VYEPTI Solution for injection Ref.[10282] Active ingredients: Eptinezumab
Source: FDA, National Drug Code (US) Revision Year: 2020
12.1. Mechanism of Action
Eptinezumab-jjmr is a humanized monoclonal antibody that binds to calcitonin gene-related peptide (CGRP) ligand and blocks its binding to the receptor.
12.2. Pharmacodynamics
The relationship between the pharmacodynamic activity and the mechanism(s) by which eptinezumab-jjmr exerts its clinical effects is unknown.
12.3. Pharmacokinetics
Eptinezumab-jjmr exhibits linear pharmacokinetics and exposure increases proportionally with doses from 100 mg to 300 mg after intravenous administration. Steady-state plasma concentration is attained after the first dose with a once every 3-month dosing schedule.
Distribution
The central volume of distribution (Vc) for eptinezumab-jjmr is approximately 3.7 liters.
Metabolism & Elimination
Eptinezumab-jjmr is expected to be degraded by proteolytic enzymes into small peptides and amino acids.
The apparent clearance of eptinezumab-jjmr was 0.006 L/h, and the terminal elimination half-life was approximately 27 days.
Specific Populations
A population pharmacokinetic analysis assessing the effects of age, race, sex, and body weight did not suggest any clinically significant impact of these covariates on eptinezumab exposures.
Patients with Renal or Hepatic Impairment
No dedicated studies were conducted to assess the effects of renal or hepatic impairment on the pharmacokinetics of eptinezumab-jjmr. However, hepatic or renal impairment is not expected to affect the pharmacokinetics of eptinezumab-jjmr. A population pharmacokinetic analysis of integrated data from eptinezumab-jjmr clinical studies did not reveal clinically significant impact on pharmacokinetics of patients with hepatic or renal impairment.
Drug Interaction Studies
P450 Enzymes
Eptinezumab-jjmr is not metabolized by cytochrome P450 enzymes; therefore, interactions with concomitant medications that are substrates, inducers, or inhibitors of cytochrome P450 enzymes are unlikely.
Sumatriptan
The co-administration of a single dose of 300 mg eptinezumab-jjmr administered as an intravenous infusion (over a period of 1 hour ± 15 min) with a single dose of 6 mg sumatriptan administered subcutaneously did not significantly influence the pharmacokinetics of eptinezumab-jjmr or sumatriptan.
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
The carcinogenic potential of eptinezumab-jjmr has not been assessed.
Mutagenesis
Genetic toxicology studies of eptinezumab-jjmr have not been conducted.
Impairment of Fertility
When eptinezumab-jjmr (0, 75, or 150 mg/kg) was administered weekly by intravenous injection to male and female rats prior to and during mating and continuing in females to gestation day 3-4, no adverse effects on fertility were observed. The higher dose tested (150 mg/kg) is 30 times the maximum recommended human dose of 300 mg, on a body weight basis (mg/kg).
14. Clinical Studies
The efficacy of VYEPTI was evaluated as a preventive treatment of episodic and chronic migraine in two randomized, multicenter, placebo-controlled studies, both with 6-month double-blind periods: one study in patients with episodic migraine (Study 1) and one study in patients with chronic migraine (Study 2). VYEPTI was administered by intravenous infusion every 3 months in both studies; however, the primary endpoint was measured at 12 weeks.
Study 1: Episodic Migraine
Study 1 (NCT02559895) included adults with a history of episodic migraine (4 to 14 headache days per month, of which at least 4 were migraine days). A total of 665 patients were randomized to receive placebo (N=222), 100 mg VYEPTI (N=221), or 300 mg VYEPTI (N=222) every 3 months for 12 months. Patients were allowed to use concurrent acute migraine or headache medications, including migraine-specific medications (i.e., triptans, ergotamine derivatives), during the trial.
The study excluded patients with a history of cardiovascular disease (hypertension, ischemic heart disease), neurological disease, or cerebrovascular disease.
The primary efficacy endpoint was the change from baseline in mean monthly migraine days over Months 1-3. Secondary endpoints included the percentages of patients with 50% or greater, and 75% or greater reductions from baseline in monthly migraine days over Months 1-3.
Patients had a median age of 39 years (range: 18 to 71 years), 84% were female, and 84% were white. The mean migraine frequency at baseline was approximately 8.6 migraine days per month and was similar across treatment groups.
VYEPTI treatment demonstrated statistically significant improvements compared to placebo for the primary efficacy endpoint, as shown in Table 2; secondary endpoints are also summarized in Table 2.
Table 2. Efficacy Endpoint Results in Study 1:
| VYEPTI 100 mg N=221 | VYEPTI 300 mg N=222 | Placebo N=222 | |
|---|---|---|---|
| Monthly Migraine Days (MMD) – Months 1-3 | |||
| Change from baseline | -3.9 | -4.3 | -3.2 |
| Difference from placebo | -0.7 | -1.1 | |
| p-value | 0.018 | <0.001 | |
| ≥50% MMD responders – Months 1-3 | |||
| % Responders | 49.8% | 56.3% | 37.4% |
| Difference from placebo | 12.4% | 18.9% | |
| p-value | 0.009* | <0.001 | |
| ≥75% MMD responders – Months 1-3 | |||
| % Responders | 22.2% | 29.7% | 16.2% |
| Difference from placebo | 6.0% | 13.5% | |
| p-value | NS** | <0.001 | |
* Nominal statistical significance
** NS = Not statistically significant
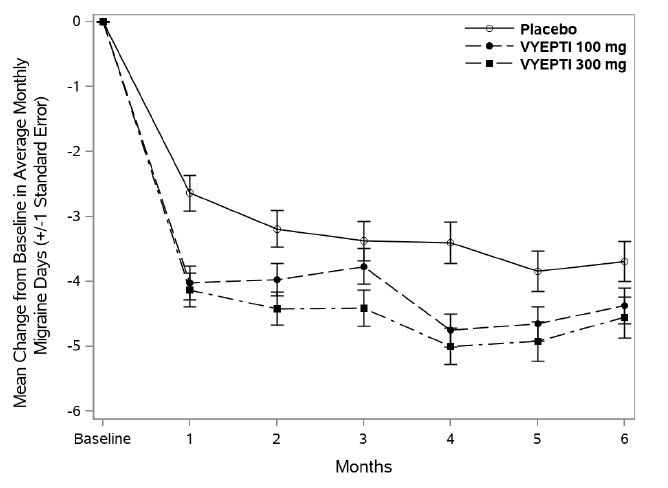
Figure 1 shows the mean change from baseline in average monthly migraine days in Study 1. Patients treated with VYEPTI at both doses had greater mean decreases from baseline in mean monthly migraine days over Months 1-3 compared to placebo-treated patients.
Figure 1. Change from Baseline in Monthly Migraine Days in Study 1:
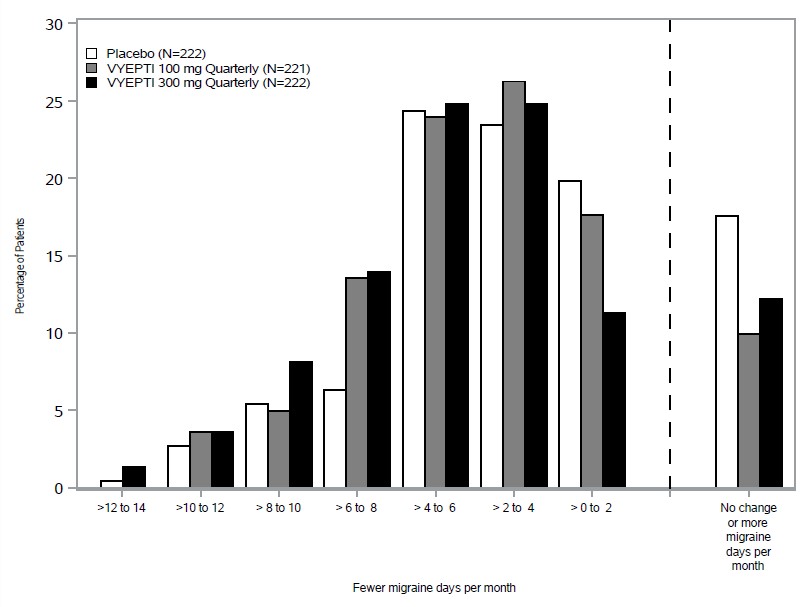
Figure 2 shows the distribution of change from baseline in mean monthly migraine days through Month 3 by treatment group in 2-day increments.
Figure 2. Distribution of Change from Baseline in Mean Monthly Migraine Days over Months 1 to 3 by Treatment Group in Study 1:
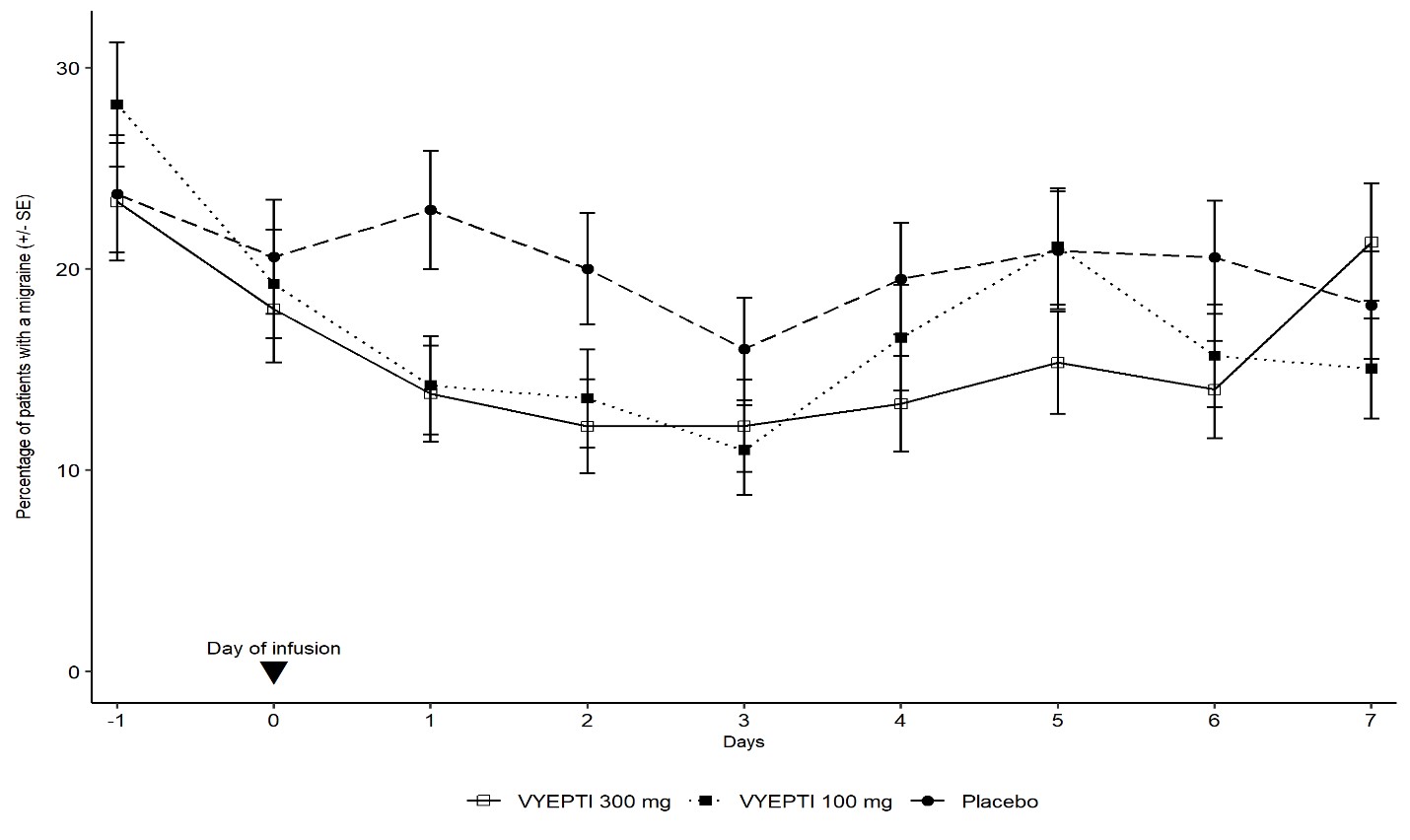
Figure 3 demonstrates that greater percentages of placebo-treated patients had migraines on most days during the first 7 days of treatment compared to VYEPTI-treated patients in Study 1.
Figure 3. Percentage of Patients with a Migraine from Day -1 (Day Prior to Infusion) to Day 7 in Study 1:
Study 2: Chronic Migraine
Study 2 (NCT02974153) included adults with a history of chronic migraine (15 to 26 headache days per month, of which at least 8 were migraine days). A total of 1072 patients were randomized and received placebo (N=366), 100 mg VYEPTI (N=356), or 300 mg VYEPTI (N=350) every 3 months for 6 months. Patients were allowed to use and to continue an established stable regimen of acute migraine or headache preventive medication (except onabotulinumtoxinA). Patients with a dual diagnosis of chronic migraine and medication overuse headache attributable to acute medication overuse (triptans, ergotamine, or combination analgesics greater than 10 days per month) were included in the study population. Patients using opioids or butalbital-containing products greater than 4 days per month were not allowed.
The study excluded patients with a history of cardiovascular disease (hypertension, ischemic heart disease), neurological disease, or cerebrovascular disease.
The primary efficacy endpoint was the change from baseline in mean monthly migraine days over Months 1-3. Secondary endpoints included the percentages of patients with 50% or greater and 75% or greater reductions from baseline in monthly migraine days over Months 1-3.
Patients had a median age of 41 years (range: 18 to 65 years), 88% were female, and 91% were white. Forty-one percent of patients were taking concomitant preventive medication for migraine. The mean migraine frequency at baseline was approximately 16.1 migraine days per month and was similar across treatment groups.
VYEPTI treatment demonstrated statistically significant improvements compared to placebo for the primary efficacy endpoint, as shown in Table 3; secondary endpoints are also summarized in Table 3.
Table 3. Efficacy Endpoint Results in Study 2:
| VYEPTI 100 mg N=356 | VYEPTI 300 mg N=350 | Placebo N=366 | |
|---|---|---|---|
| Monthly Migraine Days (MMD) – Months 1-3 | |||
| Change from baseline | -7.7 | -8.2 | -5.6 |
| Difference from placebo | -2.0 | -2.6 | |
| p-value | <0.001 | <0.001 | |
| ≥50% MMD responders –Months 1-3 | |||
| % Responders | 57.6% | 61.4% | 39.3% |
| Difference from placebo | 18.2% | 22.1% | |
| p-value | <0.001 | <0.001 | |
| ≥75% MMD responders – Months 1-3 | |||
| % Responders | 26.7% | 33.1% | 15.0% |
| Difference from placebo | 11.7% | 18.1% | |
| p-value | <0.001 | <0.001 | |
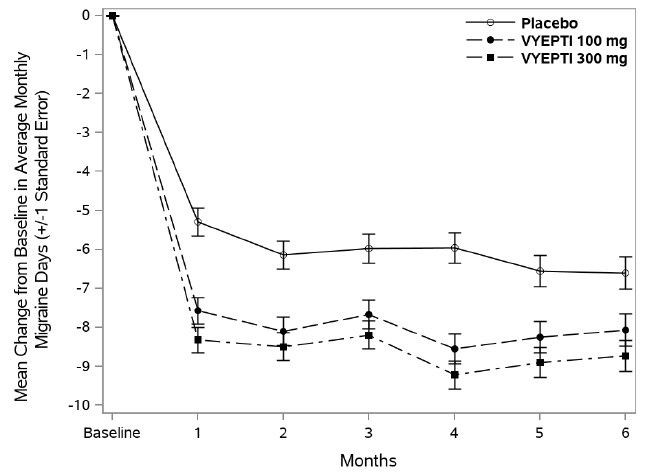
Figure 4 shows the mean change from baseline in average monthly migraine days for Study 2. Patients treated with VYEPTI at both doses had greater mean decreases from baseline in mean monthly migraine days over Month 1-3 compared to placebo-treated patients.
Figure 4. Change from Baseline in Monthly Migraine Days in Study 2:
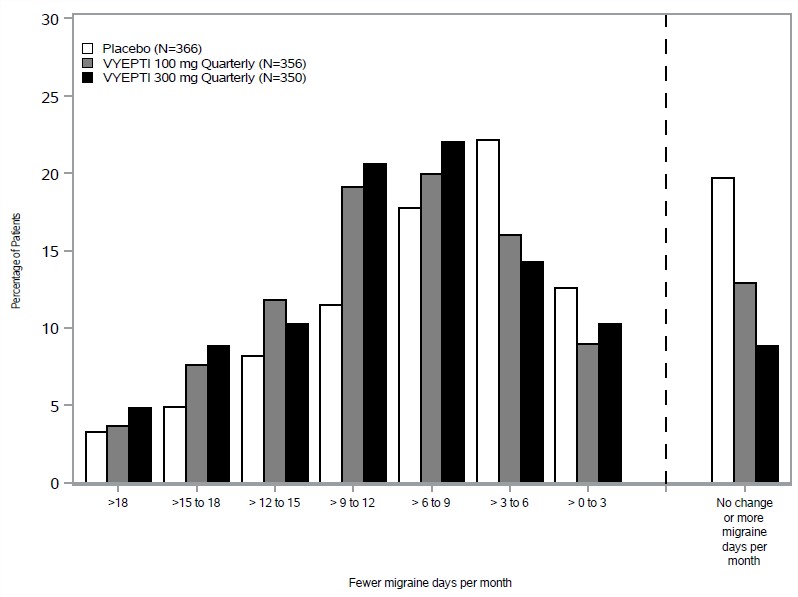
Figure 5 shows the distribution of change from baseline in mean monthly migraine days through Month 3 by treatment group in 3-day increments.
Figure 5. Distribution of Change from Baseline in Mean Monthly Migraine Days over Months 1-3 by Treatment Group in Study 2:
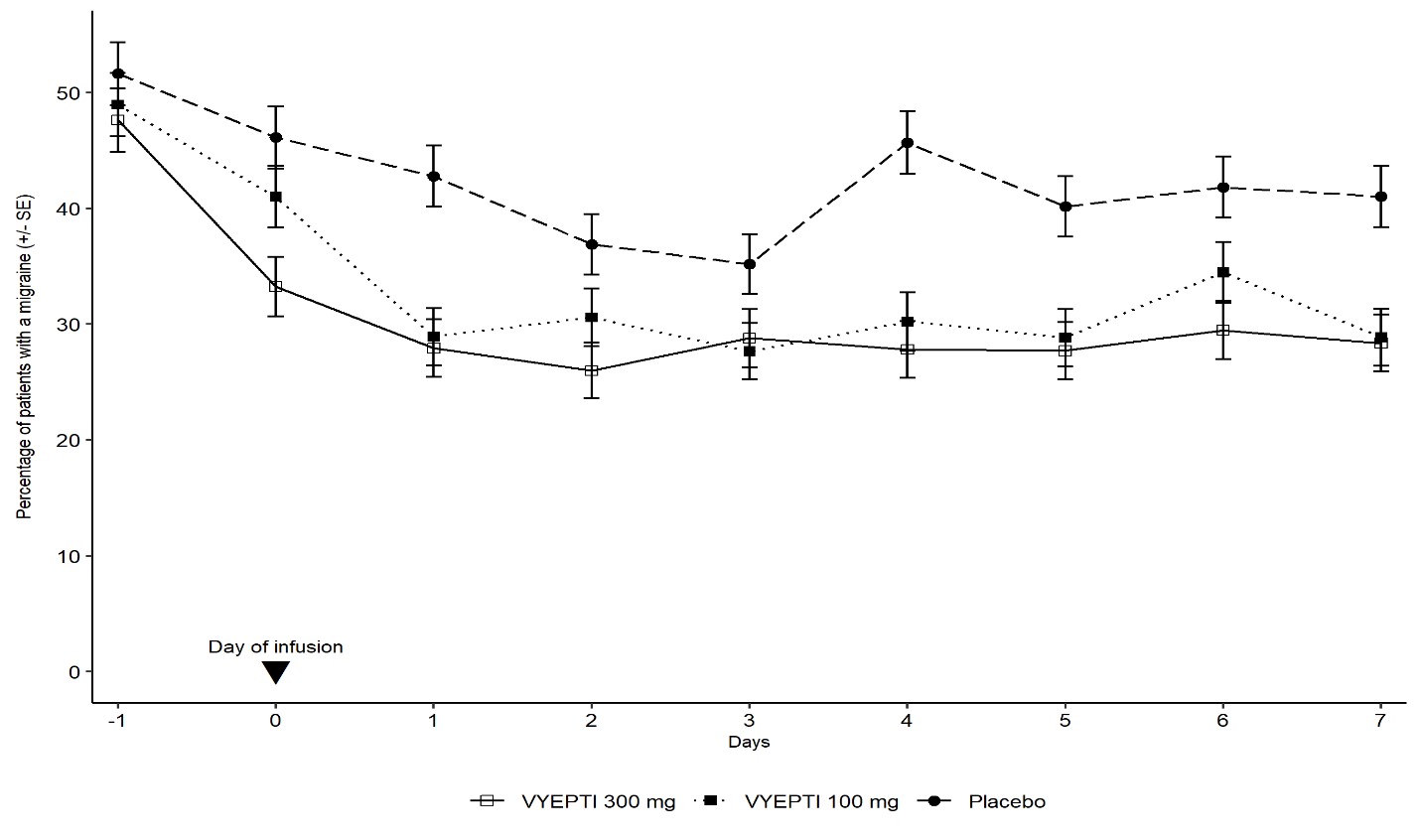
Figure 6 demonstrates that greater percentages of placebo-treated patients had migraines on individual days during the first 7 days of treatment compared to VYEPTI-treated patients in Study 2.
Figure 6. Percentage of Patients with a Migraine from Day -1 (Day Prior to Infusion) to Day 7 in Study 2:
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.