XCOPRI Film-coated tablet Ref.[10091] Active ingredients: Cenobamate
Source: FDA, National Drug Code (US) Revision Year: 2020
12.1. Mechanism of Action
The precise mechanism by which cenobamate exerts its therapeutic effects in patients with partial-onset seizures is unknown. Cenobamate has been demonstrated to reduce repetitive neuronal firing by inhibiting voltage-gated sodium currents. It is also a positive allosteric modulator of the γ-aminobutyric acid (GABAA) ion channel.
12.2. Pharmacodynamics
Interactions with Alcohol
No clinically significant differences on objective attention, psychomotor performance, and memory tests, in addition to other subjective CNS tests, were observed following concomitant use of XCOPRI and ethanol (preparation of 40% ethanol in orange juice dosed at 0.7 g/kg for males and 0.57 g/kg for females) in healthy subjects.
Cardiac Electrophysiology
In a placebo-controlled QT study in healthy volunteers, dose-dependent shortening of the QTcF interval has been observed with XCOPRI [see Warnings and Precautions (5.2)]. The mean ΔΔQTc is -11 [-13, -8] msec for 200 mg once daily and -18 [-22, -15] msec for 500 mg once daily (1.25 times the maximum recommended dosage). A higher percentage of XCOPRI-treated subjects (31% at 200 mg and 66% at 500 mg) had a QT shortening of greater than 20 msec compared to placebo (6-17%). Reductions of the QTc interval below 300 msec were not observed.
12.3. Pharmacokinetics
Cenobamate AUC increases in a greater than dose-proportional manner following single oral doses from 5 to 750 mg (0.0125 to 1.88 times the maximum recommended dosage). Cenobamate Cmax increases in a dose proportional manner. Steady-state plasma concentrations are attained after approximately two weeks of once daily dosing.
The pharmacokinetics of cenobamate are similar when used as monotherapy or as adjunctive therapy for the treatment of partial-onset seizures, except plasma cenobamate multiple-dose exposure (Cmax, AUC) decreased with co-administration of phenytoin by 27-28%.
Absorption
At least 88% of XCOPRI is absorbed following oral administration, with median Tmax ranging from 1 to 4 hours.
Effect of Food
No clinically significant differences in cenobamate pharmacokinetics were observed following administration of a high-fat meal (800-1000 calories with 50% fat).
Distribution
The apparent volume of distribution (Vd/F) of cenobamate after oral administration of XCOPRI is approximately 40-50 L. Plasma protein binding of cenobamate is 60% and independent of concentration in vitro. Cenobamate primarily binds with human albumin protein.
Elimination
The apparent terminal half-life of cenobamate is 50-60 hours and apparent oral clearance is approximately 0.45-0.63 L/hour over a dose range from 100 mg/day to 400 mg/day.
Metabolism
Cenobamate is extensively metabolized. The primary metabolic pathways are by glucuronidation via UGT2B7 and to a lesser extent by UGT2B4, and by oxidation via CYP2E1, CYP2A6, CYP2B6, and to a lesser extent by CYP2C19 and CYP3A4/5.
Following administration of radiolabeled cenobamate, unchanged cenobamate accounted for greater than 98% of the total AUC of radioactivity in plasma. Unchanged cenobamate accounted for 6.8% of the dose which was mainly excreted in the urine (6.4%).
Excretion
Following administration of radiolabeled cenobamate, a mean of 93.0% of the total radioactive dose was recovered in urine (87.8%) and feces (5.2%). More than 50% of the radioactivity was excreted within 72 hours of dosing.
Specific Populations
No clinically significant differences in the pharmacokinetics of cenobamate were observed based on age based on data from subjects age 18 years to 77 years, sex, or race/ethnicity based on data from subjects categorized as Asian, Black, Caucasian, Hispanic, or Other.
Patients with Renal Impairment
Cenobamate plasma AUC was 1.4 fold to 1.5 fold higher in subjects with mild (CLcr 60 to less than 90 mL/min) and moderate (CLcr 30 to less than 60 mL/min) following a single oral 200 mg dose of XCOPRI compared to healthy controls. In subjects with severe (CLcr less than 30 mL/min) renal impairment, cenobamate plasma AUC did not change significantly compared to healthy controls following single oral 100 mg dose of XCOPRI [see Use in Specific Populations (8.6)]. The effect of hemodialysis on cenobamate pharmacokinetics has not been studied.
Patients with Hepatic Impairment
Cenobamate plasma AUC was 2.1-fold and 2.3-fold higher in subjects with mild (5-6 points on Child-Pugh assessment) and moderate (7-9 points on Child-Pugh assessment) hepatic impairment, respectively, following a single oral 200 mg dose of XCOPRI compared to matched healthy controls [see Dosage and Administration (2.3) and Use in Specific Populations (8.7)].The effect of severe hepatic impairment on cenobamate pharmacokinetics has not been studied.
Drug Interaction Studies
Clinical Studies
Alcohol:
No clinically significant pharmacokinetic differences were observed for either cenobamate or alcohol when administered concomitantly.
AEDs:
Multiple doses of concomitant XCOPRI 200 mg once daily increased phenytoin mean Cmax and AUC by 70% and 84%, respectively, and phenobarbital mean Cmax and AUC by 34% and 37%, respectively [see Drug Interactions (7.1)]. Multiple doses of concomitant XCOPRI 200 mg once daily decreased carbamazepine mean Cmax and AUC each by 23% [see Drug Interactions (7.1].
No clinically significant differences in the pharmacokinetics of the following drugs were observed when used concomitantly with cenobamate: valproic acid, levetiracetam or lacosamide.
Based on population PK analyses, during treatment within the 100-400 mg/day XCOPRI dose range, lamotrigine concentrations are expected to decrease by 21-52% [see Drug Interactions (7.1)]; and levetiracetam concentrations are expected to decrease by 4-13%, which is not expected to be clinically significant.
In subjects treated with XCOPRI in Study 1 and Study 2, there was no clear relationship between efficacy and concomitant oxcarbazepine use. As such, the efficacy data from Study 1 and Study 2 do not support the existence of a clinically relevant interaction perpetrated by XCOPRI against oxcarbazepine.
CYP Substrates:
Multiple doses of concomitant XCOPRI 200 mg once daily decreased total bupropion (CYP2B6 substrate) mean Cmax and AUC by 23% and 39%, respectively, and decreased midazolam (CYP3A substrate) mean Cmax and AUC by 61% and 72%, respectively [see Drug Interactions (7.1)]. Multiple doses of concomitant XCOPRI 200 mg once daily increased the omeprazole (CYP2C19 substrate) mean Cmax and AUC by 83% and 107%, respectively [see Drug Interactions (7.1)]. No clinically significant differences in the pharmacokinetics of warfarin (CYP2C9 substrate) were observed when used concomitantly with cenobamate.
The effects of concomitant AEDs on cenobamate PK:
Plasma cenobamate multiple-dose exposure (Cmax, AUC) decreased with co-administration of phenytoin by 27-28%. However, repeated dosing of valproate, phenobarbital, and carbamazepine did not have any significant impact on plasma cenobamate multiple-dose exposure.
In Vitro Studies
CYP Enzymes:
Cenobamate inhibits CYP2B6, CYP2C19, and CYP3A, but cenobamate does not inhibit CYP1A2, CYP2C8, CYP2C9, or CYP2D6.
Cenobamate induces CYP2B6, CYP2C8, and CYP3A4, but cenobamate does not induce CYP1A2, CYP2C9, or CYP2C19.
Transporters Systems:
Cenobamate was not a substrate of P-gp, BCRP, OAT1, OAT3, OCT2, MATE1, or MATE2-K, and cenobamate did not inhibit P-gp, OAT1, OCT1, OCT2, OATP1B3, BSEP, OAT3, or OATP1B1.
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Oral administration of cenobamate (0, 5, 15, or 35 mg/kg/day) to Tg.rasH2 mice for up to 26 weeks did not result in an increase in tumors. Oral administration of cenobamate (0, 4, 8, or 20 mg/kg/day) to male and female rats for up to 87 or 90 weeks, respectively, did not result in an increase in tumors. Plasma exposure at the highest dose tested in rats was less than that in humans at the maximum recommended human dose (MRHD) of 400 mg/day.
Mutagenesis
Cenobamate was negative for genotoxicity in in vitro (Ames, mouse lymphoma) and in vivo (rat bone marrow micronucleus) assays.
Impairment of Fertility
Oral administration of cenobamate (0, 11, 22, or 44 mg/kg/day) to male and female rats prior to and throughout mating and continuing in females to Gestation Day 6 did not produce adverse effects on fertility, general reproductive performance, or early embryonic development. Plasma exposure (AUC) at the highest dose tested in rats was less than that in humans at the MRHD.
14. Clinical Studies
The efficacy of XCOPRI for the treatment of partial-onset seizures was established in two multicenter, randomized, double-blind, placebo-controlled studies in adult patients (Study 1 and Study 2). Patients enrolled in the studies had partial-onset seizures with or without secondary generalization and were not adequately controlled with 1 to 3 concomitant AEDs. During an 8-week baseline period, patients were required to have at least 3 or 4 partial-onset seizures per 28 days on average with no seizure-free period exceeding 3 to 4 weeks. In these studies, patients had a mean duration of epilepsy of approximately 24 years and median baseline seizure frequency of 8.5 seizures per 28 days. More than 80% of patients were taking 2 or more concomitant AEDs.
Study 1 (NCT01397968) compared doses of XCOPRI 200 mg/day with placebo. Study 2 (NCT01866111) compared doses of XCOPRI 100 mg/day, 200 mg/day, and 400 mg/day with placebo. Both studies had an 8-week baseline period to establish a baseline seizure frequency, following which patients were randomized to a treatment arm. Patients entered a treatment period consisting of an initial titration phase (6 weeks), and a subsequent maintenance phase (6 weeks for Study 1 and 12 weeks for Study 2). In Study 1, patients were started on a daily dose of 50 mg (a higher starting dose than currently recommended) and subsequently increased by 50 mg/day every two weeks, until the final daily target dose of 200 mg/day was achieved. In Study 2, patients were started on a daily dose of 50 mg (a higher starting dose than currently recommended) and subsequently increased by 50 mg/day every week (a faster titration than currently recommended) until 100 mg/day or 200 mg/day was reached and then increased by 100 mg/day every week in patients randomized to 400 mg/day [see Dosage and Administration (2.2), Warnings and Precautions (5.1), and Adverse Reactions (6.1)].
The primary efficacy outcome in Study 1 and Study 2 was the percent change from baseline in seizure frequency per 28 days in the treatment period. Table 6 summarizes the results of the primary endpoint for XCOPRI in each study.
Table 6. Percent Change from Baseline in Seizure Frequency per 28 Days in the Treatment Period (Study 1 and Study 2):
| N | Median Percent Change from Baseline in Seizure Frequency per 28 Days (%) * | p-value (Compared to Placebo) | |
|---|---|---|---|
| Study 1 | |||
| Placebo | 108 | -21.5 | -- |
| XCOPRI 200 mg/day | 113 | -55.6 | <0.0001** |
| Study 2 | |||
| Placebo | 106 | -24.3 | -- |
| XCOPRI 100 mg/day | 108 | -36.3 | 0.006** |
| XCOPRI 200 mg/day | 109 | -55.2 | <0.001** |
| XCOPRI 400 mg/day | 111 | -55.3 | <0.001** |
* A negative percent change from baseline in seizure frequency indicates reduction in seizure frequency from baseline.
** Statistically significant compared to placebo.
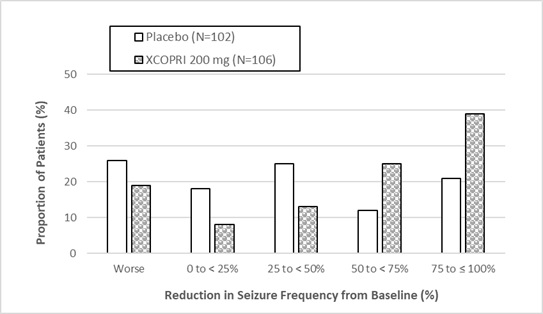
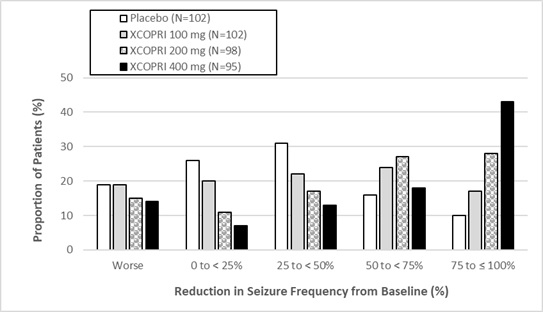
Figure 1 and Figure 2 show the proportion of patients with different percent reductions during the maintenance phase over baseline in Study 1 and Study 2, respectively. Patients in whom the seizure frequency increased are shown in the left-most column as “worse”. Patients in whom the seizure frequency decreased are shown in the remaining four categories.
Figure 1. Proportion of Patients Exhibiting Different Percent Reductions During the Maintenance Phase over Baseline in Study 1:
Figure 2. Proportion of Patients Exhibiting Different Percent Reductions During the Maintenance Phase over Baseline in Study 2:
In Study 2, 4 of 102 (4%) patients in the XCOPRI 100 mg/day group, 11 of 98 (11%) patients in the XCOPRI 200 mg/day group, and 20 of 95 (21%) patients in the XCOPRI 400 mg/day group and 1 of 102 (1%) of patients in the placebo group reported no partial seizures during the maintenance phase.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.