VOXZOGO Powder and solvent for solution for injection Ref.[49897] Active ingredients: Vosoritide
Source: European Medicines Agency (EU) Revision Year: 2024 Publisher: BioMarin International Limited, Shanbally, Ringaskiddy, County Cork, P43 R298, Ireland
5.1. Pharmacodynamic properties
Pharmacotherapeutic group: Drugs for treatment of bone diseases, Other drugs affecting bone structure and mineralisation
ATC code: M05BX07
Mechanism of action
Vosoritide is a modified type C natriuretic peptide (CNP). In patients with achondroplasia, endochondral bone growth is negatively regulated due to a gain of function mutation in fibroblast growth factor receptor 3 (FGFR3). Binding of vosoritide to natriuretic peptide receptor-B (NPR-B) antagonises FGFR3 downstream signalling by inhibiting the extracellular signal-regulated kinases 1 and 2 (ERK1/2) in the mitogen-activated protein kinase (MAPK) pathway at the level of rapidly accelerating fibrosarcoma serine/threonine protein kinase (RAF-1). As a result, vosoritide, like CNP, acts as a positive regulator of endochondral bone growth as it promotes chondrocyte proliferation and differentiation.
Pharmacodynamic effects
Exposure-dependent (AUC and Cmax) increases from baseline in urinary cyclic guanosine monophosphate (cGMP, a biomarker for NPR-B activity) concentrations and serum collagen type X marker (CXM, a biomarker for endochondral ossification) were observed on treatment with vosoritide. Increase in the urinary cGMP concentrations from pre-dose baseline took place within the first four hours post-dose. Median serum CXM concentration increased over baseline by day 29 of daily administration of this medicinal product. This effect was maintained beyond 24 months of treatment. Vosoritide activity as measured by urine cGMP was near saturation while maximal increase in growth plate activity indicated by CXM was achieved at the dose of 15 μg/kg administered subcutaneously once daily.
Clinical efficacy and safety
The efficacy and safety of vosoritide in patients with achondroplasia with confirmed FGFR3 mutation were assessed in a randomised, double-blind, placebo-controlled 52-week study (ACH study 111-301). In ACH study 111-301, patients were randomised to either vosoritide (n=60) or placebo (n=61) and the dose of vosoritide was 15 μg/kg administered subcutaneously once daily. Prior to randomisation, all patients enrolled in an observational study (ACH study 111-901) for paediatric patients with achondroplasia for at least a 6-month period during which baseline standing height and other pre-treatment growth assessments were collected. Patients with limb-lengthening surgery in the prior 18 months or who planned to have limb-lengthening surgery during the study period were excluded. The study comprised a 52-week placebo-controlled treatment phase followed by an open-label treatment extension study in which all patients received vosoritide. The primary efficacy endpoint was the change from baseline in AGV at Week 52 compared with placebo.
Patients with achondroplasia were also treated with vosoritide 15 μg/kg/day in an open label, dose-escalation study and in its long-term extension study (ACH study 111-205). Data was collected from observational studies in patients to characterise the natural history of achondroplasia. Height data from untreated patients with achondroplasia in the same age range as the clinical studies was used as an historical control to assess the effect on height after up to 5 years of vosoritide treatment.
Patient demographics and baseline characteristics are shown in Table 3.
Table 3. Patient demographics and characteristics in ACH study 111-301 and ACH study 111-205:
| Parameter | ACH study 111-301 | ACH study 111-205b | |
|---|---|---|---|
| Placebo (N=61) | 15 μg/kg/day Voxzogo (N=60) | 15 μg/kg/day Voxzogo (N=10) | |
| Age at day 1 (years) | |||
| Mean (SD) | 9.06 (2.47) | 8.35 (2.43) | 8.54 (1.54) |
| Min, max | 5.1; 14.9 | 5.1; 13.1 | 6.3; 11.1 |
| Age at day 1, n (%)a | |||
| ≥5 to <8 years | 24 (39.3) | 31 (51.7) | 4 (40.0) |
| ≥8 to <11 years | 24 (39.3) | 17 (28.3) | 5 (50.0) |
| ≥11 to <15 years | 13 (21.3) | 12 (20.0) | 1 (10.0) |
| Tanner stage b, n (%)a | |||
| I | 48 (78.7) | 48 (80.0) | 10 (100.0) |
| > I | 13 (21.3) | 12 (20.0) | |
| Sex, n (%)a | |||
| Male | 33 (54.1) | 31 (51.7) | 4 (40.0) |
| Female | 28 (45.9) | 29 (48.3) | 6 (60.0) |
| Weight (kg) | |||
| Mean (SD) | 24.62 (9.07) | 22.88 (7.96) | 25.13 (5.74) |
| Min, max | 11.6; 68.9 | 13.6; 53.0 | 18.2; 36.4 |
max, maximum; min, minimum; SD, standard deviation.
a Percentages were calculated using the total number of patients in the full analysis set (N for each treatment group) as the denominator.
b Analysis from 10 out of 35 patients who only received 15 μg/kg/day in an open label, dose-escalation study and continued into the long-term extension ACH study 111-205.
In ACH study 111-301, improvements in AGV and height Z-score from baseline were observed in patients treated with Voxzogo 15 µg/kg/day compared with placebo. Efficacy results are shown in Table 4.
Table 4. Results from placebo-controlled clinical trial:
| Placebo (N=61) | Voxzogo 15 µg/kg daily (N=60c) | Voxzogo vs. placebo | |||||
|---|---|---|---|---|---|---|---|
| Baseline | Week 52 | Change | Baseline | Week 52 | Change | LS Mean difference in changes (95% CI) | |
| Annualised growth velocity (cm/year) | |||||||
| Mean ± SD | 4.06 ± 1.20 | 3.94 ± 1.07 | -0.12 ± 1.74 | 4.26 ± 1.53 | 5.61 ± 1.05 | 1.35 ± 1.71 | 1.57a (1.22; 1.93) (p = <0.0001)b |
| Height Z-score | |||||||
| Mean ± SD | -5.14 ± 1.07 | -5.14 ± 1.09 | 0.00 ± 0.28 | -5.13 ± 1.11 | -4.89 ± 1.09 | 0.24 ± 0.32 | 0.28a (0.17; 0.39) (p = <0.0001)b |
AGV, annualised growth velocity; 95% CI, 95% confidence interval; LS, least-square; SD, standard deviation.
a Difference is 15 µg/kg Voxzogo minus placebo.
b Two-sided p-value. c Two patients in the Voxzogo group discontinued from the study before Week 52. The values for these 2 patients were imputed for this analysis.
LS mean estimated from the ANCOVA (analysis of covariance) model adjusted for baseline differences between the two arms, analysis of covariance.
The benefit of improvement in AGV in favour of Voxzogo was consistent across all predefined subgroups analysed including sex, age group, Tanner stage, baseline height Z-score, and baseline AGV. In the subgroup of males Tanner stage > I, the point estimate of treatment effect was in favour of vosoritide however there were only 8 subjects in this subgroup (3 and 5 subjects in vosoritide and placebo arms, respectively).
The observed increase in growth occurred proportionally in both the spine and the lower limbs. There was no difference in bone mineral density after treatment with Voxzogo compared to placebo. During treatment with this medicinal product, the mean increase in bone age was comparable to the mean increase in chronological age, indicating no acceleration of bone maturation.
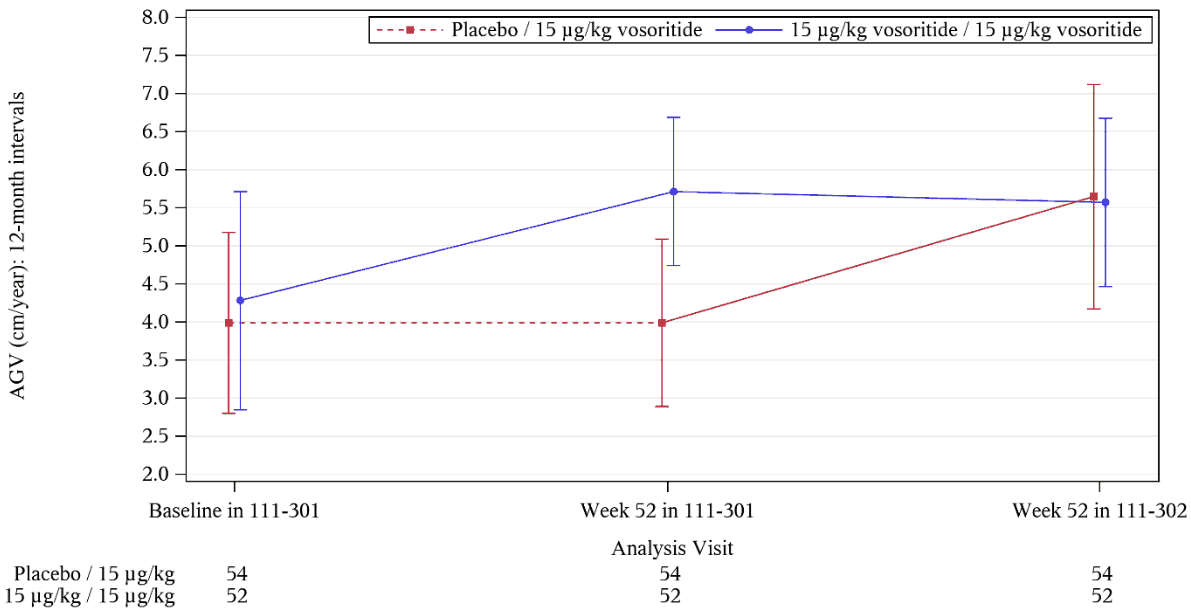
Figure 1 shows the effect of Voxzogo over the two-year period in the Voxzogo treatment group, as well as the effect in the placebo control group after receiving daily subcutaneous injections of Voxzogo for 52 weeks in the open label extension study. Improvements in AGV were maintained during continued Voxzogo therapy, with no evidence of tachyphylaxis.
Figure 1. Mean (±SD) 12-Month Interval AGV Over Time:
The figure includes all subjects enrolled in the pivotal trial who had a height assessment at week 52 in the extension study. Solid lines represent treatment with vosoritide 15 ug/kg; dashed lines represent placebo. Baseline is defined as the last assessment before the first dose of active study drug (i.e. vosoritide) or Placebo in 111-301.
12-Month AGV at post-baseline visits is derived over the previous 12 months. For example, 12-Month Interval AGV at Week 52 111-302 = [(Height at Week 52 111-302 Visit- Height at Week 52 111-301 Visit)/(Date of Week 52 111-302 Visit - Date of Week 52 111-301 Visit)] x 365.25.
Open-label extension study
In the long-term extension study (ACH study 111-205), 10 patients were treated with Voxzogo 15 µg/kg/day dose continuously for up to 5 years. The mean (SD) improvement in AGV compared to baseline at 60 months was 1.34 (1.31) cm/year.
The gain in height after 5 years of treatment with 15 µg/kg/day of Voxzogo was compared with an age and sex matched historical control. The 5-year cross-sectional comparative analysis adjusted for baseline height differences, demonstrated, there was a statistically significant mean (95% CI) difference in height in favour of Voxzogo (9.08 [5.77, 12.38] cm; p=0.0002) compared with untreated patients with achondroplasia.
Paediatric population <5 years
A total of 75 patients aged 4.4 months to 59.8 months at day 1 of dosing were enrolled in a randomized, double-blind, placebo-controlled 52-week study. At least 6 months of baseline growth data were collected in the observational study for patients who were aged 6 months and over at randomization, and at least 3-months baseline data for those subjects aged under 6 months at randomization. A total of 64 patients were randomised to receive vosoritide treatment or placebo and 11 patients received open-label treatment. At 52 weeks, patients treated with vosoritide had an improvement in Height Z-score +0.30 SDS (95% CI 0.07, 0.54) compared to placebo.
Nine children aged >24 to <60 months were treated with vosoritide for 3 years and showed an improvement in Height Z-score of + 1.22 SDS (95% CI 0.78, 1.66) and a LS mean difference in height of 5.73 cm (95% CI 3.54, 7.93) compared with an age and sex matched historical control of untreated patients with achondroplasia.
Eleven children aged >6 to <24 months were treated with vosoritide for 2 years and showed an improvement in Height Z-score of + 0.79 SDS (95% CI 0.29, 1.28) and a LS mean difference in height of 2.69 cm (95% CI 1.00, 4.38) compared with an age and sex matched historical control of untreated patients with achondroplasia.
5.2. Pharmacokinetic properties
Vosoritide is a modified recombinant human CNP. The 39 amino acid peptide analogue includes the 37 C terminal amino acids of the human CNP53 sequence plus the addition of 2 amino acids (Pro Gly) to convey resistant to neutral endopeptidase (NEP) degradation, resulting in prolonged half-life in comparison to endogenous CNP.
The pharmacokinetics of vosoritide were evaluated in a total of 58 patients aged 5 to 18 years with achondroplasia who received subcutaneous injections of vosoritide 15 μg/kg once daily for 52 weeks. The pharmacokinetic exposure of vosoritide in 15 patients aged 2 to <5 years old were comparable with older children.
In 8 patients aged 6 months to <2 years old, receiving 30 μg/kg once daily the pharmacokinetic exposure of vosoritide was 65% to 70% higher than the older children (>2 years old) receiving 15 μg/kg once daily. In 9 patients <6 months of age receiving 30 μg/kg once daily, the pharmacokinetic exposure of vosoritide was 57% to 105% higher than the older children (>2 years old) receiving 15 μg/kg once daily.
Absorption
Vosoritide was absorbed with a median Tmax of 15 minutes. The mean (± SD) peak concentration (Cmax) and area under the concentration-time curve from time zero to the last measurable concentration (AUC0-t) observed after 52 weeks of treatment was 5 800 (±3 680), and 290 000 (± 235 000) pg-min/mL respectively. The bioavailability of vosoritide was not assessed in clinical studies.
Distribution The mean (± SD) apparent volume of distribution after 52 weeks of treatment was 2 910 (± 1 660) mL/kg.
Biotransformation
The metabolism of vosoritide is expected to occur via catabolic pathways and be degraded into small peptide fragments and amino acids.
Elimination
The mean (± SD) apparent clearance after 52 weeks of treatment was 79.4 (53.0) mL/min/kg. The mean (± SD) half-life was 27.9 (9.9) minutes.
The inter-subject variability (coefficient of variation) in apparent clearance was 33.6%.
Linearity/non-linearity
The increase in plasma exposure (AUC and Cmax) with dose was greater than dose proportional across the dose range of 2.5 (0.17 times the recommended dose) to 30.0 μg/kg/day (twice the approved dose).
Special populations
No clinically significant differences in the vosoritide pharmacokinetics was observed based on age (0.9 to 16 years), sex, race or ethnicity.
Body weight
Body weight is the only significant covariate for vosoritide clearance or volume of distribution. The apparent clearance and volume of distribution of vosoritide increased with increasing body weight in patients with achondroplasia (9 to 74.5 kg). The proposed posology (see section 4.2) takes account of this deviation and recommends the use of doses above (in patients between 10 and 16 kg body weight), or below (in those above a body weight of 44 kg) the 15 μg/kg "standard dose" in order to enable a similar level of exposure across all weight-ranges.
Patients with renal and hepatic impairment
The safety and efficacy of vosoritide in patients with renal or hepatic impairment has not been evaluated. Based on the elimination mechanism, renal or hepatic impairment is not expected to alter the pharmacokinetics of vosoritide.
Drug interaction studies
In vitro cytochrome P450 (CYP) inhibition and induction studies indicated that vosoritide did not inhibit CYP 1A2, 2B6, 2C8, 2C9, 2C19, 2D6, or 3A4/5, nor induce CYP 1A2, 2B6, or 3A4/5 at clinically relevant concentrations. In vitro interaction studies also indicated that the potential for interaction with the drug-transporters OAT1, OAT3, OCT 1, OCT 2, OATP1B1, OATP1B3, MATE 1, KATE2-K, BCRP, P-gp, and BSEP is low at clinically relevant concentrations.
5.3. Preclinical safety data
Adverse reactions not observed in clinical studies but seen in animals at exposure levels similar to clinical exposure levels, and with possible relevance to clinical use.
Transient decreases in blood pressure and increases in heart rate were observed in healthy monkeys across multiple studies in doses of 28 to 300 μg/kg in a dose-related manner. Peak effects were typically observed within the first hour post dose and were generally asymptomatic. In some monkeys receiving higher doses of vosoritide, brief bouts of sternal/lateral recumbency or hypoactivity, were observed. These effects could be related to decreased blood pressure.
Adverse effects on body posture, bone shape, mobility, and bone strength were observed in normal animals in repeat-dose toxicity studies in rats and monkeys. In monkeys, the NOAEL for vosoritide is 25 μg/kg (mean Cmax value of 1 170 pg/mL; approximately equivalent to the recommended human dose in a 20 kg human) when administered daily via subcutaneous injection for 44 weeks.
Carcinogenicity/mutagenicity
Carcinogenicity and genotoxicity studies have not been performed with vosoritide. Based on the mechanism of action, vosoritide is not expected to be tumorigenic.
Impairment of fertility
In a fertility and reproductive study in male and female rats at dose levels up to 540 μg/kg/day, vosoritide had no effect on mating performance, fertility, or litter characteristics.
Reproductive and developmental toxicity
Vosoritide was not associated with effects on reproductive performance, in utero or developmental parameters measured in rats and rabbits to investigate fertility, or embryo-foetal development in pre- and post-natal development studies.
Vosoritide was detected in the breast milk in rats.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.