TASIGNA 50/200mg Hard capsule Ref.[9048] Active ingredients: Nilotinib
Source: European Medicines Agency (EU) Revision Year: 2020 Publisher: Novartis Europharm Limited, Vista Building, Elm Park, Merrion Road, Dublin 4, Ireland
Pharmacodynamic properties
Pharmacotherapeutic group: Antineoplastic agents, protein kinase inhibitors
ATC code: L01XE08
Mechanism of action
Nilotinib is a potent inhibitor of the ABL tyrosine kinase activity of the BCR-ABL oncoprotein both in cell lines and in primary Philadelphia-chromosome positive leukaemia cells. The substance binds with high affinity to the ATP-binding site in such a manner that it is a potent inhibitor of wild-type BCR-ABL and maintains activity against 32/33 imatinib-resistant mutant forms of BCR-ABL. As a consequence of this biochemical activity, nilotinib selectively inhibits the proliferation and induces apoptosis in cell lines and in primary Philadelphia-chromosome positive leukaemia cells from CML patients. In murine models of CML, as a single agent nilotinib reduces tumour burden and prolongs survival following oral administration.
Pharmacodynamic effects
Nilotinib has little or no effect against the majority of other protein kinases examined, including Src, except for the PDGF, KIT and Ephrin receptor kinases, which it inhibits at concentrations within the range achieved following oral administration at therapeutic doses recommended for the treatment of CML (see Table 6).
Table 6. Kinase profile of nilotinib (phosphorylation IC50 nM):
| BCR-ABL | PDGFR | KIT |
| 20 | 69 | 210 |
Clinical efficacy
Clinical studies in newly diagnosed CML in chronic phase
An open-label, multicentre, randomised Phase III study was conducted to determine the efficacy of nilotinib versus imatinib in 846 adult patients with cytogenetically confirmed newly diagnosed Philadelphia chromosome positive CML in the chronic phase. Patients were within six months of diagnosis and were previously untreated, with the exception of hydroxyurea and/or anagrelide. Patients were randomised 1:1:1 to receive either nilotinib 300 mg twice daily (n=282), nilotinib 400 mg twice daily (n=281) or imatinib 400 mg once daily (n=283). Randomisation was stratified by Sokal risk score at the time of diagnosis.
Baseline characteristics were well balanced between the three treatment arms. Median age was 47 years in both nilotinib arms and 46 years in the imatinib arm, with 12.8%, 10.0% and 12.4% of patients were ≥65 years of age in the nilotinib 300 mg twice daily, nilotinib 400 mg twice daily and imatinib 400 mg once daily treatment arms, respectively. There were slightly more male than female patients (56.0%, 62.3% and 55.8%, in the nilotinib 300 mg twice daily, 400 mg twice daily and imatinib 400 mg once daily arm, respectively). More than 60% of all patients were Caucasian and 25% of all patients were Asian.
The primary data analysis time point was when all 846 patients completed 12 months of treatment (or discontinued earlier). Subsequent analyses reflect when patients completed 24, 36, 48, 60 and 72 months of treatment (or discontinued earlier). The median time on treatment was approximately 70 months in the nilotinib treatment groups and 64 months in the imatinib group. The median actual dose intensity was 593 mg/day for nilotinib 300 mg twice daily, 772 mg/day for nilotinib 400 mg twice daily and 400 mg/day for imatinib 400 mg once daily. This study is ongoing.
The primary efficacy endpoint was major molecular response (MMR) at 12 months. MMR was defined as ≤0.1% BCR-ABL/ABL% by international scale (IS) measured by RQ-PCR, which corresponds to a ≥3 log reduction of BCR-ABL transcript from standardised baseline. The MMR rate at 12 months was statistically significantly higher for nilotinib 300 mg twice daily compared to imatinib 400 mg once daily (44.3% versus 22.3%, p<0.0001). The rate of MMR at 12 months, was also statistically significantly higher for nilotinib 400 mg twice daily compared to imatinib 400 mg once daily (42.7% versus 22.3%, p<0.0001).
The rates of MMR at 3, 6, 9 and 12 months were 8.9%, 33.0%, 43.3% and 44.3% for nilotinib 300 mg twice daily, 5.0%, 29.5%, 38.1% and 42.7% for nilotinib 400 mg twice daily and 0.7%, 12.0%, 18.0% and 22.3% for imatinib 400 mg once daily.
The MMR rate at 12, 24, 36, 48, 60 and 72 months is presented in Table 7.
Table 7. MMR rate:
| Νilotinib 300 mg twice daily n=282 (%) | Νilotinib 400 mg twice daily n=281 (%) | Imatinib 400 mg once daily n=283 (%) | |
|---|---|---|---|
| MMR at 12 months | |||
| Response (95% CI) | 44.31 (38.4: 50.3) | 42.71 (36.8; 48.7) | 22.3 (17.6; 27.6) |
| MMR at 24 months | |||
| Response (95% CI) | 61.71 (55.8; 67.4) | 59.11 (53.1; 64.9) | 37.5 (31.8; 43.4) |
| MMR at 36 months2 | |||
| Response (95% CI) | 58.51 (52.5; 64.3) | 57.31 (51.3; 63.2) | 38.5 (32.8; 44.5) |
| MMR at 48 months3 | |||
| Response (95% CI) | 59.9 (54.0; 65.7) | 55.2 (49.1; 61.1) | 43.8 (38.0; 49.8) |
| MMR at 60 months4 | |||
| Response (95% CI) | 62.8 (56.8; 68.4) | 61.2 (55.2; 66.9) | 49.1 (43.2; 55.1) |
| MMR at 72 months5 | |||
| Response (95% CI) | 52.5 (46.5; 58.4) | 57.7 (51.6; 63.5) | 41.7 (35.9; 47.7) |
1 Cochran-Mantel-Haenszel (CMH) test p-value for response rate (vs. imatinib 400 mg) <0.0001
2 Only patients who were in MMR at a specific time point are included as responders for that time point. A total of 199 (35.2%) of all patients were not evaluable for MMR at 36 months (87 in the nilotinib 300 mg twice daily group and 112 in the imatinib group) due to missing/unevaluable PCR assessments (n=17), atypical transcripts at baseline (n=7), or discontinuation prior to the 36-month time point (n=175).
3 Only patients who were in MMR at a specific time point are included as responders for that time point. A total of 305 (36.1%) of all patients were not evaluable for MMR at 48 months (98 in the nilotinib 300 mg BID group, 88 in the nilotinib 400 mg BID group and 119 in the imatinib group) due to missing/unevaluable PCR assessments (n=18), atypical transcripts at baseline (n=8), or discontinuation prior to the 48-month time point (n=279).
4 Only patients who were in MMR at a specific time point are included as responders for that time point. A total of 322 (38.1%) of all patients were not evaluable for MMR at 60 months (99 in the nilotinib 300 mg twice daily group, 93 in the nilotinib 400 mg twice daily group and 130 in the imatinib group) due to missing/unevaluable PCR assessments (n=9), atypical transcripts at baseline (n=8) or discontinuation prior to the 60-month time point (n=305).
5 Only patients who were in MMR at a specific time point are included as responders for that time point. A total of 395 (46.7%) of all patients were not evaluable for MMR at 72 months (130 in the nilotinib 300 mg twice daily group, 110 in the nilotinib 400 mg twice daily group and 155 in the imatinib group) due to missing/unevaluable PCR assessments (n=25), atypical transcripts at baseline (n=8) or discontinuation prior to the 72-month time point (n=362).
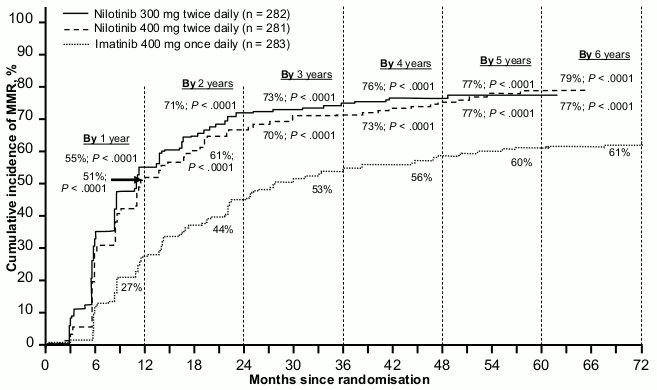
MMR rates by different time points (including patients who achieved MMR at or before those time points as responders) are presented in the cumulative incidence of MMR (see Figure 1).
Figure 1. Cumulative incidence of MMR:
For all Sokal risk groups, the MMR rates at all time points remained consistently higher in the two nilotinib groups than in the imatinib group.
In a retrospective analysis, 91% (234/258) of patients on nilotinib 300 mg twice daily achieved BCR-ABL levels ≤10% at 3 months of treatment compared to 67% (176/264) of patients on imatinib 400 mg once daily. Patients with BCR-ABL levels ≤10% at 3 months of treatment show a greater overall survival at 72 months compared to those who did not achieve this molecular response level (94.5% vs. 77.1% respectively [p=0.0005]).
Based on the Kaplan-Meier analysis of time to first MMR the probability of achieving MMR at different time points was higher for both nilotinib at 300 mg and 400 mg twice daily compared to imatinib 400 mg once daily (HR=2.17 and stratified log-rank p<0.0001 between nilotinib 300 mg twice daily and imatinib 400 mg once daily, HR=1.88 and stratified log-rank p<0.0001 between nilotinib 400 mg twice daily and imatinib 400 mg once daily).
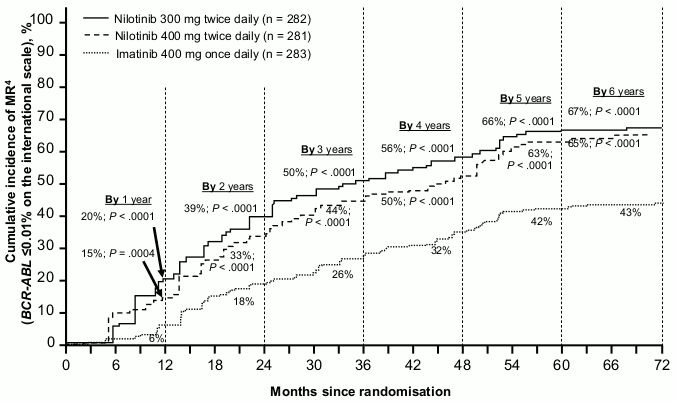
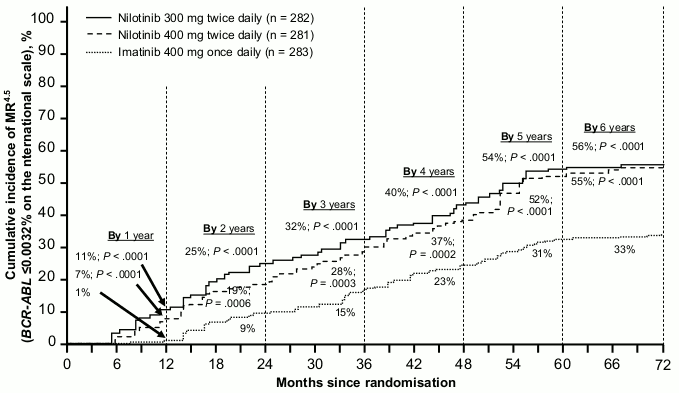
The proportion of patients who had a molecular response of ≤0.01% and ≤0.0032% by IS at different time points are presented in Table 8 and the proportion of patients who had a molecular response of ≤0.01% and ≤0.0032% by IS by different time points are presented in Figures 2 and 3. Molecular responses of ≤0.01% and ≤0.0032% by IS correspond to a ≥4 log reduction and ≥4.5 log reduction, respectively, of BCR-ABL transcripts from a standardised baseline.
Table 8. Proportions of patients who had molecular response of ≤0.01% (4 log reduction) and ≤0.0032% (4.5 log reduction):
| Nilotinib 300 mg twice daily n=282 (%) | Nilotinib 400 mg twice daily n=281 (%) | Imatinib 400 mg once daily n=283 (%) | ||||
|---|---|---|---|---|---|---|
| ≤0.01% | ≤0.0032% | ≤0.01% | ≤0.0032% | ≤0.01% | ≤0.0032% | |
| At 12 months | 11.7 | 4.3 | 8.5 | 4.6 | 3.9 | 0.4 |
| At 24 months | 24.5 | 12.4 | 22.1 | 7.8 | 10.2 | 2.8 |
| At 36 months | 29.4 | 13.8 | 23.8 | 12.1 | 14.1 | 8.1 |
| At 48 months | 33.0 | 16.3 | 29.9 | 17.1 | 19.8 | 10.2 |
| At 60 months | 47.9 | 32.3 | 43.4 | 29.5 | 31.1 | 19.8 |
| At 72 months | 44.3 | 31.2 | 45.2 | 28.8 | 27.2 | 18.0 |
Figure 2. Cumulative incidence of molecular response of ≤0.01% (4-log reduction):
Figure 3. Cumulative incidence of molecular response of ≤0.0032% (4.5 log reduction):
Based on Kaplan-Meier estimates of the duration of first MMR, the proportions of patients who were maintaining response for 72 months among patients who achieved MMR were 92.5% (95% CI: 88.6-96.4%) in the nilotinib 300 mg twice daily group, 92.2% (95% CI: 88.5-95.9%) in the nilotinib 400 mg twice daily group and 88.0% (95% CI: 83.0-93.1%) in the imatinib 400 mg once daily group.
Complete cytogenetic response (CCyR) was defined as 0% Ph+ metaphases in the bone marrow based on a minimum of 20 metaphases evaluated. Best CCyR rate by 12 months (including patients who achieved CCyR at or before the 12 month time point as responders) was statistically higher for both nilotinib 300 mg and 400 mg twice daily compared to imatinib 400 mg once daily, see Table 9.
CCyR rate by 24 months (includes patients who achieved CCyR at or before the 24 month time point as responders) was statistically higher for both the nilotinib 300 mg twice daily and 400 mg twice daily groups compared to the imatinib 400 mg once daily group.
Table 9. Best CCyR rate:
| Nilotinib 300 mg twice daily n=282 (%) | Nilotinib 400 mg twice daily n=281 (%) | Imatinib 400 mg once daily n=283 (%) | |
|---|---|---|---|
| By 12 months | |||
| Response (95% CI) | 80.1 (75.0; 84.6) | 77.9 (72.6; 82.6) | 65.0 (59.2; 70.6) |
| No response | 19.9 | 22.1 | 35.0 |
| CMH test p-value for response rate (versus imatinib 400 mg once daily) | <0.0001 | 0.0005 | |
| By 24 months | |||
| Response (95% CI) | 86.9 (82.4; 90.6) | 84.7 (79.9; 88.7) | 77.0 (71.7; 81.8) |
| No response | 13.1 | 15.3 | 23.0 |
| CMH test p-value for response rate (versus imatinib 400 mg once daily) | 0.0018 | 0.0160 | |
Based on Kaplan-Meier estimates, the proportions of patients who were maintaining response for 72 months among patients who achieved CCyR were 99.1% (95% CI: 97.9-100%) in the nilotinib 300 mg twice daily group, 98.7% (95% CI: 97.1-100%) in the nilotinib 400 mg twice daily group and 97.0% (95% CI: 94.7-99.4%) in the imatinib 400 mg once daily group.
Progression to accelerated phase (AP) or blast crisis (BC) on treatment is defined as the time from the date of randomisation to the first documented disease progression to accelerated phase or blast crisis or CML-related death. Progression to accelerated phase or blast crisis on treatment was observed in a total of 17 patients: 2 patients on nilotinib 300 mg twice daily, 3 patients on nilotinib 400 mg twice daily and 12 patients on imatinib 400 mg once daily. The estimated rates of patients free from progression to accelerated phase or blast crisis at 72 months were 99.3%, 98.7% and 95.2%, respectively (HR=0.1599 and stratified log-rank p=0.0059 between nilotinib 300 mg twice daily and imatinib once daily, HR=0.2457 and stratified log-rank p=0.0185 between nilotinib 400 mg twice daily and imatinib once daily). No new events of progression to AP/BC were reported on-treatment since the 2-year analysis.
Including clonal evolution as a criterion for progression, a total of 25 patients progressed to accelerated phase or blast crisis on treatment by the cut-off date (3 in the nilotinib 300 mg twice daily group, 5 in the nilotinib 400 mg twice daily group and 17 in the imatinib 400 mg once daily group). The estimated rates of patients free from progression to accelerated phase or blast crisis including clonal evolution at 72 months were 98.7%, 97.9% and 93.2%, respectively (HR=0.1626 and stratified log-rank p=0.0009 between nilotinib 300 mg twice daily and imatinib once daily, HR=0.2848 and stratified log-rank p=0.0085 between nilotinib 400 mg twice daily and imatinib once daily).
A total of 55 patients died during treatment or during the follow-up after discontinuation of treatment (21 in the nilotinib 300 mg twice daily group, 11 in the nilotinib 400 mg twice daily group and 23 in the imatinib 400 mg once daily group). Twenty-six (26) of these 55 deaths were related to CML (6 in the nilotinib 300 mg twice daily group, 4 in the nilotinib 400 mg twice daily group and 16 in the imatinib 400 mg once daily group). The estimated rates of patients alive at 72 months were 91.6%, 95.8% and 91.4%, respectively (HR=0.8934 and stratified log-rank p=0.7085 between nilotinib 300 mg twice daily and imatinib, HR=0.4632 and stratified log-rank p=0.0314 between nilotinib 400 mg twice daily and imatinib). Considering only CML-related deaths as events, the estimated rates of overall survival at 72 months were 97.7%, 98.5% and 93.9%, respectively (HR=0.3694 and stratified log-rank p=0.0302 between nilotinib 300 mg twice daily and imatinib, HR=0.2433 and stratified log-rank p=0.0061 between nilotinib 400 mg twice daily and imatinib).
Clinical studies in imatinib-resistant or intolerant CML in chronic phase and accelerated phase
An open-label, uncontrolled, multicentre Phase II study was conducted to determine the efficacy of nilotinib in adult patients with imatinib resistant or intolerant CML with separate treatment arms for chronic and accelerated phase disease. Efficacy was based on 321 CP patients and 137 AP patients enrolled. Median duration of treatment was 561 days for CP patients and 264 days for AP patients (see Table 10). Tasigna was administered on a continuous basis (twice daily 2 hours after a meal and with no food for at least one hour after administration) unless there was evidence of inadequate response or disease progression. The dose was 400 mg twice daily and dose escalation to 600 mg twice daily was allowed.
Table 10. Duration of exposure with nilotinib:
| Chronic phase n=321 | Accelerated phase n=137 | |
|---|---|---|
| Median duration of therapy in days (25th-75th percentiles) | 561 (196-852) | 264 (115-595) |
Resistance to imatinib included failure to achieve a complete haematological response (by 3 months), cytogenetic response (by 6 months) or major cytogenetic response (by 12 months) or progression of disease after a previous cytogenetic or haematological response. Imatinib intolerance included patients who discontinued imatinib because of toxicity and were not in major cytogenetic response at time of study entry.
Overall, 73% of patients were imatinib-resistant, while 27% were imatinib-intolerant. The majority of patients had a long history of CML that included extensive prior treatment with other antineoplastic agents, including imatinib, hydroxyurea, interferon, and some had even failed organ transplant (Table 11). The median highest prior imatinib dose had been 600 mg/day. The highest prior imatinib dose was ≥600 mg/day in 74% of all patients, with 40% of patients receiving imatinib doses ≥800 mg/day.
Table 11. CML disease history characteristics:
| Chronic phase (n=321) | Accelerated phase (n=137)* | |
|---|---|---|
| Median time since diagnosis in months (range) | 58 (5-275) | 71 (2-298) |
| Imatinib | ||
| Resistant | 226 (70%) | 109 (80%) |
| Intolerant without MCyR | 95 (30%) | 27 (20%) |
| Median time of imatinib treatment in days (25th-75th percentiles) | 975 (519-1.488) | 857 (424-1.497) |
| Prior hydroxyurea | 83% | 91% |
| Prior interferon | 58% | 50% |
| Prior bone marrow transplant | 7% | 8% |
* Missing information on imatinib-resistant/intolerant status for one patient.
The primary endpoint in the CP patients was major cytogenetic response (MCyR), defined as elimination (CCyR, complete cytogenetic response) or significant reduction to <35% Ph+ metaphases (partial cytogenetic response) of Ph+ haematopoietic cells. Complete haematological response (CHR) in CP patients was evaluated as a secondary endpoint. The primary endpoint in the AP patients was overall confirmed haematological response (HR), defined as either a complete haematological response, no evidence of leukaemia or return to chronic phase.
Chronic phase
The MCyR rate in 321 CP patients was 51%. Most responders achieved their MCyR rapidly within 3 months (median 2.8 months) of starting nilotinib treatment and these were sustained. The median time to achieve CCyR was just past 3 months (median 3.4 months). Of the patients who achieved MCyR, 77% (95% CI: 70% - 84%) were maintaining response at 24 months. Median duration of MCyR has not been reached. Of the patients who achieved CCyR, 85% (95% CI: 78%-93%) were maintaining response at 24 months. Median duration of CCyR has not been reached. Patients with a CHR at baseline achieved a MCyR faster (1.9 versus 2.8 months). Of CP patients without a baseline CHR, 70% achieved a CHR, median time to CHR was 1 month and median duration of CHR was 32.8 months. The estimated 24-month overall survival rate in CML-CP patients was 87%.
Accelerated phase
The overall confirmed HR rate in 137 AP patients was 50%. Most responders achieved a HR early with nilotinib treatment (median 1.0 months) and these have been durable (median duration of confirmed HR was 24.2 months). Of the patients who achieved HR, 53% (95% CI: 39%-67%) were maintaining response at 24 months. MCyR rate was 30% with a median time to response of 2.8 months. Of the patients who achieved MCyR, 63% (95% CI: 45%-80%) were maintaining response at 24 months. Median duration of MCyR was 32.7 months. The estimated 24-month overall survival rate in CML-AP patients was 70%.
The rates of response for the two treatment arms are reported in Table 12.
Table 12. Response in CML:
| (Best response rate) | Chronic phase | Accelerated phase | ||||
|---|---|---|---|---|---|---|
| Intolerant (n=95) | Resistant (n=226) | Total (n=321) | Intolerant (n=27) | Resistant (n=109) | Total* (n=137) | |
| Haematological Response (%) | ||||||
| Overall (95% CI) | - | - | - | 48 (29-68) | 51 (42-61) | 50 (42-59) |
| Complete | 87 (74-94) | 65 (56-72) | 701 (63-76) | 37 | 28 | 30 |
| NEL | - | - | - | 7 | 10 | 9 |
| Return to CP | - | - | - | 4 | 13 | 11 |
| Cytogenetic Response (%) | ||||||
| Major (95% CI) | 57 (46-67) | 49 (42-56) | 51 (46-57) | 33 (17-54) | 29 (21-39) | 30 (22-38) |
| Complete | 41 | 35 | 37 | 22 | 19 | 20 |
| Partial | 16 | 14 | 15 | 11 | 10 | 10 |
NEL = no evidence of leukaemia/marrow response
1 114 CP patients had a CHR at baseline and were therefore not assessable for complete haematological response
* Missing information on imatinib-resistant/intolerant status for one patient.
Efficacy data in patients with CML-BC are not yet available. Separate treatment arms were also included in the Phase II study to investigate Tasigna in a group of CP and AP patients who had been extensively pre-treated with multiple therapies including a tyrosine kinase inhibitor agent in addition to imatinib. Of these patients 30/36 (83%) were treatment resistant not intolerant. In 22 CP patients evaluated for efficacy nilotinib induced a 32% MCyR rate and a 50% CHR rate. In 11 AP patients, evaluated for efficacy, treatment induced a 36% overall HR rate.
After imatinib failure, 24 different BCR-ABL mutations were noted in 42% of chronic phase and 54% of accelerated phase CML patients who were evaluated for mutations. Tasigna demonstrated efficacy in patients harboring a variety of BCR-ABL mutations associated with imatinib resistance, except T315I.
Treatment discontinuation in adult Ph+ CML patients in chronic phase who have been treated with nilotinib as first-line therapy and who have achieved a sustained deep molecular response
n an open-label, single-arm study, 215 adult patients with Ph+ CML in chronic phase treated with nilotinib in first-line for ≥2 years who achieved MR4.5 as measured with the MolecularMD MRDx BCR-ABL test were enrolled to continue nilotinib treatment for additional 52 weeks (nilotinib consolidation phase). 190 of 215 patients (88.4%) entered the TFR phase after achieving a sustained deep molecular response during the consolidation phase, defined by the following criteria:
- the 4 last quarterly assessments (taken every 12 weeks) were at least MR4.0 (BCR-ABL/ABL ≤0.01% IS), and maintained for one year
- the last assessment being MR4.5 (BCR-ABL/ABL ≤0.0032% IS)
- no more than two assessments falling between MR4.0 and MR4.5 (0.0032% IS < BCR-ABL/ABL ≤0.01% IS).
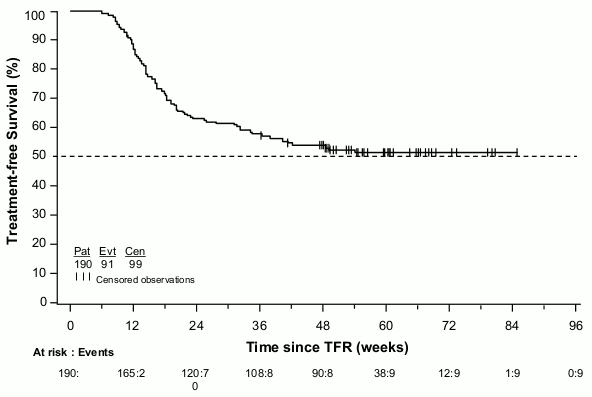
The primary endpoint was the percentage of patients in MMR at 48 weeks after starting the TFR phase (considering any patient who required re-initiation of treatment as non-responder). Of the 190 patients who entered the TFR phase, 98 patients (51.6% [95% CI: 44.2, 58.9]) were in MMR at 48 weeks.
Eighty-eight patients (46.3%) discontinued the TFR phase due to loss of MMR, and 1 (0.5%), 1 (0.5%), and 3 patients (1.6%) due to death from unknown cause, physician decision and subject decision, respectively. Among these 88 patients, 86 patients restarted nilotinib treatment and 2 patients permanently discontinued the study. Eighty-five of these 86 patients (98.8%) regained MMR, (one patient discontinued study permanently due to subject decision) and 76 patients (88.4%) regained MR4.5 by the time of the cut-off date.
The Kaplan-Meier (KM) estimated median time on nilotinib treatment to regain MMR and MR4.5 was 7.9 weeks (95% CI: 5.1, 8.0) and 13.1 weeks (95% CI: 12.3, 15.7), respectively. The KM estimated MMR and MR4.5 rates at 24 weeks of re-initiation were 98.8% (95% CI: 94.2, 99.9) and 90.9% (95% CI: 83.2, 96.0), respectively.
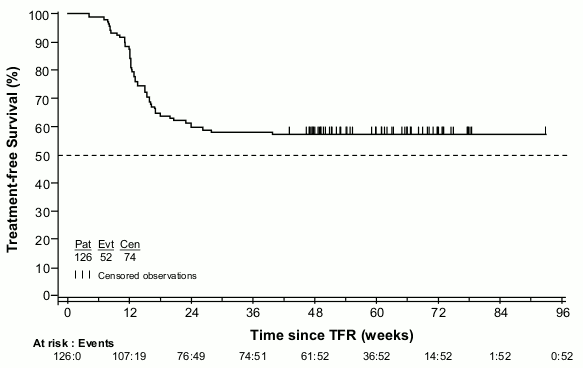
The KM estimate of median treatment-free survival (TFS) has not yet been reached (Figure 4); 99 of 190 patients (52.1%) did not have a TFS event.
Figure 4. Kaplan-Meier estimate of treatment-free survival after start of TFR (full analysis set):
Treatment discontinuation in adult CML patients in chronic phase who have achieved a sustained deep molecular response on nilotinib treatment following prior imatinib therapy
In an open-label, single-arm study, 163 adult patients with Ph+ CML in chronic phase taking tyrosine kinase inhibitors (TKIs) for ≥3 years (imatinib as initial TKI therapy for more than 4 weeks without documented MR4.5 on imatinib at the time of switch to nilotinib, then switched to nilotinib for at least two years), and who achieved MR4.5 on nilotinib treatment as measured with the MolecularMD MRDx BCR-ABL test were enrolled to continue nilotinib treatment for additional 52 weeks (nilotinib consolidation phase). 126 of 163 patients (77.3%) entered the TFR phase after achieving a sustained deep molecular response during the consolidation phase, defined by the following criterion:
- The 4 last quarterly assessments (taken every 12 weeks) showed no confirmed loss of MR4.5 (BCR-ABL/ABL ≤0.0032% IS) during one year.
The primary endpoint was the proportion of patients without confirmed loss of MR4.0 or loss of MMR within 48 weeks following treatment discontinuation. Of the 126 patients who entered the TFR phase, 73 patients (57.9%, [95% CI: 48.8, 66.7]) had no loss of MMR, no confirmed loss of MR4.0, and no re-initiation of nilotinib within 48 weeks.
Among the 53 patients who discontinued the TFR phase due to confirmed loss of MR4.0 or loss of MMR, 51 patients restarted nilotinib and 2 patients discontinued the study. Forty-eight of these 51 patients (94.1%) regained MR4.0 and 47 patients (92.2%) regained MR4.5 by the time of the cut-off date.
The Kaplan-Meier (KM) estimated median time on nilotinib to regain MR4.0 and MR4.5 was 12.0 weeks (95% CI: 8.3, 12.7) and 13.1 weeks (95% CI: 12.4, 16.1), respectively. The KM estimated MR4.0 and MR4.5 rates at 48 weeks of re-initiation were 100.0% (95% CI: not estimated) and 94.8% (95% CI: 85.1, 99.0), respectively.
The median TFS has not yet been reached (Figure 5); 74 of 126 patients (58.7%) did not have a TFS event.
Figure 5. Kaplan-Meier estimate of treatment-free survival after start of TFR (full analysis set):
Paediatric population
The safety and efficacy of nilotinib in paediatric patients with Ph+ CML in chronic phase have been investigated in two studies. A total of 69 paediatric patients (from 2 to <18 years of age) with either newly diagnosed Ph+ CML in chronic phase (n=25) or imatinib/dasatinib resistant or imatinib-intolerant Ph+ CML in chronic phase (n=44) received nilotinib treatment at a dose of 230 mg/m² twice daily, rounded to the nearest 50 mg dose (to a maximum single dose of 400 mg).
In the pooled CML patient population, the median actual dose intensity was 435.5 mg/m²/day (range: 149 to 517 mg/m²/day), and the median relative dose intensity was 94.7% (range: 32 to 112%). Forty patients (58.0%) had relative dose intensity superior to 90%. The median time on treatment with nilotinib was 13.80 months (range: 0.7-30.9 months).
In the resistant or intolerant CML patients, the major molecular response (MMR; BCR-ABL/ABL ≤0.1% IS) rate was 40.9% (95% CI: 26.3, 56.8) at 12 cycles, with 18 patients being in MMR. In the newly diagnosed CML patients, the MMR rate was 60.0% (95% CI: 38.7, 78.9) at 12 cycles, with 15 patients achieving MMR. In resistant or intolerant CML patients, the cumulative MMR rate was 47.7% by cycle 12. In newly diagnosed CML patients, the cumulative MMR rate was 64.0% by cycle 12.
Among the 21 resistant or intolerant CML patients who were in MMR at any time on treatment, the median time to first MMR was 2.76 months (95% CI: 0.03, 5.55). For the 17 newly diagnosed CML patients who achieved MMR, the median time to first MMR was 5.55 months (95% CI: 5.52, 5.75).
Among resistant or intolerant CML patients, the percentage of patients who achieved BCR-ABL/ABL ≤0.01% IS (MR4.0) by the cut-off date was 11.4%, while 4.5% of the patients achieved BCR-ABL/ABL ≤0.0032% IS (MR4.5). Among newly diagnosed patients, the percentage of patients who achieved MR4.0 was 32%, while 28.0% achieved MR4.5.
None of the 21 resistant or intolerant CML patients who were in MMR on treatment had confirmed loss of MMR. Among the 17 newly diagnosed CML patients who achieved MMR, one patient had confirmed loss of MMR (the patient lost CHR due to an increase in basophil count, however did not progress to AP/BC).
One resistant or intolerant CML patient progressed to AP/BC after about 10 months on treatment.
No deaths were reported on treatment or after treatment discontinuation in both studies.
Pharmacokinetic properties
Absorption
Peak concentrations of nilotinib are reached 3 hours after oral administration. Nilotinib absorption following oral administration was approximately 30%. The absolute bioavailability of nilotinib has not been determined. As compared to an oral drink solution (pH of 1.2 to 1.3), relative bioavailability of nilotinib capsule is approximately 50%. In healthy volunteers, Cmax and area under the serum concentration-time curve (AUC) of nilotinib are increased by 112% and 82%, respectively, compared to fasting conditions when Tasigna is given with food. Administration of Tasigna 30 minutes or 2 hours after food increased bioavailability of nilotinib by 29% or 15%, respectively (see sections 4.2, 4.4 and 4.5).
Nilotinib absorption (relative bioavailability) might be reduced by approximately 48% and 22% in patients with total gastrectomy and partial gastrectomy, respectively.
Distribution
The blood-to-plasma ratio of nilotinib is 0.71. Plasma protein binding is approximately 98% on the basis of in vitro experiments. Biotransformation Main metabolic pathways identified in healthy subjects are oxidation and hydroxylation. Nilotinib is the main circulating component in the serum. None of the metabolites contribute significantly to the pharmacological activity of nilotinib. Nilotinib is primarily metabolised by CYP3A4, with possible minor contribution from CYP2C8.
Elimination
After a single dose of radiolabelled nilotinib in healthy subjects, more than 90% of the dose was eliminated within 7 days, mainly in faeces (94% of the dose). Unchanged nilotinib accounted for 69% of the dose.
The apparent elimination half-life estimated from the multiple-dose pharmacokinetics with daily dosing was approximately 17 hours. Inter-patient variability in nilotinib pharmacokinetics was moderate to high.
Linearity/non-linearity
Steady-state nilotinib exposure was dose-dependent, with less than dose-proportional increases in systemic exposure at dose levels higher than 400 mg given as once-daily dosing. Daily systemic exposure to nilotinib with 400 mg twice-daily dosing at steady state was 35% higher than with 800 mg once-daily dosing. Systemic exposure (AUC) of nilotinib at steady state at a dose level of 400 mg twice daily was approximately 13.4% higher than at a dose level of 300 mg twice daily. The average nilotinib trough and peak concentrations over 12 months were approximately 15.7% and 14.8% higher following 400 mg twice-daily dosing compared to 300 mg twice daily. There was no relevant increase in exposure to nilotinib when the dose was increased from 400 mg twice daily to 600 mg twice daily.
Steady-state conditions were essentially achieved by day 8. An increase in serum exposure to nilotinib between the first dose and steady state was approximately 2-fold for daily dosing and 3.8-fold for twice-daily dosing.
Bioavailability/bioequivalence studies
Single-dose administration of 400 mg nilotinib, using 2 hard capsules of 200 mg whereby the content of each hard capsule was dispersed in one teaspoon of apple sauce, was shown to be bioequivalent with a single-dose administration of 2 intact hard capsules of 200 mg.
Paediatric population
Following administration of nilotinib in paediatric patients at 230 mg/m² twice daily, rounded to the nearest 50 mg dose (to a maximum single dose of 400 mg), steady-state exposure and clearance of nilotinib were found to be similar (within 2-fold) to adult patients treated with 400 mg twice daily. The pharmacokinetic exposure of nilotinib following a single or multiple doses appeared to be comparable between paediatric patients from 2 years to <10 years and from ≥10 years to <18 years.
Preclinical safety data
Nilotinib has been evaluated in safety pharmacology, repeated-dose toxicity, genotoxicity, reproductive toxicity, phototoxicity and carcinogenicity (rats and mice) studies.
Safety pharmacology studies
Nilotinib did not have effects on CNS or respiratory functions. In vitro cardiac safety studies demonstrated a preclinical signal for QT prolongation, based upon block of hERG currents and prolongation of the action potential duration in isolated rabbit hearts by nilotinib. No effects were seen in ECG measurements in dogs or monkeys treated for up to 39 weeks or in a special telemetry study in dogs.
Repeated-dose toxicity studies
Repeated-dose toxicity studies in dogs of up to 4 weeks' duration and in cynomolgus monkeys of up to 9 months' duration revealed the liver as the primary target organ of toxicity of nilotinib. Alterations included increased alanine aminotransferase and alkaline phosphatase activity and histopathology findings (mainly sinusoidal cell or Kupffer cell hyperplasia/hypertrophy, bile duct hyperplasia and periportal fibrosis). In general the changes in clinical chemistry were fully reversible after a four-week recovery period and the histological alterations showed partial reversibility. Exposures at the lowest dose levels at which the liver effects were seen were lower than the exposure in humans at a dose of 800 mg/day. Only minor liver alterations were seen in mice or rats treated for up to 26 weeks. Mainly reversible increases in cholesterol levels were seen in rats, dogs and monkeys.
Genotoxicity studies
Genotoxicity studies in bacterial in vitro systems and in mammalian in vitro and in vivo systems with and without metabolic activation did not reveal any evidence for a mutagenic potential of nilotinib.
Carcinogenicity studies
In the 2-year rat carcinogenicity study, the major target organ for non-neoplastic lesions was the uterus (dilatation, vascular ectasia, endothelial cell hyperplasia, inflammation and/or epithelial hyperplasia). There was no evidence of carcinogenicity upon administration of nilotinib at 5, 15 and 40 mg/kg/day. Exposures (in terms of AUC) at the highest dose level represented approximately 2x to 3x human daily steady-state exposure (based on AUC) to nilotinib at the dose of 800 mg/day.
In the 26-week Tg.rasH2 mouse carcinogenicity study, in which nilotinib was administered at 30, 100 and 300 mg/kg/day, skin papillomas/carcinomas were detected at 300 mg/kg, representing approximately 30 to 40 times (based on AUC) the human exposure at the maximum approved dose of 800 mg/day (administered as 400 mg twice daily). The No-Observed-Effect-Level for the skin neoplastic lesions was 100 mg/kg/day, representing approximately 10 to 20 times the human exposure at the maximum approved dose of 800 mg/day (administered as 400 mg twice daily). The major target organs for non-neoplastic lesions were the skin (epidermal hyperplasia), the growing teeth (degeneration/atrophy of the enamel organ of upper incisors and inflammation of the gingiva/odontogenic epithelium of incisors) and the thymus (increased incidence and/or severity of decreased lymphocytes).
Reproductive toxicity and fertility studies
Nilotinib did not induce teratogenicity, but did show embryo- and foetotoxicity at doses that also showed maternal toxicity. Increased post-implantation loss was observed in both the fertility study, which involved treatment of both males and females, and the embryotoxicity study, which involved treatment of females. Embryo-lethality and foetal effects (mainly decreased foetal weights, premature fusion of the facial bones (fused maxilla/zygomatic) visceral and skeletal variations) in rats and increased resorption of foetuses and skeletal variations in rabbits were present in the embryotoxicity studies. In a pre- and postnatal development study in rats, maternal exposure to nilotinib caused reduced pup body weight with associated changes in physical development parameters as well as reduced mating and fertility indices in the offspring. Exposure to nilotinib in females at No-Observed-Adverse-Effect-Levels was generally less or equal to that in humans at 800 mg/day.
No effects on sperm count/motility or on fertility were noted in male and female rats up to the highest tested dose, approximately 5 times the recommended dosage for humans.
Juvenile animal studies
In a juvenile development study, nilotinib was administered via oral gavage to juvenile rats from the first week post partum through young adult (day 70 post partum) at doses of 2, 6 and 20 mg/kg/day. Besides standard study parameters, evaluations of developmental landmarks, CNS effects, mating and fertility were performed. Based on a reduction in body weight in both genders and a delayed preputial separation in males (which may be associated with the reduction in weight), the No-Observed-Effect-Level in juvenile rats was considered to be 6 mg/kg/day. The juvenile animals did not exert increased sensitivity to nilotinib relative to adults. In addition, the toxicity profile in juvenile rats was comparable to that observed in adult rats.
Phototoxicity studies
Nilotinib was shown to absorb light in the UV-B and UV-A range, is distributed into the skin and showed a phototoxic potential in vitro, but no effects have been observed in vivo. Therefore the risk that nilotinib causes photosensitisation in patients is considered very low.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.