosteroid use, alcohol consumption, severe immunosuppression, higher body mass index), cases of osteonecrosis have been reported particularly in patients with advanced HIV-disease and/or long-term exposure to combination antiretroviral therapy (CART). Patients should be advised to seek medical advice if they experience joint aches and pain, joint stiffness or difficulty in movement.
Special populations
Liver disease
Efavirenz is contraindicated in patients with severe hepatic impairment (see sections 4.3 and 5.2) and not recommended in patients with moderate hepatic impairment because of insufficient data to determine whether dose adjustment is necessary. Because of the extensive cytochrome P450-mediated metabolism of efavirenz and limited clinical experience in patients with chronic liver disease, caution must be exercised in administering efavirenz to patients with mild hepatic impairment. Patients should be monitored carefully for dose-related adverse reactions, especially nervous system symptoms. Laboratory tests should be performed to evaluate their liver disease at periodic intervals (see section 4.2).
The safety and efficacy of efavirenz has not been established in patients with significant underlying liver disorders. Patients with chronic hepatitis B or C and treated with combination antiretroviral therapy are at increased risk for severe and potentially fatal hepatic adverse reactions. Patients with pre-existing liver dysfunction including chronic active hepatitis have an increased frequency of liver function abnormalities during combination antiretroviral therapy and should be monitored according to standard practice. If there is evidence of worsening liver disease or persistent elevations of serum transaminases to greater than 5 times the upper limit of the normal range, the benefit of continued therapy with efavirenz needs to be weighed against the potential risks of significant liver toxicity. In such patients, interruption or discontinuation of treatment must be considered (see section 4.8).
In patients treated with other medicinal products associated with liver toxicity, monitoring of liver enzymes is also recommended. In case of concomitant antiviral therapy for hepatitis B or C, please refer also to the relevant product information for these medicinal products.
Renal insufficiency
The pharmacokinetics of efavirenz have not been studied in patients with renal insufficiency; however, less than 1% of an efavirenz dose is excreted unchanged in the urine, so the impact of renal impairment on efavirenz elimination should be minimal (see section 4.2). There is no experience in patients with severe renal failure and close safety monitoring is recommended in this population.
Elderly patients
Insufficient numbers of older patients have been evaluated in clinical studies to determine whether they respond differently than younger patients.
Paediatric population
Efavirenz has not been evaluated in children below 3 years of age or who weigh less than 13 kg. Therefore, efavirenz should not be given to children less than 3 years of age.
Rash was reported in 26 of 57 children (46%) treated with efavirenz during a 48-week period and was severe in three patients. Prophylaxis with appropriate antihistamines prior to initiating therapy with efavirenz in children may be considered.
Lactose
Patients with rare hereditary problems of galactose intolerance, total lactase deficiency or glucose-galactose malabsorption should not take this medicinal product. Individuals with these conditions may take efavirenz oral solution, which is free from lactose.
Sodium
These medicinal products contain less than 1 mmol sodium (23 mg) per film-coated tablet, that is to say essentially ‘sodium free’.
Interaction with other medicinal products and other forms of interaction
Efavirenz is an in vivo inducer of CYP3A4, CYP2B6 and UGT1A1. Compounds that are substrates of these enzymes may have decreased plasma concentrations when co-administered with efavirenz. In vitro efavirenz is also an inhibitor of CYP3A4. Theoretically, efavirenz may therefore initially increase the exposure to CYP3A4 substrates and caution is warranted for CYP3A4 substrates with narrow therapeutic index (see section 4.3). Efavirenz may be an inducer of CYP2C19 and CYP2C9; however inhibition has also been observed in vitro and the net effect of co-administration with substrates of these enzymes is not clear (see section 5.2).
Efavirenz exposure may be increased when given with medicinal products (for example, ritonavir) or food (for example, grapefruit juice), which inhibit CYP3A4 or CYP2B6 activity.
Compounds or herbal preparations (for example Ginkgo biloba extracts and St. John’s wort) which induce these enzymes may give rise to decreased plasma concentrations of efavirenz. Concomitant use of St. John’s wort is contraindicated (see section 4.3). Concomitant use of Ginkgo biloba extracts is not recommended (see section 4.4).
Co-administration of efavirenz with metamizole, which is an inducer of metabolising enzymes including CYP2B6 and CYP3A4, may cause a reduction in plasma concentrations of efavirenz with potential decrease in clinical efficacy. Therefore, caution is advised when metamizole and efavirenz are administered concurrently; clinical response and/or drug levels should be monitored as appropriate.
QT Prolonging Drugs
Efavirenz is contraindicated with concomitant use of drugs (they may cause prolonged QTc interval and Torsade de Pointes) such as: antiarrhythmics of classes IA and III, neuroleptics and antidepressant agents, certain antibiotics including some agents of the following classes: macrolides, fluoroquinolones, imidazole, and triazole antifungal agents, certain non-sedating antihistaminics (terfenadine, astemizole), cisapride, flecainide, certain antimalarials and methadone (see section 4.3).
Paediatric population
Interaction studies have only been performed in adults.
Contraindications of concomitant use
Efavirenz must not be administered concurrently with terfenadine, astemizole, cisapride, midazolam, triazolam, pimozide, bepridil, or ergot alkaloids (for example, ergotamine, dihydroergotamine, ergonovine, and methylergonovine) since inhibition of their metabolism may lead to serious, life-threatening events (see section 4.3).
Efavirenz must not be administered with elbasvir/grazoprevir due to the expected significant decreases in elbasvir and grazoprevir plasma concentrations caused by induction of drug metabolising enzymes and/or transport proteins and which are expected to result in the loss of virologic response of elbasvir/grazoprevir (see section 4.5).
St. John’s wort (Hypericum perforatum)
Co-administration of efavirenz and St. John’s wort or herbal preparations containing St. John’s wort is contraindicated. Plasma levels of efavirenz can be reduced by concomitant use of St. John’s wort due to induction ofdrug metabolising enzymes and/or transport proteins by St. John’s wort. Ifa patient is already taking St. John’s wort, stop St. John’s wort, check viral levels and if possible efavirenz levels. Efavirenz levels may increase on stopping St. John’s wort and the dose of efavirenz may need adjusting. The inducing effect of St. John’s wort may persist for at least 2 weeks after cessation of treatment (see section 4.3).
Praziquantel
Concomitant use with praziquantel is not recommended due to significant decrease in plasma concentrations of praziquantel, with risk of treatment failure due to increased hepatic metabolism by efavirenz. In case the combination is needed, an increased dose of praziquantel could be considered.
Other interactions
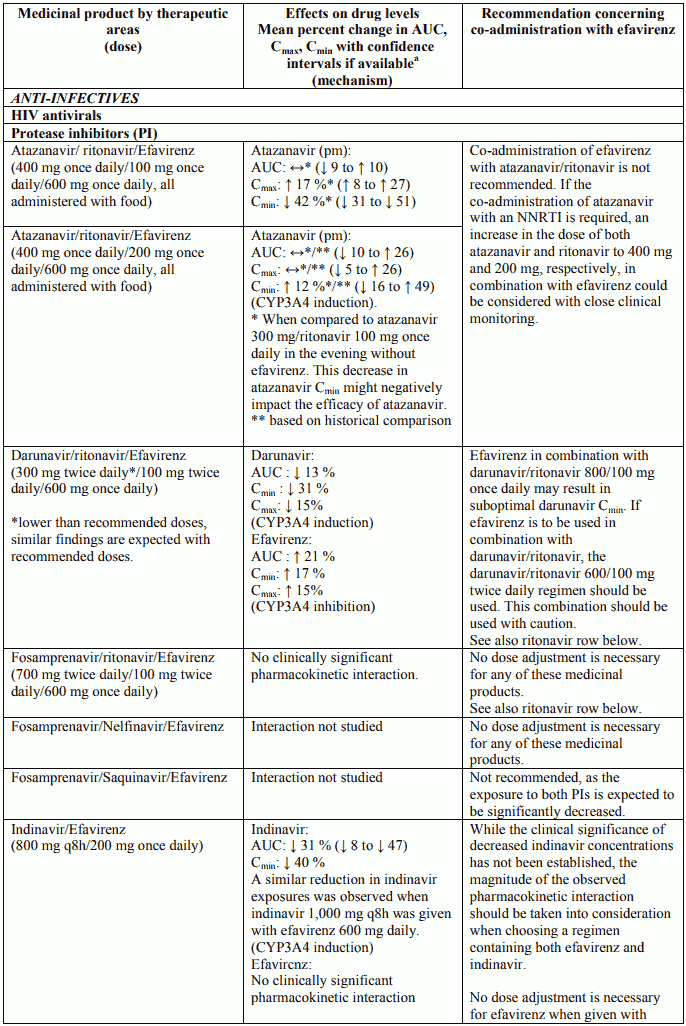
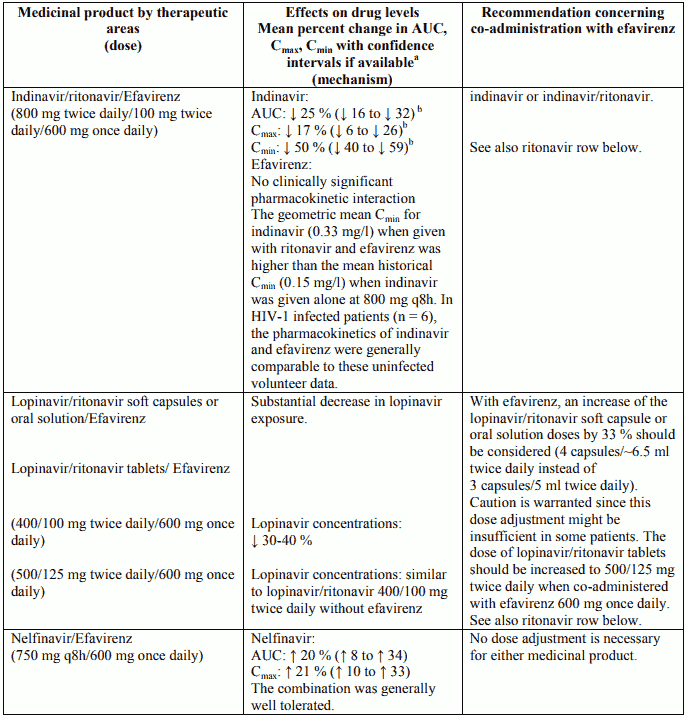
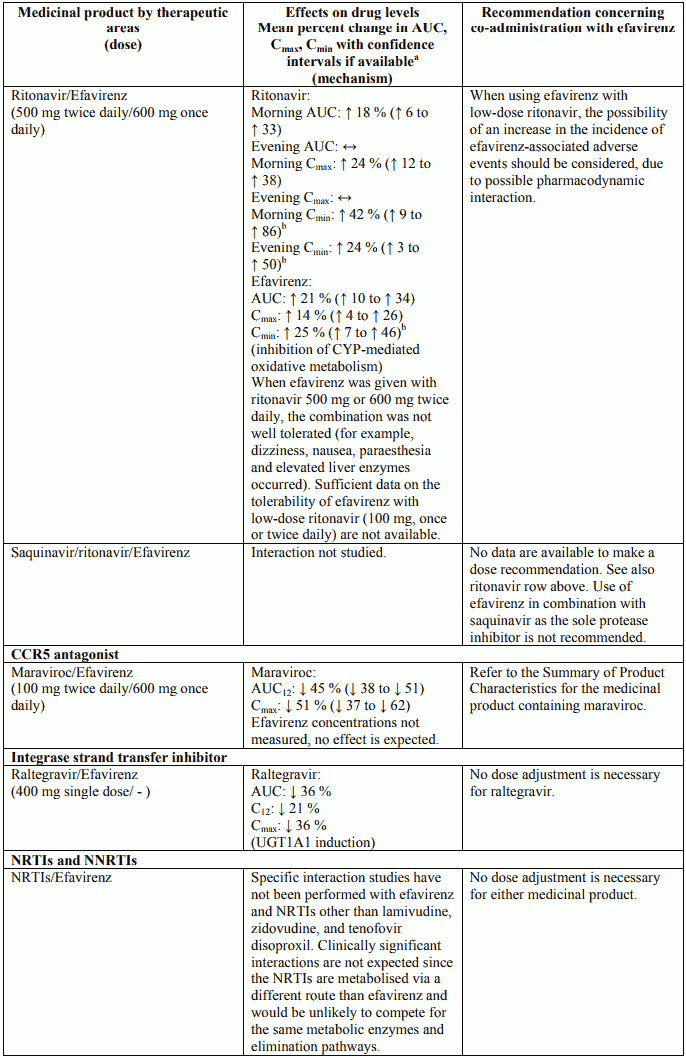
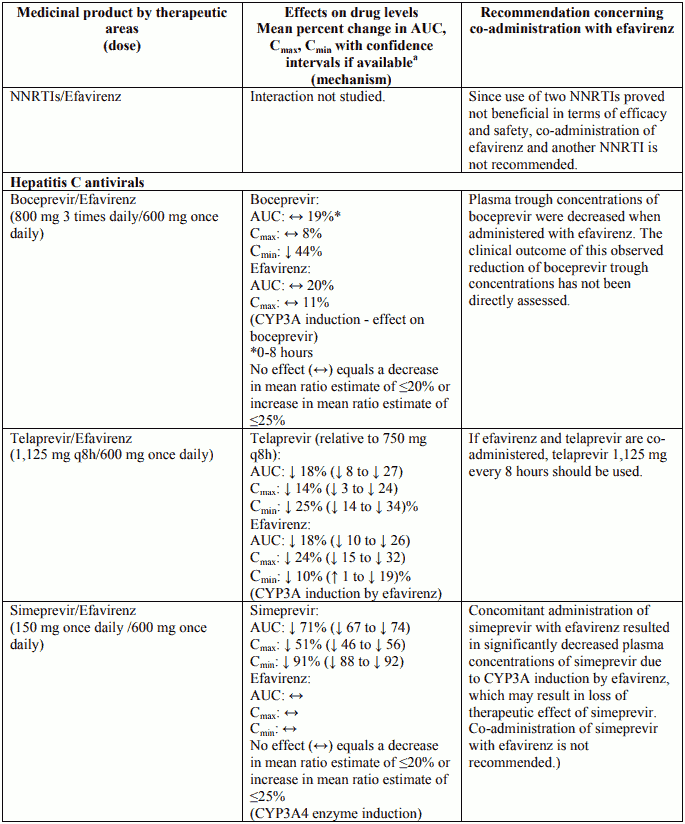
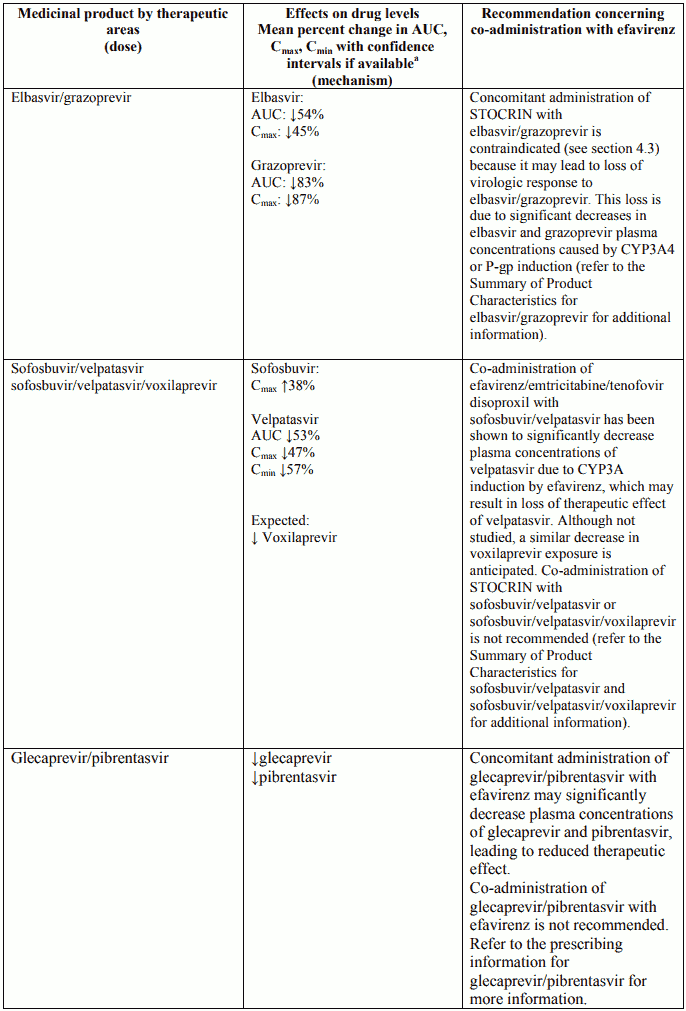
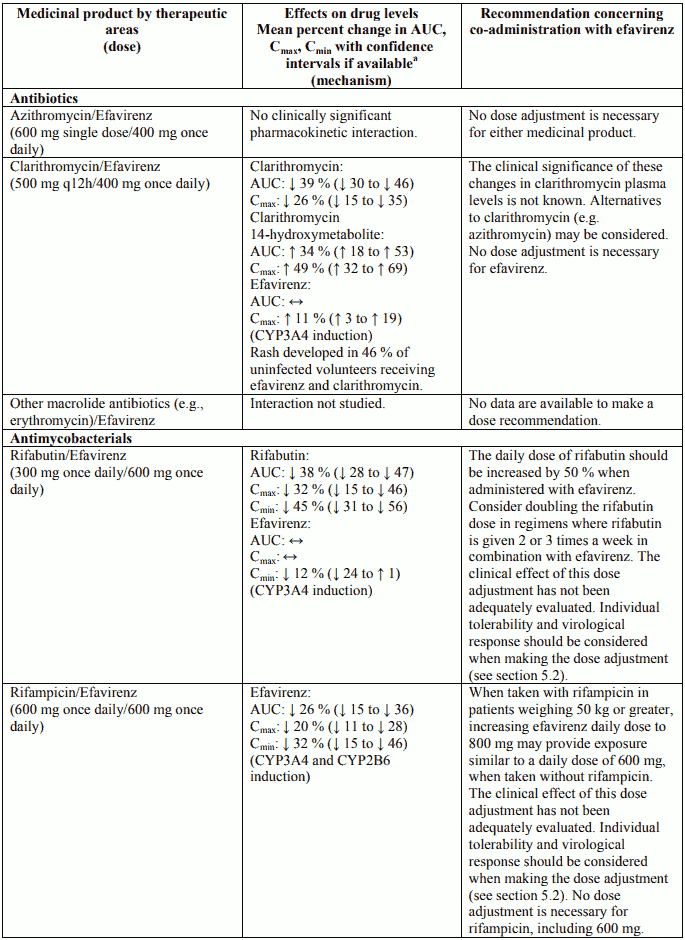
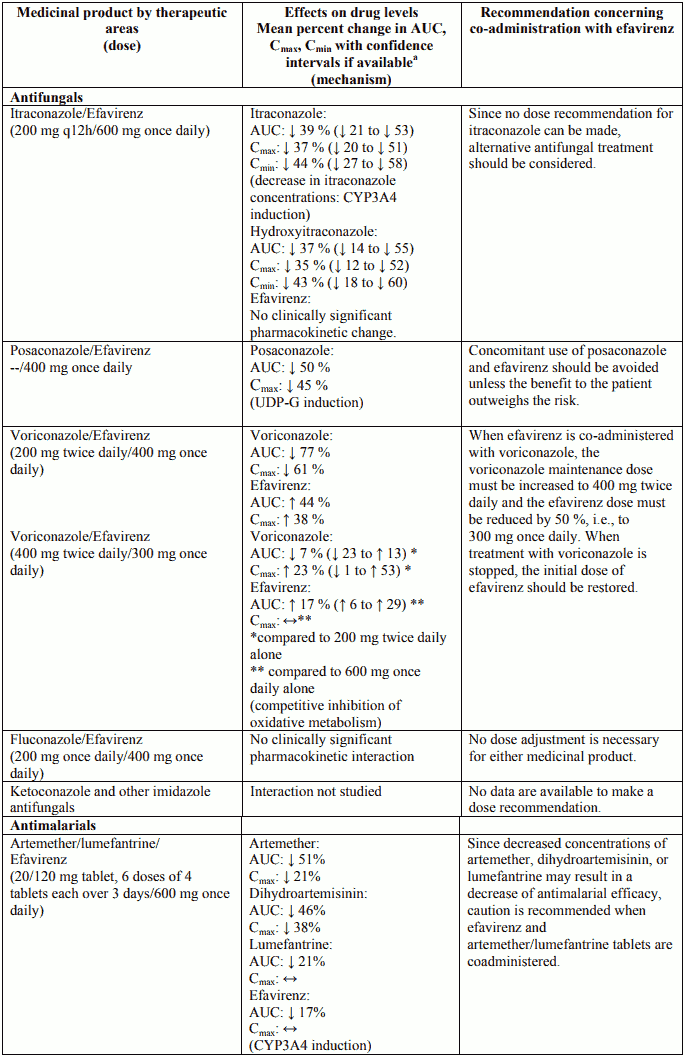
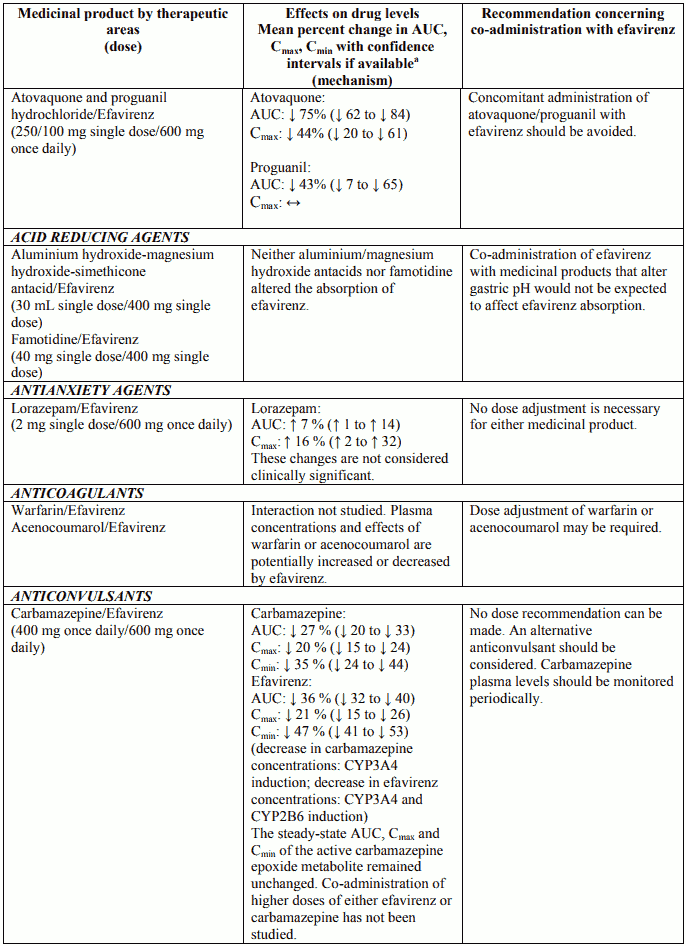
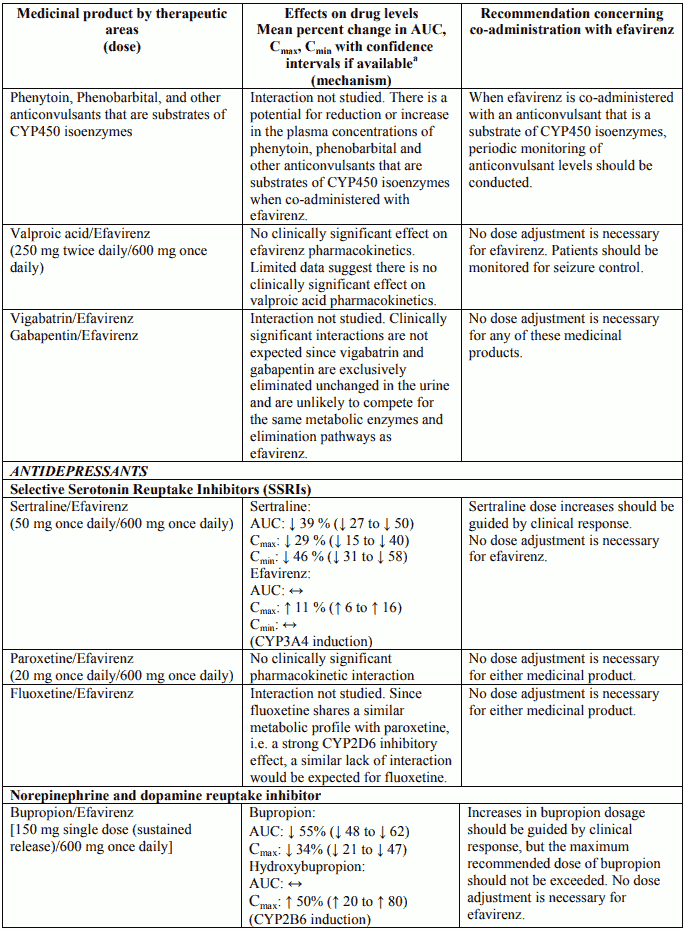
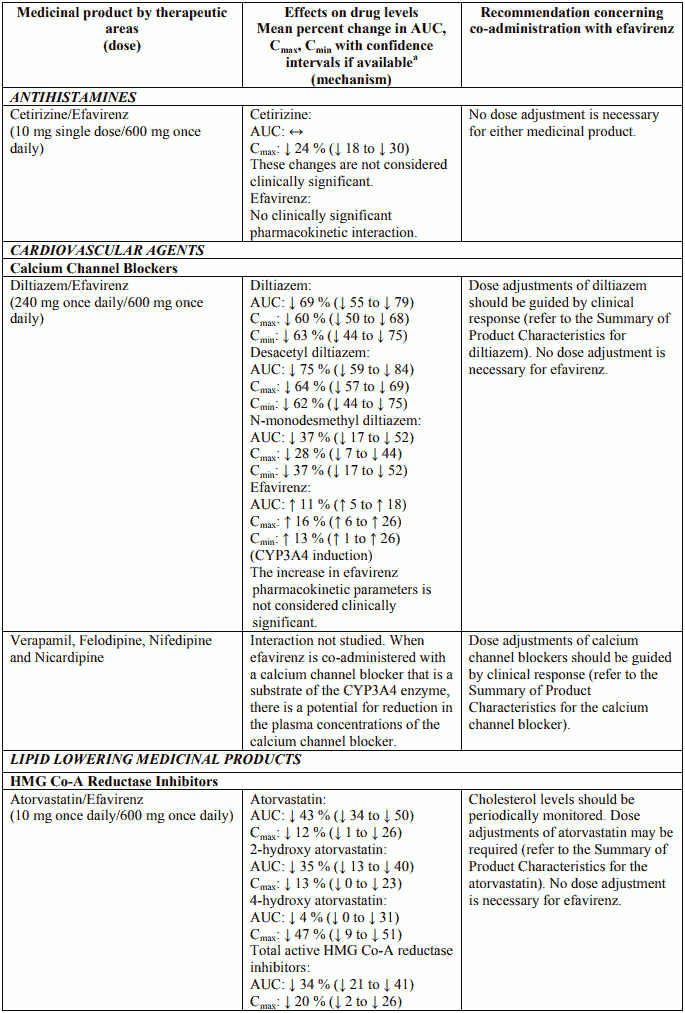
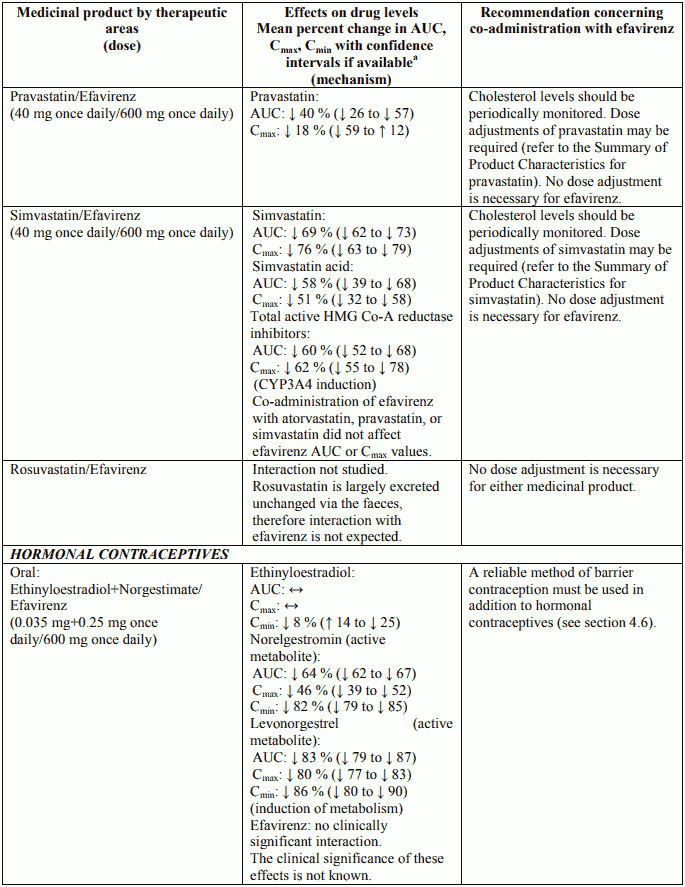
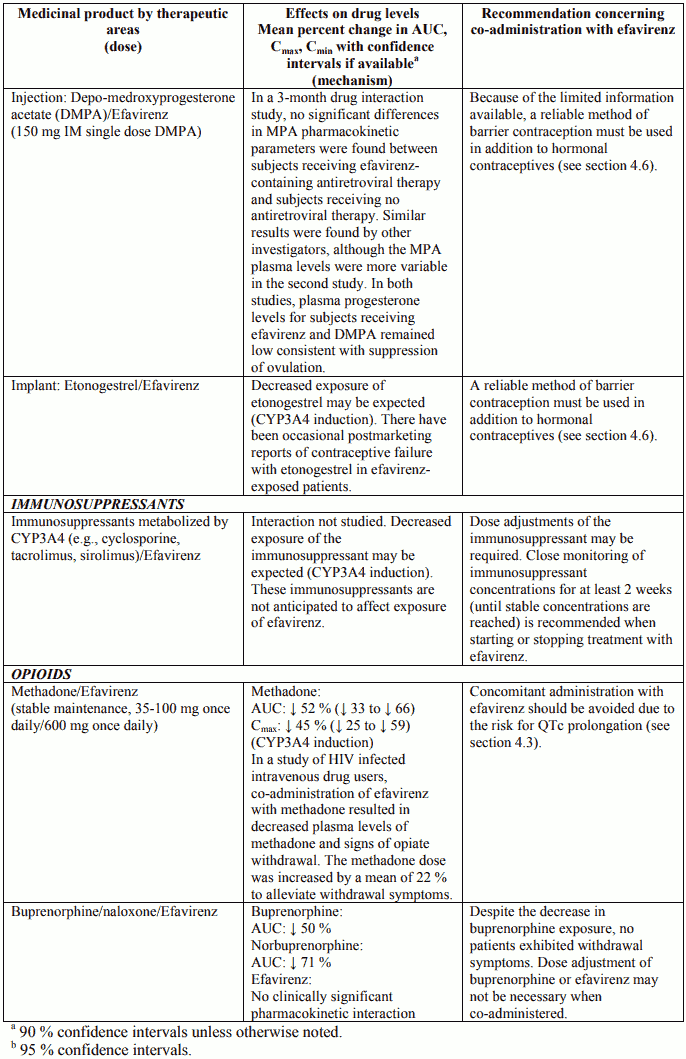
Interactions between efavirenz and protease inhibitors, antiretroviral agents other than protease inhibitors and other non-antiretroviral medicinal products are listed in Table 2 below (increase is indicated as “↑”, decrease as “↓”, no change as “↔”, and once every 8 or 12 hours as “q8h” or “q12h”). If available, 90% or 95% confidence intervals are shown in parentheses. Studies were conducted in healthy subjects unless otherwise noted.
Table 2. Interactions between efavirenz and other medicinal products in adults:
Other interactions
Efavirenz does not bind to cannabinoid receptors. False-positive urine cannabinoid test results have been reported with some screening assays in uninfected and HIV-infected subjects receiving efavirenz. Confirmatory testing by a more specific method such as gas chromatography/mass spectrometry is recommended in such cases.
Fertility, pregnancy and breast-feeding
Contraception in males and females
Barrier contraception should always be used in combination with other methods of contraception (for example, oral or other hormonal contraceptives, see section 4.5). Because of the long half-life of efavirenz, use of adequate contraceptive measures for 12 weeks after discontinuation of efavirenz is recommended.
Pregnancy
Efavirenz should not be used during pregnancy, unless the patient’s clinical condition requires such treatment. Women of childbearing potential should undergo pregnancy testing before initiation of efavirenz (see section 5.3).
There have been seven retrospective reports of findings consistent with neural tube defects, including meningomyelocele, all in mothers exposed to efavirenz-containing regimens (excluding any efavirenz-containing fixed-dose combination tablets) in the first trimester. Two additional cases (1 prospective and 1 retrospective) including events consistent with neural tube defects have been reported with a fixed-dose combination tablet containing efavirenz, emtricitabine, and tenofovir disoproxil. A causal relationship of these events to the use of efavirenz has not been established, and the denominator is unknown. As neural tube defects occur within the first 4 weeks of foetal development (at which time neural tubes are sealed), this potential risk would concern women exposed to efavirenz during the first trimester of pregnancy.
As of July 2013, the Antiretroviral Pregnancy Registry (APR) has received prospective reports of 904 pregnancies with first trimester exposure to efavirenz-containing regimens, resulting in 766 live births. One child was reported to have a neural tube defect, and the frequency and pattern of other birth defects were similar to those seen in children exposed to non-efavirenz-containing regimens, as well as those in HIV negative controls. The incidence of neural tube defects in the general population ranges from 0.5-1 case per 1,000 live births.
Malformations have been observed in foetuses from efavirenz-treated monkeys (see section 5.3).
Breast-feeding
Efavirenz has been shown to be excreted in human milk. There is insufficient information on the effects of efavirenz in newborns/infants. Risk to the infant can not be excluded. Breast-feeding should be discontinued during treatment with efavirenz. It is recommended that HIV infected women do not breast-feed their infants under any circumstances in order to avoid transmission of HIV.
Fertility
The effect of efavirenz on male and female fertility in rats has only been evaluated at doses that achieved systemic drug exposures equivalent to or below those achieved in humans given recommended doses of efavirenz. In these studies, efavirenz did not impair mating or fertility of male or female rats (doses up to 100 mg/kg/bid), and did not affect sperm or offspring of treated male rats (doses up to 200 mg/bid). The reproductive performance of offspring born to female rats given efavirenz was not affected.
Effects on ability to drive and use machines
Efavirenz may cause dizziness, impaired concentration, and/or somnolence. Patients should be instructed that if they experience these symptoms they should avoid potentially hazardous tasks such as driving or operating machinery.
Undesirable effects
Summary of the safety profile
Efavirenz has been studied in over 9,000 patients. In a subset of 1,008 adult patients who received 600 mg efavirenz daily in combination with PIs and/or NRTIs in controlled clinical studies, the most frequently reported adverse reactions of at least moderate severity reported in at least 5% of patients were rash (11.6%), dizziness (8.5%), nausea (8.0%), headache (5.7%) and fatigue (5.5%). The most notable adverse reactions associated with efavirenz are rash and nervous system symptoms. Nervous system symptoms usually begin soon after therapy onset and generally resolve after the first 2-4 weeks. Severe skin reactions such as Stevens-Johnson syndrome and erythema multiforme; psychiatric adverse reactions including severe depression, death by suicide, and psychosis like behaviour; and seizures have been reported in patients treated with efavirenz. The administration of efavirenz with food may increase efavirenz exposure and may lead to an increase in the frequency of adverse reactions (see section 4.4).
The long-term safety profile of efavirenz-containing regimens was evaluated in a controlled trial (006) in which patients received efavirenz + zidovudine + lamivudine (n=412, median duration 180 weeks), efavirenz + indinavir (n=415, median duration 102 weeks), or indinavir + zidovudine + lamivudine (n=401, median duration 76 weeks). Long-term use of efavirenz in this study was not associated with any new safety concerns.
Tabulated list of adverse reactions
Adverse reactions of moderate or greater severity with at least possible relationship to treatment regimen (based on investigator attribution) reported in clinical trials of efavirenz at the recommended dose in combination therapy (n=1,008) are listed below. Also listed in italics are adverse reactions observed post-marketing in association with efavirenz-containing antiretroviral treatment regimens. Frequency is defined using the following convention: very common (≥1/10); common (≥1/100 to <1/10); uncommon (≥1/1,000 to <1/100); rare (≥1/10,000 to <1/1,000); or very rare (<1/10,000).
| Immune system disorders | |
| uncommon | hypersensitivity |
| Metabolism and nutrition disorders | |
| common | hypertriglyceridaemia* |
| uncommon | hypercholesterolaemia* |
| Psychiatric disorders | |
| common | abnormal dreams, anxiety, depression, insomnia* |
| uncommon | affect lability, aggression, confusional state, euphoric mood, hallucination, mania, paranoia, psychosis‡, suicide attempt, suicide ideation, catatonia* |
| rare | delusion‡‡, neurosis‡‡, completed suicide‡‡* |
| Nervous system disorders | |
| common | cerebellar coordination and balance disturbances‡ , disturbance in attention (3.6%), dizziness (8.5%), headache (5.7%), somnolence (2.0%)* |
| uncommon | agitation, amnesia, ataxia, coordination abnormal, convulsions, thinking abnormal, tremor‡ |
| not known | encephalopathy |
| Eye disorders | |
| uncommon | vision blurred |
| Ear and labyrinth disorders | |
| uncommon | tinnitus‡, vertigo |
| Vascular disorders | |
| uncommon | flushing‡ |
| Gastrointestinal disorders | |
| common | abdominal pain, diarrhoea, nausea, vomiting |
| uncommon | pancreatitis |
| Hepatobiliary disorders | |
| common | aspartate aminotransferase (AST) increased*, alanine aminotransferase (ALT) increased*, gamma-glutamyltransferase (GGT) increased* |
| uncommon | hepatitis acute |
| rare | hepatic failure‡‡* |
| Skin and subcutaneous tissue disorders | |
| very common | rash (11.6%)* |
| common | pruritus |
| uncommon | erythema multiforme, Stevens-Johnson syndrome* |
| rare | photoallergic dermatitis‡ |
| Reproductive system and breast disorders | |
| uncommon | gynaecomastia |
| General disorders and administration site conditions | |
| common | fatigue |
*,‡,‡‡ See section Description of selected adverse reactions for more details.
Description of selected adverse reactions
Information regarding post-marketing surveillance
‡ These adverse reactions were identified through post-marketing surveillance; however, the frequencies were determined using data from 16 clinical trials (n=3,969).
‡‡ These adverse reactions were identified through post-marketing surveillance but not reported as drug-related events for efavirenz-treated patients in 16 clinical trials. The frequency category of “rare” was defined per A Guideline on Summary of Product Characteristics (SmPC) (rev. 2, Sept 2009) on the basis ofan estimated upper bound of the 95% confidence interval for 0 events given the number of patients treated with efavirenz in these clinical trials (n=3,969).
Rash
In clinical studies, 26% of patients treated with 600 mg of efavirenz experienced skin rash compared with 17% of patients treated in control groups. Skin rash was considered treatment related in 18% of patients treated with efavirenz. Severe rash occurred in less than 1% of patients treated with efavirenz, and 1.7% discontinued therapy because of rash. The incidence of erythema multiforme or Stevens-Johnson syndrome was approximately 0.1%.
Rashes are usually mild-to-moderate maculopapular skin eruptions that occur within the first two weeks of initiating therapy with efavirenz. In most patients rash resolves with continuing therapy with efavirenz within one month. Efavirenz can be reinitiated in patients interrupting therapy because of rash. Use of appropriate antihistamines and/or corticosteroids is recommended when efavirenz is restarted.
Experience with efavirenz in patients who discontinued other antiretroviral agents of the NNRTI class is limited. Reported rates of recurrent rash following a switch from nevirapine to efavirenz therapy, primarily based on retrospective cohort data from published literature, range from 13 to 18%, comparable to the rate observed in patients treated with efavirenz in clinical studies. (See section 4.4.)
Psychiatric symptoms
Serious psychiatric adverse reactions have been reported in patients treated with efavirenz. In controlled trials the frequency of specific serious psychiatric events were:
| Efavirenz regimen (n=1,008) | Control regimen (n=635) | |
|---|---|---|
| Severe depression | 1.6% | 0.6% |
| Suicidal ideation | 0.6% | 0.3% |
| Non-fatal suicide attempts | 0.4% | 0% |
| Aggressive behaviour | 0.4% | 0.3% |
| Paranoid reactions | 0.4% | 0.3% |
| Manic reactions | 0.1% | 0% |
Patients with a history of psychiatric disorders appear to be at greater risk of these serious psychiatric adverse reactions with frequencies of each of the above events ranging from 0.3% for manic reactions to 2.0% for both severe depression and suicidal ideation. There have also been post-marketing reports of death by suicide, delusions, psychosis-like behaviour and catatonia.
Nervous system symptoms
In clinical controlled trials, frequently reported adverse reactions included, but were not limited to: dizziness, insomnia, somnolence, impaired concentration and abnormal dreaming. Nervous system symptoms of moderate-to-severe intensity were experienced by 19% (severe 2.0%) of patients compared to 9% (severe 1%) of patients receiving control regimens. In clinical studies 2% of patients treated with efavirenz discontinued therapy due to such symptoms.
Nervous system symptoms usually begin during the first one or two days of therapy and generally resolve after the first 2-4 weeks. In a study of uninfected volunteers, a representative nervous system symptom had a median time to onset of 1 hour post-dose and a median duration of 3 hours. Nervous system symptoms may occur more frequently when efavirenz is taken concomitantly with meals possibly due to increased efavirenz plasma levels (see section 5.2). Dosing at bedtime seems to improve the tolerability of these symptoms and can be recommended during the first weeks of therapy and in patients who continue to experience these symptoms (see section 4.2). Dose reduction or splitting the daily dose has not been shown to provide benefit.
Analysis of long-term data showed that, beyond 24 weeks of therapy, the incidences of new-onset nervous system symptoms among efavirenz-treated patients were generally similar to those in the control arm.
Ataxia and encephalopathy associated with high levels of efavirenz, occurring months to years after beginning efavirenz therapy have been reported post-marketing (see section 4.4).
Hepatic failure
A few of the post-marketing reports of hepatic failure, including cases in patients with no pre-existing hepatic disease or other identifiable risk factors, were characterised by a fulminant course, progressing in some cases to transplantation or death.
Immune Reactivation Syndrome
In HIV infected patients with severe immune deficiency at the time of initiation of combination antiretroviral therapy (CART), an inflammatory reaction to asymptomatic or residual opportunistic infections may arise. Autoimmune disorders (such as Graves' disease and autoimmune hepatitis) have also been reported; however, the reported time to onset is more variable and these events can occur many months after initiation oftreatment (see section 4.4).
Osteonecrosis
Cases of osteonecrosis have been reported, particularly in patients with generally acknowledged risk factors, advanced HIV disease or long-term exposure to combination antiretroviral therapy (CART). The frequency of this is unknown (see section 4.4).
Laboratory test abnormalities
Liver enzymes
Elevations of AST and ALT to greater than five times the upper limit of the normal range (ULN) were seen in 3% of 1,008 patients treated with 600 mg of efavirenz (5-8% after long-term treatment in study 006). Similar elevations were seen in patients treated with control regimens (5% after long-term treatment). Elevations of GGT to greater than five times ULN were observed in 4% of all patients treated with 600 mg of efavirenz and 1.5%-2% of patients treated with control regimens (7% of efavirenz-treated patients and 3% of control-treated patients after long-term treatment). Isolated elevations of GGT in patients receiving efavirenz may reflect enzyme induction. In the long-term study (006), 1% of patients in each treatment arm discontinued because of liver or biliary system disorders.
Amylase
In the clinical trial subset of 1,008 patients, asymptomatic increases in serum amylase levels greater than 1.5 times the upper limit of normal were seen in 10% of patients treated with efavirenz and 6% of patients treated with control regimens. The clinical significance of asymptomatic increases in serum amylase is unknown.
Metabolic parameters
Weight and levels of blood lipids and glucose may increase during antiretroviral therapy (see section 4.4).
Paediatric population
Undesirable effects in children were generally similar to those of adult patients. Rash was reported more frequently in children (in a clinical study including 57 children who received efavirenz during a 48-week period, rash was reported in 46%) and was more often of higher grade than in adults (severe rash was reported in 5.3% of children). Prophylaxis with appropriate antihistamines prior to initiating therapy with efavirenz in children may be considered. Although nervous system symptoms are difficult for young children to report, they appear to be less frequent in children and were generally mild. In the study of 57 children, 3.5% of patients experienced nervous system symptoms of moderate intensity, predominantly dizziness. No child had severe symptoms or had to discontinue because of nervous system symptoms.
Other special populations
Liver enzymes in hepatitis B or C co-infected patients
In the long-term data set from study 006, 137 patients treated with efavirenz-containing regimens (median duration of therapy, 68 weeks) and 84 treated with a control regimen (median duration, 56 weeks) were seropositive at screening for hepatitis B (surface antigen positive) and/or C (hepatitis C antibody positive). Among co-infected patients in study 006, elevations in AST to greater than five times ULN developed in 13% of efavirenz treated patients and in 7% of controls, and elevations in ALT to greater than five times ULN developed in 20% and 7% respectively. Among co-infected patients, 3% of those treated with efavirenz and 2% in the control arm discontinued because of liver disorders (see section 4.4).
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the national reporting system listed in Appendix V.
Incompatibilities
Not applicable.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.