TRUVADA Film-coated tablet Ref.[27928] Active ingredients: Emtricitabine Tenofovir disoproxil Tenofovir disoproxil and Emtricitabine
Source: European Medicines Agency (EU) Revision Year: 2023 Publisher: Gilead Sciences Ireland UC, Carrigtohill, County Cork, T45 DP77, Ireland
4.3. Contraindications
Hypersensitivity to the active substances or to any of the excipients listed in section 6.1.
Use for pre-exposure prophylaxis in individuals with unknown or positive HIV-1 status.
4.4. Special warnings and precautions for use
Patients with HIV-1 harbouring mutations
Truvada should be avoided in antiretroviral-experienced patients with HIV-1 harbouring the K65R mutation (see section 5.1).
Overall HIV-1 infection prevention strategy
Truvada is not always effective in preventing the acquisition of HIV-1. The time to onset of protection after commencing Truvada is unknown.
Truvada should only be used for pre-exposure prophylaxis as part of an overall HIV-1 infection prevention strategy including the use of other HIV-1 prevention measures (e.g. consistent and correct condom use, knowledge of HIV-1 status, regular testing for other sexually transmitted infections).
Risk of resistance with undetected HIV-1 infection
Truvada should only be used to reduce the risk of acquiring HIV-1 in individuals confirmed to be HIV negative (see section 4.3). Individuals should be re-confirmed to be HIV-negative at frequent intervals (e.g. at least every 3 months) using a combined antigen/antibody test while taking Truvada for pre-exposure prophylaxis.
Truvada alone does not constitute a complete regimen for the treatment of HIV-1 and HIV-1 resistance mutations have emerged in individuals with undetected HIV-1 infection who are only taking Truvada.
If clinical symptoms consistent with acute viral infection are present and recent (<1 month) exposures to HIV-1 are suspected, use of Truvada should be delayed for at least one month and HIV-1 status reconfirmed before starting Truvada for pre-exposure prophylaxis.
Importance of adherence
The effectiveness of Truvada in reducing the risk of acquiring HIV-1 is strongly correlated with adherence as demonstrated by measurable drug levels in blood (see section 5.1). HIV-1 uninfected individuals should be counselled at frequent intervals to strictly adhere to the recommended Truvada daily dosing schedule.
Patients with hepatitis B or C virus infection
HIV-1 infected patients with chronic hepatitis B or C treated with antiretroviral therapy are at an increased risk for severe and potentially fatal hepatic adverse reactions. Physicians should refer to current HIV treatment guidelines for the management of HIV infection in patients co-infected with hepatitis B virus (HBV) or hepatitis C virus (HCV).
The safety and efficacy of Truvada for pre-exposure prophylaxis in patients with HBV or HCV infection has not been established.
In case of concomitant antiviral therapy for hepatitis B or C, please refer also to the relevant Summary of Product Characteristics for these medicinal products. See also under Use with ledipasvir and sofosbuvir or sofosbuvir and velpatasvir below.
Tenofovir disoproxil is indicated for the treatment of HBV and emtricitabine has shown activity against HBV in pharmacodynamic studies but the safety and efficacy of Truvada have not been specifically established in patients with chronic HBV infection.
Discontinuation of Truvada therapy in patients infected with HBV may be associated with severe acute exacerbations of hepatitis. Patients infected with HBV who discontinue Truvada should be closely monitored with both clinical and laboratory follow-up for at least several months after stopping treatment. If appropriate, resumption of hepatitis B therapy may be warranted. In patients with advanced liver disease or cirrhosis, treatment discontinuation is not recommended since post-treatment exacerbation of hepatitis may lead to hepatic decompensation.
Liver disease
The safety and efficacy of Truvada have not been established in patients with significant underlying liver disorders. The pharmacokinetics of tenofovir has been studied in patients with hepatic impairment and no dose adjustment is required. The pharmacokinetics of emtricitabine has not been studied in patients with hepatic impairment. Based on minimal hepatic metabolism and the renal route of elimination for emtricitabine, it is unlikely that a dose adjustment would be required for Truvada in patients with hepatic impairment (see sections 4.2 and 5.2).
HIV-1 infected patients with pre-existing liver dysfunction, including chronic active hepatitis, have an increased frequency of liver function abnormalities during combination antiretroviral therapy (CART) and should be monitored according to standard practice. If there is evidence of worsening liver disease in such patients, interruption or discontinuation of treatment must be considered.
Renal and bone effects in adults
Renal effects
Emtricitabine and tenofovir are primarily excreted by the kidneys by a combination of glomerular filtration and active tubular secretion. Renal failure, renal impairment, elevated creatinine, hypophosphataemia and proximal tubulopathy (including Fanconi syndrome) have been reported with the use of tenofovir disoproxil (see section 4.8).
Renal monitoring
Prior to initiating Truvada for the treatment of HIV-1 infection or for use in pre-exposure prophylaxis, it is recommended that creatinine clearance is calculated in all individuals.
In individuals without risk factors for renal disease, it is recommended that renal function (creatinine clearance and serum phosphate) is monitored after two to four weeks of use, after three months of use and every three to six months thereafter.
In individuals at risk for renal disease more frequent monitoring of renal function is required.
See also under Co-administration of other medicinal products below.
Renal management in HIV-1 infected patients
If serum phosphate is <1.5 mg/dL (0.48 mmol/L) or creatinine clearance is decreased to <50 mL/min in any patient receiving Truvada, renal function should be re-evaluated within one week, including measurements of blood glucose, blood potassium and urine glucose concentrations (see section 4.8, proximal tubulopathy). Consideration should be given to interrupting treatment with Truvada in patients with creatinine clearance decreased to <50 mL/min or decreases in serum phosphate to <1.0 mg/dL (0.32 mmol/L). Interrupting treatment with Truvada should also be considered in case of progressive decline of renal function when no other cause has been identified.
Renal safety with Truvada has only been studied to a very limited degree in HIV-1 infected patients with impaired renal function (creatinine clearance <80 mL/min). Dose interval adjustments are recommended for HIV-1 infected patients with creatinine clearance 30-49 mL/min (see section 4.2). Limited clinical study data suggest that the prolonged dose interval is not optimal and could result in increased toxicity and possibly inadequate response. Furthermore, in a small clinical study, a subgroup of patients with creatinine clearance between 50 and 60 mL/min who received tenofovir disoproxil in combination with emtricitabine every 24 hours had a 2-4-fold higher exposure to tenofovir and worsening of renal function (see section 5.2). Therefore, a careful benefit-risk assessment is needed when Truvada is used in patients with creatinine clearance <60 mL/min, and renal function should be closely monitored. In addition, the clinical response to treatment should be closely monitored in patients receiving Truvada at a prolonged dosing interval. The use of Truvada is not recommended in patients with severe renal impairment (creatinine clearance <30 mL/min) and in patients who require haemodialysis since appropriate dose reductions cannot be achieved with the combination tablet (see sections 4.2 and 5.2).
Renal management in pre-exposure prophylaxis
Truvada has not been studied in HIV-1 uninfected individuals with creatinine clearance <60 mL/min and is therefore not recommended for use in this population. If serum phosphate is <1.5 mg/dL (0.48 mmol/L) or creatinine clearance is decreased to <60 mL/min in any individual receiving Truvada for pre-exposure prophylaxis, renal function should be re-evaluated within one week, including measurements of blood glucose, blood potassium and urine glucose concentrations (see section 4.8, proximal tubulopathy). Consideration should be given to interrupting use of Truvada in individuals with creatinine clearance decreased to <60 mL/min or decreases in serum phosphate to <1.0 mg/dL (0.32 mmol/L). Interrupting use of Truvada should also be considered in case of progressive decline of renal function when no other cause has been identified.
Bone effects
Bone abnormalities such as osteomalacia which can manifest as persistent or worsening bone pain and, which can infrequently contribute to fractures may be associated with tenofovir disoproxilinduced proximal renal tubulopathy (see section 4.8).
Tenofovir disoproxil may also cause a reduction in bone mineral density (BMD).
If bone abnormalities are suspected or detected then appropriate consultation should be obtained.
Treatment of HIV-1 infection
In a 144-week controlled clinical study (GS-99-903) that compared tenofovir disoproxil with stavudine in combination with lamivudine and efavirenz in antiretroviral-naïve patients, small decreases in BMD of the hip and spine were observed in both treatment groups. Decreases in BMD of spine and changes in bone biomarkers from baseline were significantly greater in the tenofovir disoproxil treatment group at 144 weeks. Decreases in BMD of hip were significantly greater in this group until 96 weeks. However, there was no increased risk of fractures or evidence for clinically relevant bone abnormalities over 144 weeks in this study.
In other studies (prospective and cross-sectional), the most pronounced decreases in BMD were seen in patients treated with tenofovir disoproxil as part of a regimen containing a boosted protease inhibitor. Overall in view of the bone abnormalities associated with tenofovir disoproxil and the limitations of long term data on the impact of tenofovir disoproxil on bone health and fracture risk, alternative treatment regimens should be considered for patients with osteoporosis that are at a high risk for fractures.
Pre-exposure prophylaxis
In clinical studies of HIV-1 uninfected individuals, small decreases in BMD were observed. In a study of 498 men, the mean changes from baseline to week 24 in BMD ranged from -0.4% to -1.0% across hip, spine, femoral neck and trochanter in men who received daily Truvada prophylaxis (n = 247) vs. placebo (n = 251).
Renal and bone effects in the paediatric population
There are uncertainties associated with the long-term renal and bone effects of tenofovir disoproxil during the treatment of HIV-1 infection in the paediatric population and the long-term renal and bone effects of Truvada when used for pre-exposure prophylaxis in uninfected adolescents (see section 5.1). Moreover, the reversibility of renal toxicity after cessation of tenofovir disoproxil for treatment of HIV-1 or after cessation of Truvada for pre-exposure prophylaxis cannot be fully ascertained.
A multidisciplinary approach is recommended to weigh the benefit/risk balance of the use of Truvada for the treatment of HIV-1 infection or for pre-exposure prophylaxis, decide the appropriate monitoring during treatment (including decision for treatment withdrawal) and consider the need for supplementation on a case by case basis.
When using Truvada for pre-exposure prophylaxis individuals should be reassessed at each visit to ascertain whether they remain at high risk of HIV-1 infection. The risk of HIV-1 infection should be balanced against the potential for renal and bone effects with long-term use of Truvada.
Renal effects
Renal adverse reactions consistent with proximal renal tubulopathy have been reported in HIV-1 infected paediatric patients aged 2 to <12 years in clinical study GS-US-104-0352 (see sections 4.8 and 5.1).
Renal monitoring
Renal function (creatinine clearance and serum phosphate) should be evaluated prior to initiating Truvada for treatment of HIV-1 or for pre-exposure prophylaxis, and should be monitored during use as in adults (see above).
Renal management
If serum phosphate is confirmed to be <3.0 mg/dL (0.96 mmol/L) in any paediatric patient receiving Truvada, renal function should be re-evaluated within one week, including measurements of blood glucose, blood potassium and urine glucose concentrations (see section 4.8, proximal tubulopathy). If renal abnormalities are suspected or detected then consultation with a nephrologist should be obtained to consider interruption of Truvada use. Interrupting use of Truvada should also be considered in case of progressive decline of renal function when no other cause has been identified.
Co-administration and risk of renal toxicity
The same recommendations apply as in adults (see Co-administration of other medicinal products below).
Renal impairment
The use of Truvada is not recommended in individuals under the age of 18 years with renal impairment (see section 4.2). Truvada should not be initiated in paediatric patients with renal impairment and should be discontinued in paediatric patients who develop renal impairment during Truvada use.
Bone effects
Use of tenofovir disoproxil may cause a reduction in BMD. The effects of tenofovir disoproxilassociated changes in BMD on long-term bone health and future fracture risk are uncertain (see section 5.1).
If bone abnormalities are detected or suspected during use of Truvada in any paediatric patient, consultation with an endocrinologist and/or nephrologist should be obtained.
Weight and metabolic parameters
An increase in weight and in levels of blood lipids and glucose may occur during antiretroviral therapy. Such changes may in part be linked to disease control and life style. For lipids, there is in some cases evidence for a treatment effect, while for weight gain there is no strong evidence relating this to any particular treatment. For monitoring of blood lipids and glucose reference is made to established HIV treatment guidelines. Lipid disorders should be managed as clinically appropriate.
Mitochondrial dysfunction following exposure in utero
Nucleos(t)ide analogues may impact mitochondrial function to a variable degree, which is most pronounced with stavudine, didanosine and zidovudine. There have been reports of mitochondrial dysfunction in HIV negative infants exposed in utero and/or postnatally to nucleoside analogues; these have predominantly concerned treatment with regimens containing zidovudine. The main adverse reactions reported are haematological disorders (anaemia, neutropenia) and metabolic disorders (hyperlactatemia, hyperlipasemia). These events have often been transitory. Late onset neurological disorders have been reported rarely (hypertonia, convulsion, abnormal behaviour). Whether such neurological disorders are transient or permanent is currently unknown. These findings should be considered for any child exposed in utero to nucleos(t)ide analogues, who present with severe clinical findings of unknown etiology, particularly neurologic findings. These findings do not affect current national recommendations to use antiretroviral therapy in pregnant women to prevent vertical transmission of HIV.
Immune Reactivation Syndrome
In HIV infected patients with severe immune deficiency at the time of institution of CART, an inflammatory reaction to asymptomatic or residual opportunistic pathogens may arise and cause serious clinical conditions, or aggravation of symptoms. Typically, such reactions have been observed within the first few weeks or months of initiation of CART. Relevant examples are cytomegalovirus retinitis, generalised and/or focal mycobacterial infections, and Pneumocystis jirovecii pneumonia. Any inflammatory symptoms should be evaluated and treatment instituted when necessary. Autoimmune disorders (such as Graves' disease and autoimmune hepatitis) have also been reported to occur in the setting of immune reactivation; however, the reported time to onset is more variable and these events can occur many months after initiation of treatment.
Opportunistic infections
HIV-1 infected patients receiving Truvada or any other antiretroviral therapy may continue to develop opportunistic infections and other complications of HIV infection, and therefore should remain under close clinical observation by physicians experienced in the treatment of patients with HIV associated diseases.
Osteonecrosis
Although the aetiology is considered to be multifactorial (including corticosteroid use, alcohol consumption, severe immunosuppression, higher body mass index), cases of osteonecrosis have been reported particularly in patients with advanced HIV-disease and/or long-term exposure to CART. Patients should be advised to seek medical advice if they experience joint aches and pain, joint stiffness or difficulty in movement.
Co-administration of other medicinal products
Use of Truvada should be avoided with concurrent or recent use of a nephrotoxic medicinal product (see section 4.5). If concomitant use with nephrotoxic agents is unavoidable, renal function should be monitored weekly.
Cases of acute renal failure after initiation of high dose or multiple non-steroidal anti-inflammatory drugs (NSAIDs) have been reported in HIV-1 infected patients treated with tenofovir disoproxil and with risk factors for renal dysfunction. If Truvada is co-administered with an NSAID, renal function should be monitored adequately.
A higher risk of renal impairment has been reported in HIV-1 infected patients receiving tenofovir disoproxil in combination with a ritonavir or cobicistat boosted protease inhibitor. Close monitoring of renal function is required in these patients (see section 4.5). In HIV-1 infected patients with renal risk factors, the co-administration of tenofovir disoproxil with a boosted protease inhibitor should be carefully evaluated.
Truvada should not be administered concomitantly with other medicinal products containing emtricitabine, tenofovir disoproxil, tenofovir alafenamide, or other cytidine analogues, such as lamivudine (see section 4.5). Truvada should not be administered concomitantly with adefovir dipivoxil.
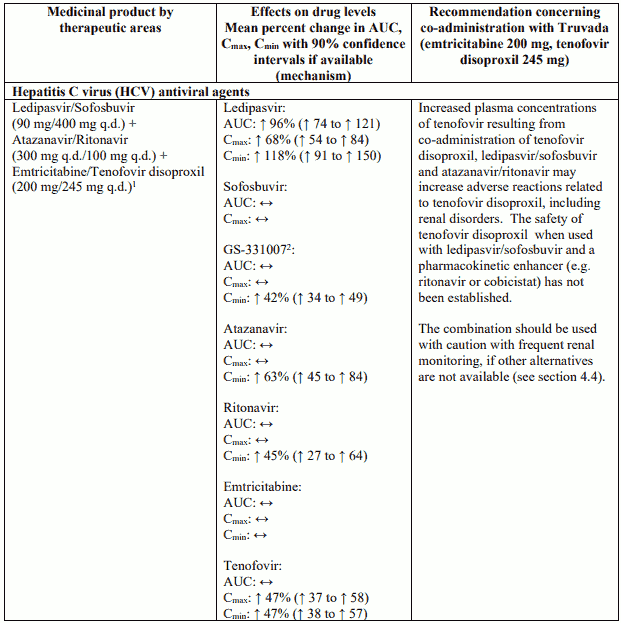
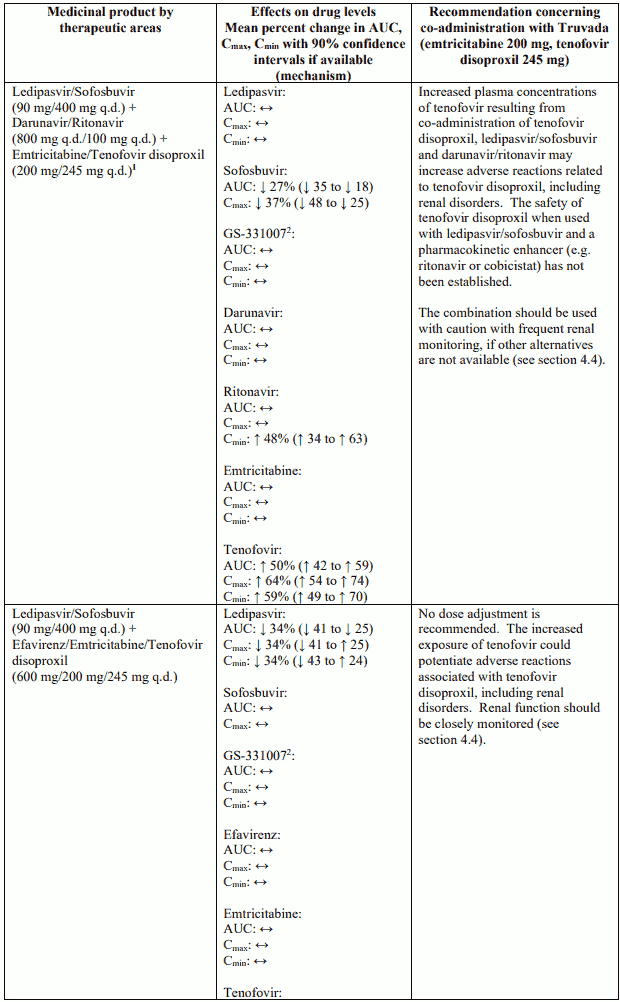
Use with ledipasvir and sofosbuvir, sofosbuvir and velpatasvir or sofosbuvir, velpatasvir and voxilaprevir
Co-administration of tenofovir disoproxil with ledipasvir/sofosbuvir, sofosbuvir/velpatasvir or sofosbuvir/velpatasvir/voxilaprevir has been shown to increase plasma concentrations of tenofovir, especially when used together with an HIV regimen containing tenofovir disoproxil and a pharmacokinetic enhancer (ritonavir or cobicistat).
The safety of tenofovir disoproxil when co-administered with ledipasvir/sofosbuvir, sofosbuvir/velpatasvir or sofosbuvir/velpatasvir/voxilaprevir and a pharmacokinetic enhancer has not been established. The potential risks and benefits associated with co-administration should be considered, particularly in patients at increased risk of renal dysfunction. Patients receiving ledipasvir/sofosbuvir, sofosbuvir/velpatasvir or sofosbuvir/velpatasvir/voxilaprevir concomitantly with tenofovir disoproxil and a boosted HIV protease inhibitor should be monitored for adverse reactions related to tenofovir disoproxil.
Co-administration of tenofovir disoproxil and didanosine
Co-administration of tenofovir disoproxil and didanosine is not recommended (see section 4.5).
Triple nucleoside therapy
There have been reports of a high rate of virological failure and of emergence of resistance at an early stage in HIV-1 infected patients when tenofovir disoproxil was combined with lamivudine and abacavir as well as with lamivudine and didanosine as a once daily regimen. There is close structural similarity between lamivudine and emtricitabine and similarities in the pharmacokinetics and pharmacodynamics of these two agents. Therefore, the same problems may be seen if Truvada is administered with a third nucleoside analogue.
Elderly
Truvada has not been studied in individuals over the age of 65 years. Individuals over the age of 65 years are more likely to have decreased renal function, therefore caution should be exercised when administering Truvada to older people.
Excipients
Truvada contains lactose monohydrate. Patients with rare hereditary problems of galactose intolerance, total lactase deficiency, or glucose-galactose malabsorption should not take this medicinal product.
This medicine contains less than 1 mmol sodium (23 mg) per tablet, that is to say essentially ‘sodiumfree’.
4.5. Interaction with other medicinal products and other forms of interaction
Interaction studies have only been performed in adults.
As Truvada contains emtricitabine and tenofovir disoproxil, any interactions that have been identified with these agents individually may occur with Truvada. Interaction studies have only been performed in adults.
The steady-state pharmacokinetics of emtricitabine and tenofovir were unaffected when emtricitabine and tenofovir disoproxil were administered together versus each medicinal product dosed alone.
In vitro and clinical pharmacokinetic interaction studies have shown the potential for CYP450 mediated interactions involving emtricitabine and tenofovir disoproxil with other medicinal products is low.
Concomitant use not recommended
Truvada should not be administered concomitantly with other medicinal products containing emtricitabine, tenofovir disoproxil, tenofovir alafenamide or other cytidine analogues, such as lamivudine (see section 4.4). Truvada should not be administered concomitantly with adefovir dipivoxil.
Didanosine
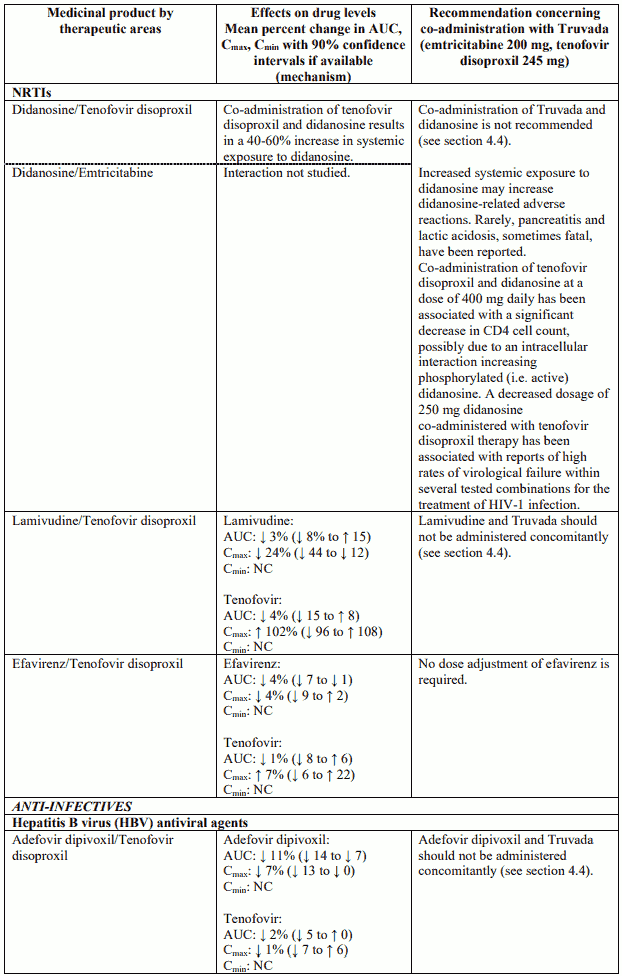
The co-administration of Truvada and didanosine is not recommended (see section 4.4 and Table 2).
Renally eliminated medicinal products
Since emtricitabine and tenofovir are primarily eliminated by the kidneys, co-administration of Truvada with medicinal products that reduce renal function or compete for active tubular secretion (e.g. cidofovir) may increase serum concentrations of emtricitabine, tenofovir and/or the co-administered medicinal products.
Use of Truvada should be avoided with concurrent or recent use of a nephrotoxic medicinal product. Some examples include, but are not limited to, aminoglycosides, amphotericin B, foscarnet, ganciclovir, pentamidine, vancomycin, cidofovir or interleukin-2 (see section 4.4).
Other interactions
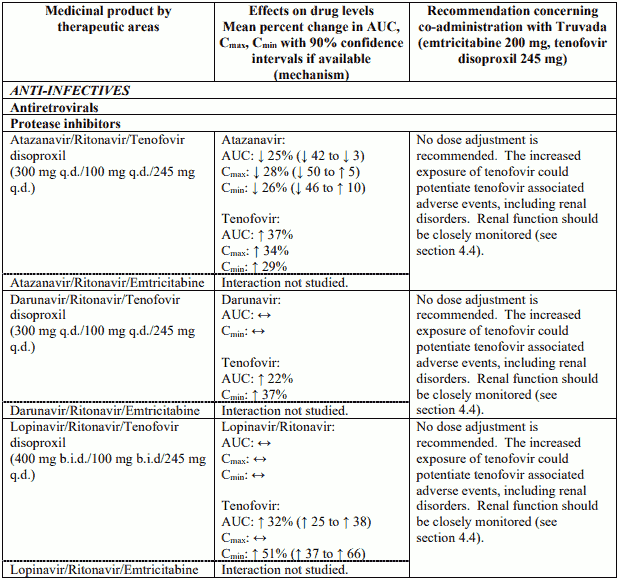
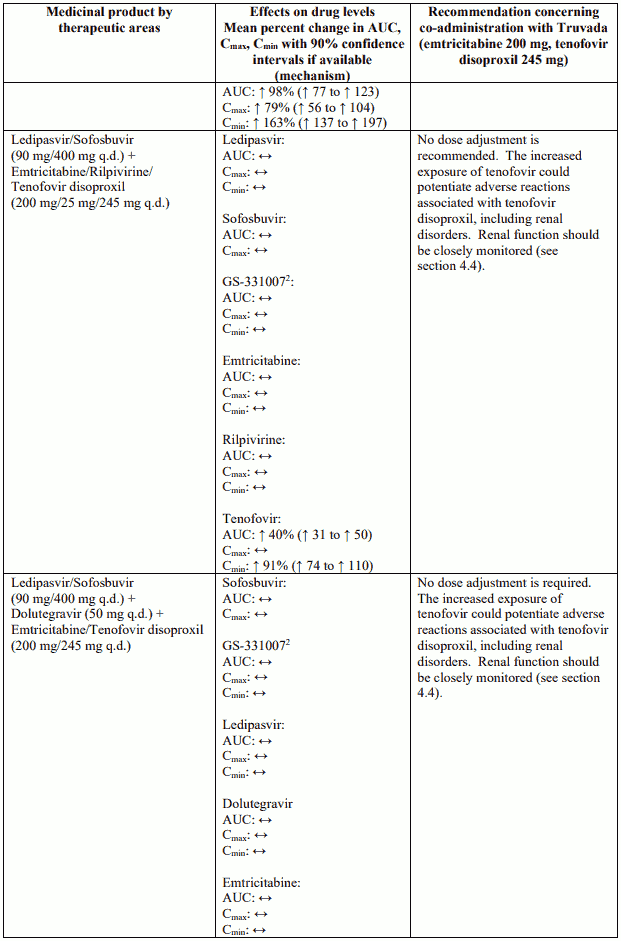
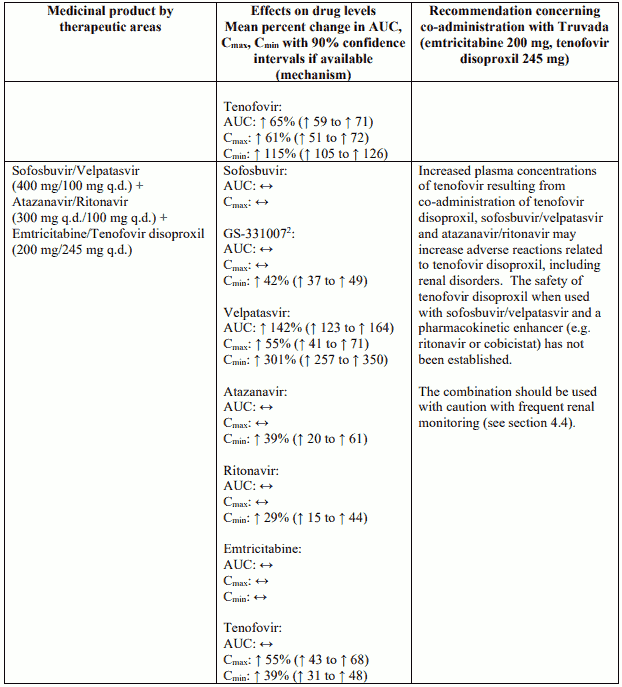
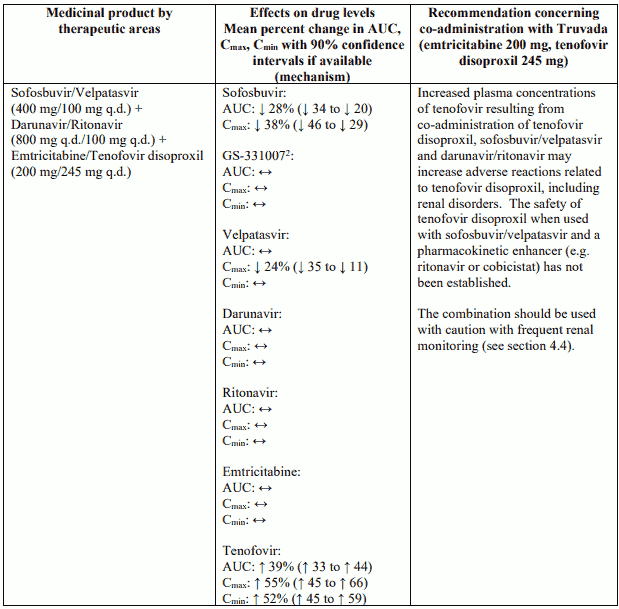
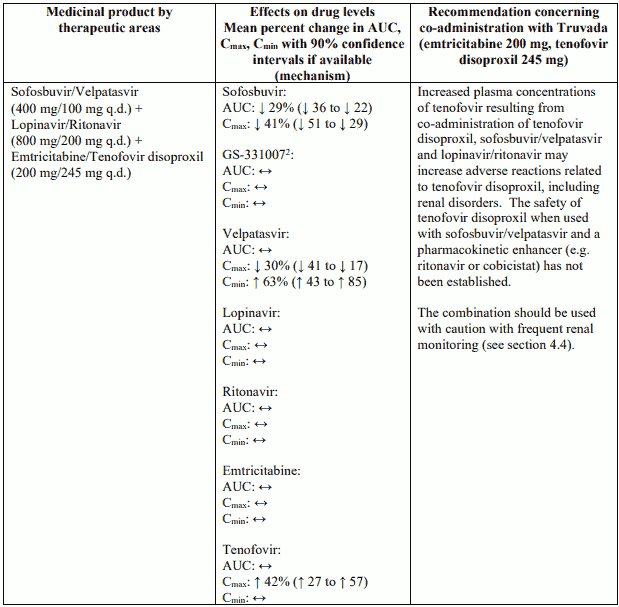
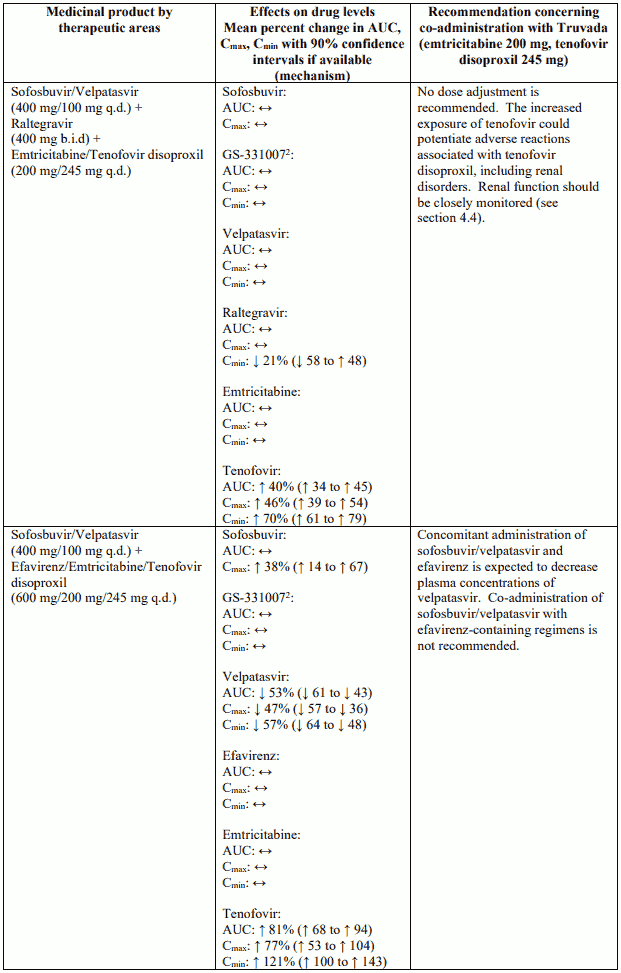
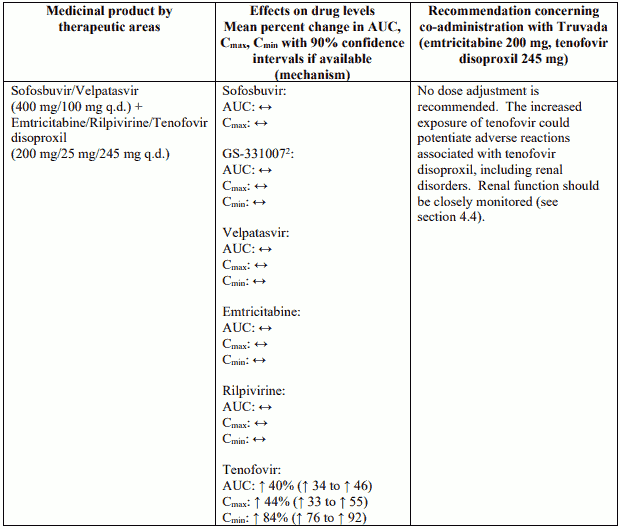
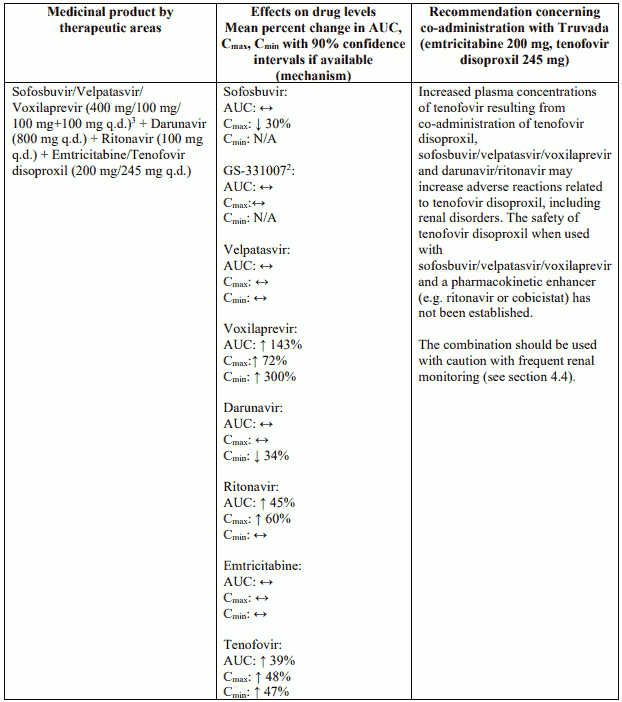
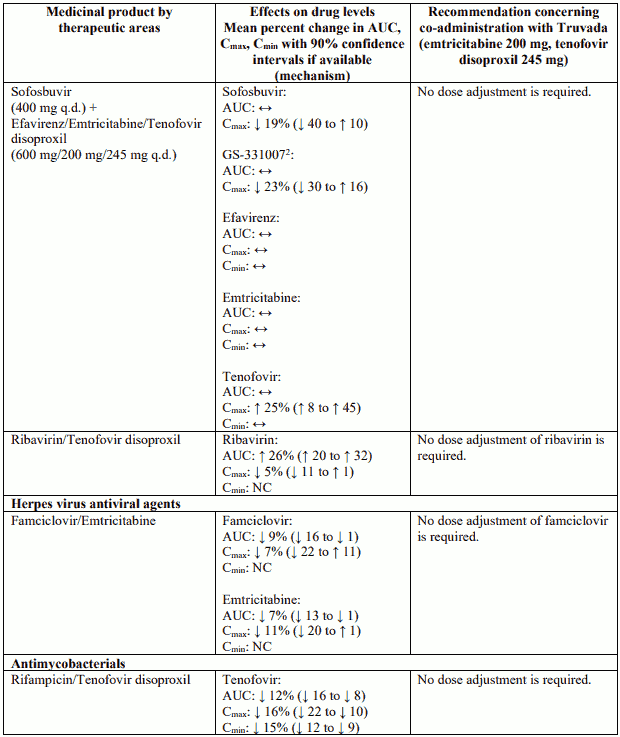
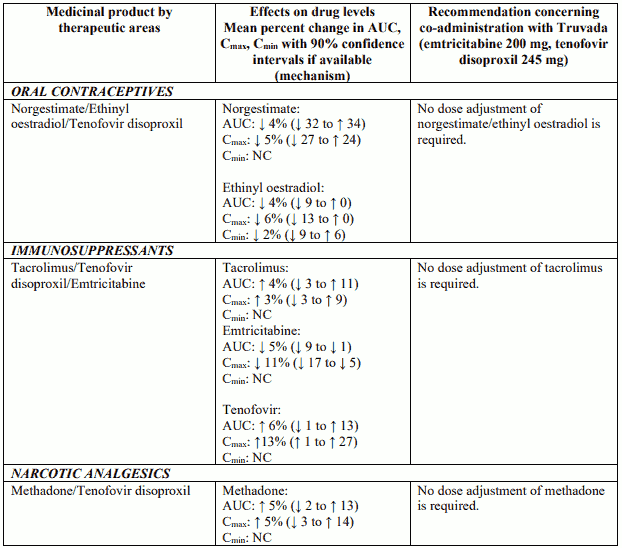
Interactions between Truvada or its individual component(s) and other medicinal products are listed in Table 2 below (increase is indicated as “↑”, decrease as “↓”, no change as “↔”, twice daily as “b.i.d.” and once daily as “q.d.”). If available, 90% confidence intervals are shown in parentheses.
Table 2: Interactions between Truvada or its individual component(s) and other medicinal products:
NC = not calculated.
N/A = not applicable.
1 Data generated from simultaneous dosing with ledipasvir/sofosbuvir. Staggered administration (12 hours apart) provided similar results.
2 The predominant circulating metabolite of sofosbuvir.
3 Study conducted with additional voxilaprevir 100 mg to achieve voxilaprevir exposures expected in HCV-infected patients.
4.6. Fertility, pregnancy and lactation
Pregnancy
A large amount of data on pregnant women (more than 1,000 pregnancy outcomes) indicate no malformations or foetal/neonatal toxicity associated with emtricitabine and tenofovir disoproxil. Animal studies on emtricitabine and tenofovir disoproxil do not indicate reproductive toxicity (see section 5.3). Therefore the use of Truvada may be considered during pregnancy, if necessary.
Breast-feeding
Emtricitabine and tenofovir have been shown to be excreted in human milk. There is insufficient information on the effects of emtricitabine and tenofovir in newborns/infants. Therefore Truvada should not be used during breast-feeding.
In order to avoid transmission of HIV to the infant it is recommended that women living with HIV do not breast-feed their infants.
Fertility
No human data on the effect of Truvada are available. Animal studies do not indicate harmful effects of emtricitabine or tenofovir disoproxil on fertility.
4.7. Effects on ability to drive and use machines
No studies on the effects on the ability to drive and use machines have been performed. However, individuals should be informed that dizziness has been reported during treatment with both emtricitabine and tenofovir disoproxil.
4.8. Undesirable effects
Summary of the safety profile
HIV-1 infection
The most frequently reported adverse reactions considered possibly or probably related to emtricitabine and/or tenofovir disoproxil were nausea (12%) and diarrhoea (7%) in an open-label randomised clinical study in adults (GS-01-934, see section 5.1). The safety profile of emtricitabine and tenofovir disoproxil in this study was consistent with the previous experience with these agents when each was administered with other antiretroviral agents.
Pre-exposure prophylaxis
No new adverse reactions to Truvada were identified from two randomised placebo-controlled studies (iPrEx, Partners PrEP) in which 2,830 HIV-1 uninfected adults received Truvada once daily for pre-exposure prophylaxis. Patients were followed for a median of 71 weeks and 87 weeks, respectively. The most frequent adverse reaction reported in the Truvada group in the iPrEx study was headache (1%).
Tabulated summary of adverse reactions
The adverse reactions considered at least possibly related to treatment with the components of Truvada from clinical study and post-marketing experience in HIV-1 infected patients are listed in Table 3, below, by body system organ class and frequency. Within each frequency grouping, undesirable effects are presented in order of decreasing seriousness. Frequencies are defined as very common (≥1/10), common (≥1/100 to <1/10), uncommon (≥1/1,000 to <1/100) or rare (≥1/10,000 to <1/1,000).
Table 3. Tabulated summary of adverse reactions associated with the individual components of Truvada based on clinical study and post-marketing experience:
| Frequency | Emtricitabine | Tenofovir disoproxil |
|---|---|---|
| Blood and lymphatic system disorders | ||
| Common: | neutropenia | |
| Uncommon: | anaemia2 | |
| Immune system disorders | ||
| Common: | allergic reaction | |
| Metabolism and nutrition disorders | ||
| Very common: | hypophosphataemia1 | |
| Common: | hyperglycaemia, hypertriglyceridaemia | |
| Uncommon: | hypokalaemia1 | |
| Rare: | lactic acidosis | |
| Psychiatric disorders | ||
| Common: | insomnia, abnormal dreams | |
| Nervous system disorders | ||
| Very common: | headache | dizziness |
| Common: | dizziness | headache |
| Gastrointestinal disorders | ||
| Very common: | diarrhoea, nausea | diarrhoea, vomiting, nausea |
| Common: | elevated amylase including elevated pancreatic amylase, elevated serum lipase, vomiting, abdominal pain, dyspepsia | abdominal pain, abdominal distension, flatulence |
| Uncommon: | pancreatitis | |
| Hepatobiliary disorders | ||
| Common: | elevated serum aspartate aminotransferase (AST) and/or elevated serum alanine aminotransferase (ALT), hyperbilirubinaemia | increased transaminases |
| Rare: | hepatic steatosis, hepatitis | |
| Skin and subcutaneous tissue disorders | ||
| Very common: | rash | |
| Common: | vesiculobullous rash, pustular rash, maculopapular rash, rash, pruritus, urticaria, skin discolouration (increased pigmentation)2 | |
| Uncommon: | angioedema3 | |
| Rare: | angioedema | |
| Musculoskeletal and connective tissue disorders | ||
| Very common: | elevated creatine kinase | |
| Uncommon: | rhabdomyolysis1, muscular weakness1 | |
| Rare: | osteomalacia (manifested as bone pain and infrequently contributing to fractures)1,3, myopathy1 | |
| Renal and urinary disorders | ||
| Uncommon: | increased creatinine, proteinuria, proximal renal tubulopathy including Fanconi syndrome | |
| Rare: | renal failure (acute and chronic), acute tubular necrosis, nephritis (including acute interstitial nephritis)3, nephrogenic diabetes insipidus | |
| General disorders and administration site conditions | ||
| Very common: | asthenia | |
| Common: | pain, asthenia | |
1 This adverse reaction may occur as a consequence of proximal renal tubulopathy. It is not considered to be causally associated with tenofovir disoproxil in the absence of this condition.
^26 Anaemia was common and skin discolouration (increased pigmentation) was very common when emtricitabine was administered to paediatric patients.
3 This adverse reaction was identified through post-marketing surveillance but not observed in randomised controlled clinical studies in adults or paediatric HIV clinical studies for emtricitabine or in randomised controlled clinical studies or the tenofovir disoproxil expanded access program for tenofovir disoproxil. The frequency category was estimated from a statistical calculation based on the total number of patients exposed to emtricitabine in randomised controlled clinical studies (n=1,563) or tenofovir disoproxil in randomised controlled clinical studies and the expanded access program (n=7,319).
Description of selected adverse reactions
Renal impairment
As Truvada may cause renal damage monitoring of renal function is recommended (see section 4.4). Proximal renal tubulopathy generally resolved or improved after tenofovir disoproxil discontinuation. However, in some HIV-1 infected patients, declines in creatinine clearance did not completely resolve despite tenofovir disoproxil discontinuation. Patients at risk of renal impairment (such as patients with baseline renal risk factors, advanced HIV disease, or patients receiving concomitant nephrotoxic medications) are at increased risk of experiencing incomplete recovery of renal function despite tenofovir disoproxil discontinuation (see section 4.4).
Lactic acidosis
Cases of lactic acidosis have been reported with tenofovir disoproxil alone or in combination with other antiretrovirals. Patients with predisposing factors such as patients with decompensated liver disease, or patients receiving concomitant medications known to induce lactic acidosis are at increased risk of experiencing severe lactic acidosis during tenofovir disoproxil treatment, including fatal outcomes.
Metabolic parameters
Weight and levels of blood lipids and glucose may increase during antiretroviral therapy (see section 4.4).
Immune Reactivation Syndrome
In HIV infected patients with severe immune deficiency at the time of initiation of CART, an inflammatory reaction to asymptomatic or residual opportunistic infections may arise. Autoimmune disorders (such as Graves' disease and autoimmune hepatitis) have also been reported; however, the reported time to onset is more variable and these events can occur many months after initiation of treatment (see section 4.4).
Osteonecrosis
Cases of osteonecrosis have been reported, particularly in patients with generally acknowledged risk factors, advanced HIV disease or long-term exposure to CART. The frequency of this is unknown (see section 4.4).
Paediatric population
Assessment of adverse reactions related to emtricitabine is based on experience in three paediatric studies (n=169) where treatment-naïve (n=123) and treatment-experienced (n=46) paediatric HIV infected patients aged 4 months to 18 years were treated with emtricitabine in combination with other antiretroviral agents. In addition to the adverse reactions reported in adults, anaemia (9.5%) and skin discolouration (31.8%) occurred more frequently in clinical trials in paediatric patients than in adults (see section 4.8, Tabulated summary of adverse reactions).
Assessment of adverse reactions related to tenofovir disoproxil is based on two randomised trials (studies GS-US 104-0321 and GS-US-104-0352) in 184 HIV-1 infected paediatric patients (aged 2 to <18 years) who received treatment with tenofovir disoproxil (n=93) or placebo/active comparator (n=91) in combination with other antiretroviral agents for 48 weeks (see section 5.1). The adverse reactions observed in paediatric patients who received treatment with tenofovir disoproxil were consistent with those observed in clinical studies of tenofovir disoproxil in adults (see section 4.8 Tabulated summary of adverse reactions and 5.1).
Reductions in BMD have been reported in paediatric patients. In HIV-1 infected adolescents (aged 12 to <18 years), the BMD Z-scores observed in subjects who received tenofovir disoproxil were lower than those observed in subjects who received placebo. In HIV-1 infected children (aged 2 to 15 years), the BMD Z-scores observed in subjects who switched to tenofovir disoproxil were lower than those observed in subjects who remained on their stavudine- or zidovudine-containing regimen (see sections 4.4 and 5.1).
In study GS-US-104-0352, 89 HIV-1 infected paediatric patients with a median age of 7 years (range 2 to 15 years) were exposed to tenofovir disoproxil for a median of 331 weeks. Eight of the 89 patients (9.0%) discontinued study drug due to renal adverse events. Five subjects (5.6%) had laboratory findings clinically consistent with proximal renal tubulopathy, 4 of whom discontinued tenofovir disoproxil therapy. Seven patients had estimated glomerular filtration rate (GFR) values between 70 and 90 mL/min/1.73 m². Among them, 3 patients experienced a clinically meaningful decline in estimated GFR during therapy which improved after discontinuation of tenofovir disoproxil.
Other special populations
Individuals with renal impairment
Since tenofovir disoproxil can cause renal toxicity, close monitoring of renal function is recommended in any adults with renal impairment receiving Truvada (see sections 4.2, 4.4 and 5.2). The use of Truvada is not recommended in individuals under the age of 18 years with renal impairment (see sections 4.2 and 4.4).
HIV/HBV or HCV co-infected patients
The adverse reaction profile of emtricitabine and tenofovir disoproxil in a limited number of HIV-infected patients in study GS-01-934 who were co-infected with HBV (n=13) or HCV (n=26) was similar to that observed in patients infected with HIV without co-infection. However, as would be expected in this patient population, elevations in AST and ALT occurred more frequently than in the general HIV infected population.
Exacerbations of hepatitis after discontinuation of treatment
In HBV infected patients, clinical and laboratory evidence of hepatitis have occurred after discontinuation of treatment (see section 4.4).
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the national reporting system listed in Appendix V.
6.2. Incompatibilities
Not applicable.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.