VIVIMUSTA Solution for injection Ref.[109370] Active ingredients: Bendamustine
Source: FDA, National Drug Code (US) Revision Year: 2022
12.1. Mechanism of Action
Bendamustine is a bifunctional mechlorethamine derivative containing a purine-like benzimidazole ring. Mechlorethamine and its derivatives form electrophilic alkyl groups. These groups form covalent bonds with electron-rich nucleophilic moieties, resulting in interstrand DNA crosslinks. The bifunctional covalent linkage can lead to cell death via several pathways. Bendamustine is active against both quiescent and dividing cells. The exact mechanism of action of bendamustine remains unknown.
12.2. Pharmacodynamics
Based on the pharmacokinetics/pharmacodynamics analyses of data from adult patients with NHL, nausea increased with increasing bendamustine maximum concentrations (Cmax).
Cardiac Electrophysiology
The effect of bendamustine on the QTc interval was evaluated in 53 patients with indolent NHL and mantle cell lymphoma on Day 1 of Cycle 1 after administration of rituximab at 375 mg/m2 intravenous infusion followed by a 30-minute intravenous infusion of bendamustine at 90 mg/m2/day. No mean changes greater than 20 milliseconds were detected up to one hour post infusion. The potential for delayed effects on the QT interval after one hour was not evaluated.
12.3. Pharmacokinetics
Absorption
Following a single IV dose of bendamustine hydrochloride Cmax typically occurred at the end of infusion. The dose proportionality of bendamustine has not been studied.
Distribution
The protein binding of bendamustine ranged from 94-96% and was concentration independent from 1 to 50 μg/mL. The blood to plasma concentration ratios in human blood ranged from 0.84 to 0.86 over a concentration range of 10 to 100 μg/mL.
The mean steady-state volume of distribution (Vss) of bendamustine was approximately 20 to 25 L.
Elimination
After a single intravenous dose of 120 mg/m2 of bendamustine over 1 hour, the intermediate half-life (t½) of the parent compound was approximately 40 minutes. The mean terminal elimination t½ of two active metabolites, γ-hydroxybendamustine (M3) and N desmethylbendamustine (M4) were approximately 3 hours and 30 minutes, respectively. Bendamustine clearance in humans was approximately 700 mL/min.
Metabolism
Bendamustine is extensively metabolized via hydrolytic, oxidative, and conjugative pathways. Bendamustine is primarily metabolized via hydrolysis to monohydroxy (HP1) and dihydroxy-bendamustine (HP2) metabolites with low cytotoxic activity in vitro. Two active minor metabolites, M3 and M4, are primarily formed via CYP1A2 in vitro. M3 and M4 concentrations of these metabolites in plasma are 1/10th and 1/100th that of the parent compound, respectively.
Excretion
Following intravenous infusion of radiolabeled bendamustine hydrochloride in patients with cancer, approximately 76% of the dose was recovered. Approximately 50% of the dose was recovered in the urine (3.3% unchanged) and approximately 25% of the dose was recovered in the feces. Less than 1% of the dose was recovered in the urine as M3 and M4, and less than 5% of the dose was recovered in the urine as HP2.
Specific Populations
No clinically meaningful effects on the pharmacokinetics of bendamustine were observed based on age (31 to 84 years), sex, mild to moderate renal impairment (CLcr ≥ 30 mL/min), or hepatic impairment with total bilirubin 1.5 < ULN and AST or ALT < 2.5 × ULN. The effects of severe renal impairment (CLcr < 30 mL/min), or hepatic impairment with total bilirubin 1.5 to 3 × ULN and AST or ALT 2.5 to 10 × ULN or total bilirubin > 3 × ULN on the pharmacokinetics of bendamustine is unknown.
Race/Ethnicity
Exposures in Japanese subjects (n=6) were 40% higher than non-Japanese subjects receiving the same dose. The clinical importance of this difference on the safety and efficacy of bendamustine hydrochloride in Japanese subjects has not been established.
Drug Interaction Studies
In Vitro Studies
Effect of Bendamustine Hydrochloride on CYP Substrates: Bendamustine hydrochloride did not inhibit CYP1A2, 2C9/10, 2D6, 2E1, or 3A4/5. Bendamustine hydrochloride did not induce metabolism of CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2E1, or CYP3A4/5.
Effect of Transporters on Bendamustine Hydrochloride: Bendamustine hydrochloride is a substrate of P-glycoprotein and breast cancer resistance protein (BCRP).
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Bendamustine was carcinogenic in mice. After intraperitoneal injections at 37.5 mg/m2/day (the lowest dose tested, approximately 0.3 times the maximum recommended human dose [MRHD]) and 75 mg/m2/day (approximately 0.6 times the MRHD) for 4 days, peritoneal sarcomas in female AB/jena mice were produced. Oral administration at 187.5 mg/m2/day (the only dose tested, approximately 1.6 times the MRHD) for 4 days induced mammary carcinomas and pulmonary adenomas.
Bendamustine is a mutagen and clastogen. In a reverse bacterial mutation assay (Ames assay), bendamustine was shown to increase revertant frequency in the absence and presence of metabolic activation. Bendamustine was clastogenic in human lymphocytes in vitro, and in rat bone marrow cells in vivo (increase in micronucleated polychromatic erythrocytes) from 37.5 mg/m2, (the lowest dose tested, approximately 0.3 times the MRHD).
Bendamustine induced morphologic abnormalities in spermatozoa in mice. Following tail vein injection of bendamustine at 120 mg/m2 or a saline control on days 1 and 2 for a total of three weeks, the number of spermatozoa with morphologic abnormalities was 16% higher in the bendamustine-treated group as compared to the saline control group.
14. Clinical Studies
14.1 Chronic Lymphocytic Leukemia (CLL)
The efficacy of bendamustine hydrochloride was evaluated in an open-label, randomized, controlled multicenter trial comparing bendamustine hydrochloride to chlorambucil. The trial was conducted in 301 previously-untreated patients with Binet Stage B or C (Rai Stages I-IV) CLL requiring treatment. Need-to-treat criteria included hematopoietic insufficiency, B-symptoms, rapidly progressive disease or risk of complications from bulky lymphadenopathy. Patients with autoimmune hemolytic anemia or autoimmune thrombocytopenia, Richter’s syndrome, or transformation to prolymphocytic leukemia were excluded from the study. Patients were randomly assigned to receive either bendamustine hydrochloride 100 mg/m 2 intravenously over 30 minutes on Days 1 and 2 of each 28-day cycle or chlorambucil 0.8 mg/kg (Broca’s normal weight) orally on Days 1 and 15 of each 28-day cycle.
The patient populations in the bendamustine hydrochloride and chlorambucil treatment groups were balanced with regard to the following baseline characteristics: age (median 63 vs. 66 years), sex (63% vs. 61% male), Binet stage (71% vs. 69% Binet B), lymphadenopathy (79% vs. 82%), enlarged spleen (76% vs. 80%), enlarged liver (48% vs. 46%), hypercellular bone marrow (79% vs. 73%), “B” symptoms (51% vs. 53%), lymphocyte count (mean 65.7 × 109/L vs. 65.1 × 109/L), and serum lactate dehydrogenase concentration (mean 370.2 vs. 388.4 U/L). Ninety percent of patients in both treatment groups had immuno-phenotypic confirmation of CLL (CD5, CD23 and either CD19 or CD20 or both).
Efficacy endpoints of objective response rate and progression-free survival were calculated using a pre-specified algorithm based on NCI working group criteria for CLL. The results of this open-label randomized study demonstrated a higher rate of overall response and a longer progression-free survival for bendamustine hydrochloride compared to chlorambucil (see Table 6). Survival data are not mature.
Table 6. Efficacy Data for CLL:
| Bendamustine Hydrochloride (N=153) | Chlorambucil (N=148) | p-value | |
| Response Rate n (%) | |||
| Overall response rate | 90 (59) | 38 (26) | <0.0001 |
| (95% CI) | (51, 66.6) | (18.6, 32.7) | |
| Complete response (CR)* | 13 (8) | 1 (<1) | |
| Nodular partial response (nPR)** | 4 (3) | 0 | |
| Partial response (PR) † | 73 (48) | 37 (25) | |
| Progression-Free Survival†† | |||
| Median, months (95% CI) | 18 (11.7, 23.5) | 6 (5.6, 8.6) | |
| Hazard ratio (95% CI) | 0.27 (0.17, 0.43) | <0.0001 | |
CI = confidence interval
* CR was defined as peripheral lymphocyte count ≤ 4 × 109/L, neutrophils ≥ 1.5 × 109/L, platelets >100 × 109/L, hemoglobin >110 g/L, without transfusions, absence of palpable hepatosplenomegaly, lymph nodes ≤ 1.5 cm, < 30% lymphocytes without nodularity in at least a normocellular bone marrow and absence of “B” symptoms. The clinical and laboratory criteria were required to be maintained for a period of at least 56 days.
** nPR was defined as described for CR with the exception that the bone marrow biopsy shows persistent nodules.
† PR was defined as ≥50% decrease in peripheral lymphocyte count from the pre-treatment baseline value, and either ≥50% reduction in lymphadenopathy, or ≥50% reduction in the size of spleen or liver, as well as one of the following hematologic improvements: neutrophils ≥1.5 × 109/L or 50% improvement over baseline, platelets >100 × 109/L or 50% improvement over baseline, hemoglobin >110 g/L or 50% improvement over baseline without transfusions, for a period of at least 56 days.
†† PFS was defined as time from randomization to progression or death from any cause.
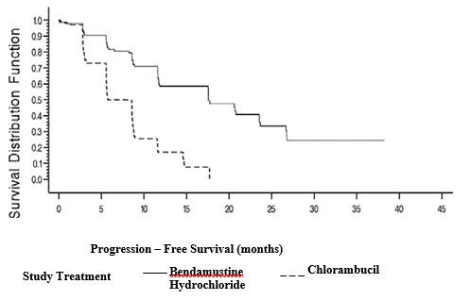
Kaplan-Meier estimates of progression-free survival comparing bendamustine hydrochloride with chlorambucil are shown in Figure 1.
Figure 1. Progression-Free Survival
14.2 Non-Hodgkin Lymphoma (NHL)
The efficacy of bendamustine hydrochloride was evaluated in a single arm study of 100 patients with indolent B-cell NHL that had progressed during or within six months of treatment with rituximab or a rituximab-containing regimen. Patients were included if they relapsed within 6 months of either the first dose (monotherapy) or last dose (maintenance regimen or combination therapy) of rituximab. All patients received bendamustine hydrochloride 120 mg/m2 intravenously on Days 1 and 2 of a 21-day treatment cycle for up to 8 cycles.
The median age was 60 years, 65% were male, and 95% had a baseline WHO performance status of 0 or 1. Major tumor subtypes were follicular lymphoma (62%), diffuse small lymphocytic lymphoma (21%), and marginal zone lymphoma (16%). Ninety-nine percent of patients had received previous chemotherapy, 91% of patients had received previous alkylator therapy, and 97% of patients had relapsed within 6 months of either the first dose (monotherapy) or last dose (maintenance regimen or combination therapy) of rituximab.
Efficacy was based on the assessments by a blinded independent review committee (IRC) and included overall response rate (complete response + complete response unconfirmed + partial response) and duration of response (DR) as summarized in Table 7.
Table 7. Efficacy Data for NHL*:
| Bendamustine Hydrochloride (N=100) | |
| Response Rate (%) | |
| Overall response rate (CR+CRu+PR) | 74 |
| (95% CI) | (64.3, 82.3) |
| Complete response (CR) | 13 |
| Complete response unconfirmed (CRu) | 4 |
| Partial response (PR) | 57 |
| Duration of Response (DR) | |
| Median, months (95% CI) | 9.2 months (7.1, 10.8) |
CI = confidence interval
* IRC assessment was based on modified International Working Group response criteria (IWG-RC). Modifications to IWG-RC specified that a persistently positive bone marrow in patients who met all other criteria for CR would be scored as PR. Bone marrow sample lengths were not required to be ≥20 mm.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.