ZAPONEX Orodispersible tablet Ref.[7178] Active ingredients: Clozapine
Source: Medicines & Healthcare Products Regulatory Agency (GB) Revision Year: 2020 Publisher: Leyden Delta BV, Neerbosscheweg 620, 6544 LL, Nijmegen, The Netherlands
Contraindications
- Hypersensitivity to the active substance or to any of the excipients, listed in section 6.1.
- Patients unable to undergo regular blood tests.
- History of toxic or idiosyncratic granulocytopenia/agranulocytosis (with the exception of granulocytopenia/agranulocytosis from previous chemotherapy).
- History of clozapine-induced agranulocytosis.
- Clozapine treatment must not be started concurrently with substances known to have a substantial potential for causing agranulocytosis; concomitant use of depot antipsychotics is to be discouraged.
- Impaired bone marrow function.
- Uncontrolled epilepsy.
- Alcoholic and other toxic psychoses, drug intoxication, comatose conditions.
- Circulatory collapse and/or CNS depression of any cause.
- Severe renal or cardiac disorders (e.g. myocarditis).
- Active liver disease associated with nausea, anorexia or jaundice; progressive liver disease, hepatic failure.
- Paralytic ileus.
Special warnings and precautions for use
Agranulocytosis
Clozapine can cause agranulocytosis. The incidence of agranulocytosis and the fatality rate in those developing agranulocytosis have decreased markedly since the institution of white blood cell (WBC) counts and absolute neutrophil count (ANC) monitoring. The following precautionary measures are therefore mandatory and should be carried out in accordance with official recommendations.
Because of the risks associated with clozapine, its use is limited to patients in whom therapy is indicated as set out in section 4.1 and:
- who have initially normal leukocyte findings (WBC count ≥3500/mm³ (3.5x109/L) and ANC ≥2000/mm³ (2.0x109/L), and
- in whom regular WBC counts and ANC can be performed weekly for the first 18 weeks and at least 4-week intervals thereafter. Monitoring must continue throughout treatment and for 4 weeks after complete discontinuation of clozapine.
Before initiating clozapine therapy patients should have a blood test (see “agranulocytosis”) and a history and physical examination. Patients with history of cardiac illness or abnormal cardiac findings on physical examination should be referred to a specialist for other examinations that might include an ECG, and the patient treated only if the expected benefits clearly outweigh the risks (see section 4.3). The treating physician should consider performing a pre-treatment ECG.
Prescribing physicians must comply fully with the required safety measures.
Prior to treatment initiation, physicians must ensure, to the best of their knowledge, that the patient has not previously experienced an adverse haematological reaction to clozapine that necessitated its discontinuation. Prescriptions should not be issued for periods longer than the interval between two blood counts.
Immediate discontinuation of clozapine is mandatory if either the WBC count is less than 3000/mm³ (3.0x109/L) or the ANC is less than 1500/mm³ (1.5x109/L) at any time during clozapine treatment. Patients in whom clozapine has been discontinued as a result of either WBC or ANC deficiencies must not be re-exposed to clozapine.
At each consultation, a patient receiving clozapine must be reminded to contact the treating physician immediately if any kind of infection begins to develop. Particular attention should be paid to flu-like complaints such as fever or sore throat and to other evidence of infection, which may be indicative of neutropenia. Patients and their caregivers must be informed that, in the event of any of these symptoms, they must have a blood cell count performed immediately. Prescribers are encouraged to keep a record of all patients' blood results and to take any steps necessary to prevent these patients from accidentally being rechallenged in the future.
Patients with a history of primary bone marrow disorders may be treated only if the benefit outweighs the risk. They should be carefully reviewed by a haematologist prior to starting clozapine.
Patients who have low WBC counts because of benign ethnic neutropenia should be given special consideration and may only be started on clozapine with the agreement of a haematologist.
White Blood Cell (WBC) counts and Absolute Neutrophil Count (ANC) monitoring
WBC and differential blood counts must be performed within 10 days prior to initiating clozapine treatment to ensure that only patients with normal WBC counts and ANC (WBC count ≥3500/mm³ (3.5x109/L) and ANC ≥ 2000/mm 3 (2.0x109/L)) will receive clozapine. After the start of clozapine treatment regular WBC count and ANC must be assessed and monitored weekly for the first 18 weeks, and at least at four-week intervals thereafter.
Monitoring must continue throughout treatment and for 4 weeks after complete discontinuation of clozapine or until haematological recovery has occurred (see “Low WBC count/ANC” below). At each consultation, the patient must be reminded to contact the treating physician immediately if any kind of infection, fever, sore throat or other flu-like symptoms develop. WBC and differential blood counts must be performed immediately if any symptoms or signs of an infection occur.
Low WBC count/ANC
If, during clozapine therapy, either the WBC count falls to between 3500/mm³ (3.5x109/L) and 3000/mm³ (3.0x109/L) or the ANC falls to between 2000/mm³ (2.0x109/L) and 1500/mm 3 (1.5x109/L), haematological evaluations must be performed at least twice weekly until the patient’s WBC count and ANC stabilise within the range 3000-3500/mm³ (3.0-3.5x109/L) and 1500-2000/mm³ (1.5-2.0x109/L), respectively, or higher.
Immediate discontinuation of clozapine treatment is mandatory if either the WBC count is less than 3000/mm 3 (3.0x109/L) or the ANC is less than 1500/mm³ (1.5x109/L) during clozapine treatment. WBC counts and differential blood counts should then be performed daily and patients should be carefully monitored for flu-like symptoms or other symptoms suggestive of infection. Confirmation of the haematological values is recommended by performing two blood counts on two consecutive days; however, clozapine should be discontinued after the first blood count.
Following discontinuation of clozapine, haematological evaluation is required until haematological recovery has occurred.
Table 1:
| Blood cell count | Action required | |
|---|---|---|
| WBC/mm³ (/L) | ANC/mm³ (/L) | |
| ≥3500 (≥3.5x109) | ≥2000 (≥2.0x109) | Continue clozapine treatment |
| 3000-3500 (3.0x109-3.5x109) | 1500-2000 (1.5x109-2.0x109) | Continue clozapine treatment, sample blood twice weekly until counts stabilise or increase |
| <3000 (<3.0x109) | <1500 (<1.5x109) | Immediately stop clozapine treatment, sample blood daily until haematological abnormality is resolved, monitor for infection. Do not re-expose the patient |
If clozapine has been withdrawn and either a further drop in the WBC count below 2000/mm³ (2.0x109/L) occurs or the ANC falls below 1000/mm³ (1.0x109/L), the management of this condition must be guided by an experienced haematologist.
Discontinuation of therapy for haematological reasons
Patients in whom clozapine has been discontinued as a result of either WBC or ANC deficiencies (see above) must not be re-exposed to clozapine.
Prescribers are encouraged to keep a record of all patients' blood results and to take any steps necessary to prevent the patient being accidentally rechallenged in the future.
Discontinuation of therapy for other reasons
Patients who have been on clozapine for more than 18 weeks and have had their treatment interrupted for more than 3 days but less than 4 weeks should have their WBC count and ANC monitored weekly for an additional 6 weeks. If no haematological abnormality occurs, monitoring at intervals not exceeding 4 weeks may be resumed. If clozapine treatment has been interrupted for 4 weeks or longer, weekly monitoring is required for the next 18 weeks of treatment and the dose should be re-titrated (see section 4.2).
Eosinophilia
In the event of eosinophilia, discontinuation of clozapine is recommended if the eosinophil count rises above 3000/mm³ (3.0x109/L); therapy should be restarted only after the eosinophil count has fallen below 1000/mm³ (1.0x109/L).
Thrombocytopenia
In the event of thrombocytopenia, discontinuation of clozapine therapy is recommended if the platelet count falls below 50 000/mm³ (50x109/L).
Cardiovascular disorders
Orthostatic hypotension, with or without syncope, can occur during clozapine treatment. Rarely, collapse can be profound and may be accompanied by cardiac and/or respiratory arrest. Such events are more likely to occur with concurrent use of a benzodiazepine or any other psychotropic agent (see section 4.5) and during initial titration in association with rapid dose escalation; on very rare occasions they may occur even after the first dose. Therefore, patients commencing clozapine treatment require close medical supervision. Monitoring of standing and supine blood pressure is necessary during the first weeks of treatment in patients with Parkinson’s disease.
Analysis of safety databases suggests that the use of clozapine is associated with an increased risk of myocarditis especially during, but not limited to, the first two months of treatment. Some cases of myocarditis have been fatal.
Pericarditis/pericardial effusion and cardiomyopathy have also been reported in association with clozapine use; these reports also include fatalities. Myocarditis or cardiomyopathy should be suspected in patients who experience persistent tachycardia at rest, especially in the first two months of treatment, and/or palpitations, arrhythmias, chest pain and other signs and symptoms of heart failure (e.g. unexplained fatigue, dyspnoea, tachypnoea), or symptoms that mimic myocardial infarction. Other symptoms which may be present in addition to the above include flu-like symptoms. If myocarditis or cardiomyopathy is suspected, clozapine treatment should be promptly stopped and the patient immediately referred to a cardiologist.
In patients who are diagnosed with cardiomyopathy while on clozapine treatment, there is potential to develop mitral valve incompetence. Mitral valve incompetence has been reported in cases of cardiomyopathy related to clozapine treatment. These cases of mitral valve incompetence reported either mild or moderate mitral regurgitation on two- dimensional echocardiography (2DEcho) (see section 4.8).
Patients with clozapine-induced myocarditis or cardiomyopathy should not be re-exposed to clozapine.
Myocardial infarction
There have been post marketing reports of myocardial infarction, including fatal cases. Causality assessment was difficult in the majority of these cases because of serious pre-existing cardiac disease and plausible alternative causes.
QT interval prolongation
As with other antipsychotics, caution is advised in patients with known cardiovascular disease or family history of QT prolongation.
As with other antipsychotics, caution should be exercised when clozapine is prescribed with medicines known to increase QTc interval.
Cerebrovascular adverse events
An approximately 3-fold increased risk of cerebrovascular adverse events has been seen in randomised placebo controlled clinical trials in the dementia population with some atypical antipsychotics. The mechanism for this increased risk is not known. An increased risk cannot be excluded for other antipsychotics or other patient populations. Clozapine should be used with caution in patients with risk factors for stroke.
Risk of thromboembolism
Since clozapine may be associated with thromboembolism, immobilisation of patients should be avoided. Cases of venous thromboembolism (VTE) have been reported with antipsychotic drugs. Since patients treated with antipsychotics often present with acquired risk factors for VTE, all possible risk factors for VTE should be identified before and during treatment with clozapine and preventive measures undertaken.
Seizures
Patients with a history of epilepsy should be closely observed during clozapine therapy since dose-related convulsions have been reported. In such cases, the dose should be reduced (see section 4.2) and, if necessary, an anti-convulsant treatment should be initiated.
Anticholinergic effects
Clozapine exerts anticholinergic activity, which may produce undesirable effects throughout the body. Careful supervision is indicated in the presence of prostatic enlargement and narrow-angle glaucoma. Probably on account of its anticholinergic properties, clozapine has been associated with varying degrees of impairment of intestinal peristalsis, ranging from constipation to intestinal obstruction, faecal impaction and paralytic ileus, megacolon and intestinal infarction ischaemia (see section 4.8). On rare occasions these cases have been fatal. Particular care is necessary in patients who are receiving concomitant medications known to cause constipation (especially those with anticholinergic properties such as some antipsychotics, antidepressants and anti-parkinsonian treatments), have a history of colonic disease or a history of lower abdominal surgery as these may exacerbate the situation. It is vital that constipation is recognised and actively treated.
Fever
During clozapine therapy, patients may experience transient temperature elevations above 38°C, with the peak incidence within the first 3 weeks of treatment. This fever is generally benign. Occasionally, it may be associated with an increase or decrease in the WBC count. Patients with fever should be carefully evaluated to rule out the possibility of an underlying infection or the development of agranulocytosis. In the presence of high fever, the possibility of neuroleptic malignant syndrome (NMS) must be considered. If the diagnosis of NMS is confirmed, clozapine should be discontinued immediately and appropriate medical measures should be administered.
Falls
Clozapine may cause seizures, somnolence, postural hypotension, motor and sensory instability, which may lead to falls and, consequently, fractures or other injuries. For patients with diseases, conditions, or medications that could exacerbate these effects, complete fall risk assessments when initiating antipsychotic treatment and recurrently for patients on long-term antipsychotic therapy.
Metabolic changes
Atypical antipsychotic drugs, including clozapine, have been associated with metabolic changes that may increase cardiovascular/cerebrovascular risk. These metabolic changes may include hyperglycaemia, dyslipidaemia, and body weight gain. While atypical antipsychotic drugs may produce some metabolic changes, each drug in the class has its own specific profile.
Hyperglycaemia
Impaired glucose tolerance and/or development or exacerbation of diabetes mellitus has been reported rarely during treatment with clozapine. A mechanism for this possible association has not yet been determined. Cases of severe hyperglycaemia with ketoacidosis or hyperosmolar coma have been reported very rarely in patients with no prior history of hyperglycaemia, some of which have been fatal.
When follow-up data were available, discontinuation of clozapine resulted mostly in resolution of the impaired glucose tolerance, and reinstitution of clozapine resulted in its reoccurrence. Patients with an established diagnosis of diabetes mellitus who are started on atypical antipsychotics should be monitored regularly for worsening of glucose control. Patients with risk factors for diabetes mellitus (e.g. obesity, family history of diabetes) who are starting treatment with atypical antipsychotics should undergo fasting blood glucose testing at the beginning of treatment and periodically during treatment. Patients who develop symptoms of hyperglycaemia during treatment with atypical antipsychotics should undergo fasting blood glucose testing. In some cases, hyperglycaemia has resolved when the atypical antipsychotic was discontinued; however, some patients required continuation of antidiabetic treatment despite discontinuation of the suspect drug. The discontinuation of clozapine should be considered in patients where active medical management of their hyperglycaemia has failed.
Dyslipidaemia
Undesirable alterations in lipids have been observed in patients treated with atypical antipsychotics including clozapine. Clinical monitoring, including baseline and periodic follow-up lipid evaluations in patients using clozapine is recommended.
Weight gain
Weight gain has been observed with atypical antipsychotic use, including clozapine. Clinical monitoring of weight is recommended.
Rebound withdrawal effects
Acute withdrawal reactions have been reported following abrupt cessation of clozapine therefore gradual withdrawal is recommended. If abrupt discontinuation is necessary (e.g. because of leukopenia), the patient should be carefully observed for the recurrence of psychotic symptoms and symptoms related to cholinergic rebound, such as profuse sweating, headache, nausea, vomiting and diarrhoea.
Phenylketonurics
Zaponex orodispersible tablets contain aspartame, a source of phenylalanine which may be harmful for people with phenylketonuria.
Special populations
Hepatic impairment
Patients with stable pre-existing liver disorders may receive clozapine but need regular liver function tests. Liver function tests should be performed in patients in whom symptoms of possible liver dysfunction, such as nausea, vomiting and/or anorexia, develop during clozapine therapy. If the elevation of the values is clinically relevant (more than 3 times the UNL) or if symptoms of jaundice occur, treatment with clozapine must be discontinued. It may be resumed (see “Re-starting therapy” under section 4.2) only when the results of liver function tests are normal. In such cases, liver function should be closely monitored after re-introduction of the drug.
Patients aged 60 years and older
Initiation of treatment in patients aged 60 years and older is recommended at a lower dose (see section 4.2).
Orthostatic hypotension can occur with clozapine treatment and there have been reports of tachycardia, which may be sustained. Patients aged 60 years and older, particularly those with compromised cardiovascular function, may be more susceptible to these effects.
Patients aged 60 years and older, may also be particularly susceptible to the anticholinergic effects of clozapine, such as urinary retention and constipation.
Increased mortality in elderly people with dementia
Data from two large observational studies showed that elderly people with dementia who are treated with antipsychotics are at a small increased risk of death compared with those who are not treated. There are insufficient data to give a firm estimate of the precise magnitude of the risk and the cause of the increased risk is not known.
Clozapine is not approved for the treatment of dementia-related behavioural disturbances.
Interaction with other medicinal products and other forms of interaction
Contraindication of concomitant use
Substances known to have a substantial potential to depress bone marrow function must not be used concurrently with clozapine (see section 4.3).
Long-acting depot antipsychotics (which have myelosuppressive potential) must not be used concurrently with clozapine because these cannot be rapidly removed from the body in situations where this may be required, e.g. neutropenia (see section 4.3).
Alcohol should not be used concomitantly with clozapine due to possible potentiation of sedation.
Precautions including dose adjustment
Clozapine may enhance the central effects of CNS depressants such as narcotics, antihistamines, and benzodiazepines. Particular caution is advised when clozapine therapy is initiated in patients who are receiving a benzodiazepine or any other psychotropic substance. These patients may have an increased risk of circulatory collapse, which, on rare occasions, can be profound and may lead to cardiac and/or respiratory arrest. It is not clear whether cardiac or respiratory collapse can be prevented by dose adjustment.
Because of the possibility of additive effects, caution is essential in the concomitant administration of substances possessing anticholinergic, hypotensive, or respiratory depressant effects.
Owing to its anti-alpha-adrenergic properties, clozapine may reduce the blood-pressure-increasing effect of norepinephrine or other predominantly alpha-adrenergic agents and reverse the pressor effect of epinephrine.
Concomitant administration of substances known to inhibit the activity of some cytochrome P450 isozymes may increase the levels of clozapine, and the dose of clozapine may need to be reduced to prevent undesirable effects. This is more important for CYP 1A2 inhibitors such as caffeine (see below), perazine and the selective serotonin reuptake inhibitor fluvoxamine. Some of the other serotonin reuptake inhibitors such as fluoxetine, paroxetine, and, to a lesser degree, sertraline, are CYP 2D6 inhibitors and, as a consequence, major pharmacokinetic interactions with clozapine are less likely. Similarly, pharmacokinetic interactions with CYP 3A4 inhibitors such as azole antimycotics, cimetidine, erythromycin and protease inhibitors are unlikely, although some have been reported. Hormonal contraceptives (including combinations of estrogen and progesterone or progesterone only) are CYP 1A2, CYP 3A4 and CYP 2C19 inhibitors. Therefore, initiation or discontinuation of hormonal contraceptives, may require dose adjustment of clozapine according to the individual medical need. Because the plasma concentration of clozapine is increased by caffeine intake and decreased by nearly 50% following a 5-day caffeine-free period, dosage changes of clozapine may be necessary when there is a change in caffeine-drinking habit. In cases of sudden cessation of smoking, the plasma clozapine concentration may be increased, thus leading to an increase in adverse effects.
Cases have been reported of an interaction between citalopram and clozapine, which may increase the risk of adverse events associated with clozapine. The nature of this interaction has not been fully elucidated.
Concomitant administration of substances known to induce cytochrome P450 enzymes may decrease the plasma levels of clozapine, leading to reduced efficacy. Substances known to induce the activity of cytochrome P450 enzymes and with reported interactions with clozapine include, for instance, carbamazepine (not to be used concomitantly with clozapine, due to its myelosuppressive potential), phenytoin and rifampicin. Known inducers of CYP1A2, such as omeprazole, may lead to decreased clozapine levels. The potential for reduced efficacy of clozapine should be considered when it is used in combination with these substances.
Other
Concomitant use of lithium or other CNS-active agents may increase the risk of development of neuroleptic malignant syndrome (NMS).
Rare but serious reports of seizures, including onset of seizures in non-epileptic patients, and isolated cases of delirium where clozapine was co-administered with valproic acid have been reported. These effects are possibly due to a pharmacodynamic interaction, the mechanism of which has not been determined.
Caution is called for in patients receiving concomitant treatment with other substances which are either inhibitors or inducers of the cytochrome P450 isozymes. With tricyclic antidepressants, phenothiazines and type 1 c anti-arrhythmics, which are known to bind to cytochrome P450 2D6, no clinically relevant interactions have been observed thus far.
As with other antipsychotics, caution should be exercised when clozapine is prescribed with medicines known to increase QTc interval or causing electrolyte imbalance.
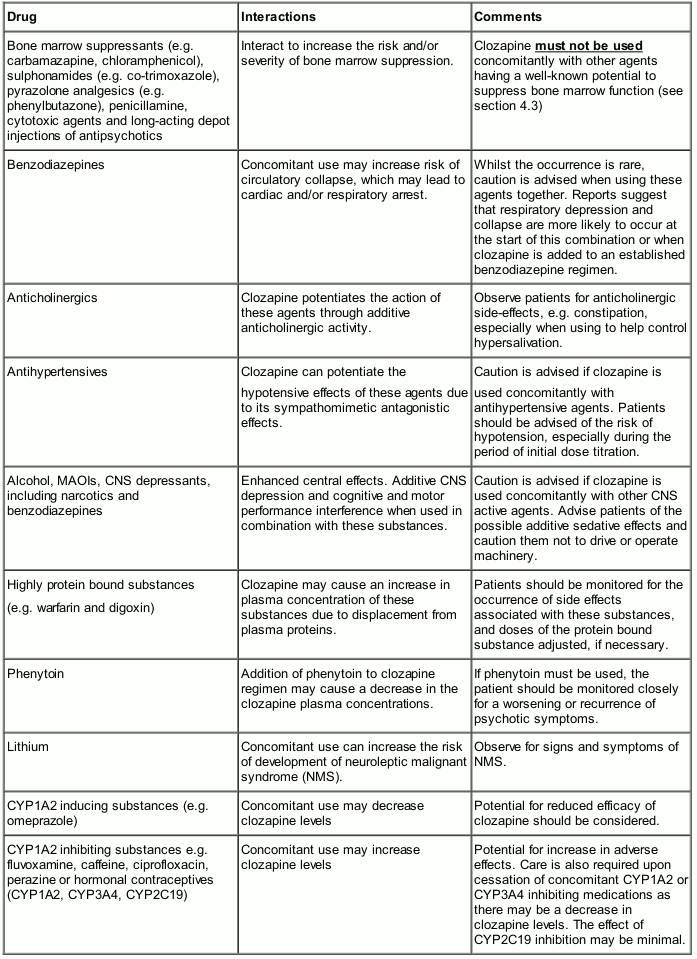
An outline of drug interactions believed to be most important with clozapine is given in Table 2 below. The list is not exhaustive.
Table 2. Reference to the most common drug interactions with clozapine:
Fertility, pregnancy and lactation
Pregnancy
For clozapine, there are only limited clinical data on exposed pregnancies. Animal studies do not indicate direct or indirect harmful effects with respect to pregnancy, embryonal/foetal development, parturition or postnatal development (see section 5.3). Caution should be exercised when prescribing to pregnant women.
Neonates exposed to antipsychotics (including clozapine) during the third trimester of pregnancy are at risk of adverse reactions including extrapyramidal and/or withdrawal symptoms that may vary in severity and duration following delivery. There have been reports of agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress, or feeding disorder. Consequently, newborns should be monitored carefully.
Breastfeeding
Animal studies suggest that clozapine is excreted in breast milk and has an effect in the nursing infant; therefore, mothers receiving clozapine should not breast-feed.
Fertility
Limited data available on the effects of clozapine on human fertility are inconclusive. In male and female rats, clozapine did not affect fertility when administered up to 40 mg/kg, corresponding to a human equivalence dose of 6.4 mg/kg or approximately a third of the maximum permissible adult human dose.
Women of child-bearing potential
A return to normal menstruation may occur as a result of switching from other antipsychotics to clozapine. Adequate contraceptive measures must therefore be ensured in women of childbearing potential.
Effects on ability to drive and use machines
Owing to the ability of clozapine to cause sedation and lower the seizure threshold, activities such as driving or operating machinery should be avoided, especially during the initial weeks of treatment.
Undesirable effects
Summary of the safety profile
For the most part, the adverse event profile of clozapine is predictable from its pharmacological properties. An important exception is its propensity to cause agranulocytosis (see section 4.4). Because of this risk, its use is restricted to treatment-resistant schizophrenia and psychosis occurring during the course of Parkinson’s disease in cases where standard treatment has failed. While blood monitoring is an essential part of the care of patients receiving clozapine, the physician should be aware of other rare but serious adverse reactions, which may be diagnosed in the early stages only by careful observation and questioning of the patient in order to prevent morbidity and mortality.
The most serious adverse reactions experienced with clozapine are agranulocytosis, seizures, cardiovascular effects and fever (see section 4.4).
The most common side effects are drowsiness/sedation, dizziness, tachycardia, constipation and hypersalivation.
Data from the clinical trials experience showed that a varying proportion of clozapine-treated patients (from 7.1 to 15.6%) were discontinued due to an adverse event, including only those that could be reasonably attributed to clozapine. The more common events considered to be causes of discontinuation were leukopenia, somnolence, dizziness (excluding vertigo) and psychotic disorder.
Blood and lymphatic system
Development of granulocytopenia and agranulocytosis is a risk inherent to clozapine treatment. Although generally reversible on withdrawal of treatment, agranulocytosis may result in sepsis and can prove fatal. Because immediate withdrawal of treatment is required to prevent the development of life-threatening agranulocytosis, monitoring of the WBC count is mandatory (see section 4.4). Table 3 below summarises the estimated incidence of agranulocytosis for each clozapine treatment period.
Table 3. Estimated incidence of agranulocytosis1:
| Treatment period | Incidence of agranulocytosis per 100,000 person-weeks2 of observation |
|---|---|
| Weeks 0-18 | 32.0 |
| Weeks 19-52 | 2.3 |
| Weeks 53 and higher | 1.8 |
1 From the UK Clozaril Patient Monitoring Service lifetime registry experience between 1989 and 2001.
2 Person-time is the sum of individual units of time that the patients in the registry were exposed to clozapine before experiencing agranulocytosis. For example, 100,000 person-weeks could be observed in 1,000 patients who were in the registry for 100 weeks (100*1000=100,000), or in 200 patients who were in the registry for 500 weeks (200*500=100,000) before experiencing agranulocytosis.
The cumulative incidence of agranulocytosis in the UK Clozaril Patient Monitoring Service lifetime registry experience (0-11.6 years between 1989 and 2001) is 0.78%. The majority of cases (approximately 70%) occur within the first 18 weeks of treatment.
Metabolic and Nutritional Disorders
Impaired glucose tolerance and/or development or exacerbation of diabetes mellitus has been reported rarely during treatment with clozapine. On very rare occasions, severe hyperglycaemia, sometimes leading to ketoacidosis/hyperosmolar coma, has been reported in patients on clozapine treatment with no prior history of hyperglycaemia. Glucose levels normalised in most patients after discontinuation of clozapine and in a few cases hyperglycaemia recurred when treatment was reinitiated. Although most patients had risk factors for non-insulin- dependent diabetes mellitus, hyperglycaemia has also been documented in patients with no known risk factors (see section 4.4).
Nervous System Disorders
The very common adverse reactions observed include drowsiness/sedation, and dizziness.
Clozapine can cause EEG changes, including the occurrence of spike and wave complexes. It lowers the seizure threshold in a dose-dependent manner and may induce myoclonic jerks or generalised seizures. These symptoms are more likely to occur with rapid dose increases and in patients with pre-existing epilepsy. In such cases the dose should be reduced and, if necessary, anticonvulsant treatment initiated. Carbamazepine should be avoided because of its potential to depress bone marrow function, and with other anticonvulsant agents the possibility of a pharmacokinetic interaction should be considered. In rare cases, patients treated with clozapine may experience delirium.
Very rarely, tardive dyskinesia has been reported in patients on clozapine who had been treated with other antipsychotic agents. Patients in whom tardive dyskinesia developed with other antipsychotics have improved on clozapine.
Cardiac Disorders
Tachycardia and postural hypotension with or without syncope may occur, especially in the initial weeks of treatment. The prevalence and severity of hypotension is influenced by the rate and magnitude of dose titration. Circulatory collapse as a result of profound hypotension, in particular related to aggressive titration, with the possible serious consequences of cardiac or pulmonary arrest, has been reported with clozapine.
A minority of clozapine-treated patients experience ECG changes similar to those seen with other antipsychotics, including S-T segment depression and flattening or inversion of T waves, which normalise after discontinuation of clozapine. The clinical significance of these changes is unclear. However, such abnormalities have been observed in patients with myocarditis, which should therefore be considered.
Isolated cases of cardiac arrhythmias, pericarditis/pericardial effusion and myocarditis have been reported, some of which have been fatal. The majority of the cases of myocarditis occurred within the first 2 months of initiation of therapy with clozapine. Cardiomyopathy generally occurred later in the treatment.
Eosinophilia has been co-reported with some cases of myocarditis (approximately 14%) and pericarditis/pericardial effusion; it is not known, however, whether eosinophilia is a reliable predictor of carditis.
Signs and symptoms of myocarditis or cardiomyopathy include persistent tachycardia at rest, palpitations, arrhythmias, chest pain and other signs and symptoms of heart failure (e.g. unexplained fatigue, dyspnoea, tachypnoea), or symptoms that mimic myocardial infarction. Other symptoms which may be present in addition to the above include flu-like symptoms.
Sudden, unexplained deaths are known to occur among psychiatric patients who receive conventional antipsychotic medication but also among untreated psychiatric patients. Such deaths have been reported very rarely in patients receiving clozapine.
Vascular Disorders
Rare cases of thromboembolism have been reported.
Respiratory System
Respiratory depression or arrest has occurred very rarely, with or without circulatory collapse (see sections 4.4 and 4.5).
Gastrointestinal System
Constipation and hypersalivation have been observed very frequently, and nausea and vomiting frequently. Very rarely ileus may occur (see section 4.4). Rarely clozapine treatment may be associated with dysphagia. Aspiration of ingested food may occur in patients presenting with dysphagia or as a consequence of acute overdosage.
Hepatobiliary Disorders
Transient, asymptomatic elevations of liver enzymes and rarely, hepatitis and cholestatic jaundice may occur. Very rarely, fulminant hepatic necrosis has been reported. If jaundice develops, clozapine should be discontinued (see section 4.4). In rare cases, acute pancreatitis has been reported.
Renal Disorders
Isolated cases of acute interstitial nephritis have been reported in association with clozapine therapy.
Reproductive and Breast Disorders
Very rare reports of priapism have been received.
General Disorders
Cases of neuroleptic malignant syndrome (NMS) have been reported in patients receiving clozapine either alone or in combination with lithium or other CNS-active agents.
Acute withdrawal reactions have been reported (see section 4.4).
Tabulated list of adverse reactions
The table below (Table 4) summarises the adverse reactions accumulated from reports made spontaneously and during clinical studies.
Table 4. Treatment-emergent adverse experience frequency estimate from spontaneous and clinical trial reports:
Adverse reactions are ranked under headings of frequency, using the following convention: Very common (≥1/10), common (≥1/100 to <1/10), uncommon (≥1/1,000 to <1/100), rare (≥1/10,000 to <1/1,000), very rare (<1/10,000), not known (cannot be estimated from the available data).
Infections and infestations
Not known: Sepsis*
Blood and lymphatic system disorders
Common: Leukopenia/decreased WBC/neutropenia, eosinophilia, leukocytosis
Uncommon: Agranulocytosis
Rare: Anaemia
Very rare: Thrombocytopenia, thrombocythaemia
Immune system disorders
Not known: Angioedema*, leukocytoclastic vasculitis*, drug rash with eosinophilia and systemic symptoms (DRESS)*
Endocrine disorders
Not known: Pseudophaeochromocytoma*
Metabolism and nutrition disorders
Common: Weight gain
Rare: Diabetes mellitus , impaired glucose tolerance, obesity*
Very rare: Hyperosmolar coma, ketoacidosis, severe hyperglycaemia, hypercholesterolemia, hypertriglyceridemia
Psychiatric disorders
Common: Dysarthria
Uncommon: Dysphemia
Rare: Agitation, restlessness
Nervous system disorders
Very common: Drowsiness/sedation, dizziness
Common: Seizures/convulsions/myoclonic jerks, extrapyramidal symptoms, akathisia, tremor, rigidity, headache
Uncommon: Neuroleptic malignant syndrome
Rare: Confusion, delirium
Very rare: Tardive dyskinesia, obsessive compulsive symptoms
Not known: Cholinergic syndrome (after abrupt withdrawal), EEG changes, pleurothotonus*, restless legs syndrome*
Eye disorders
Common: Blurred vision
Cardiac disorders
Very common: Tachycardia
Common: ECG changes
Rare: Circulatory collapse, arrhythmias, myocarditis, pericarditis/pericardial effusion
Very rare: Cardiomyopathy, cardiac arrest
Not known: Myocardial infarction*,**, myocarditis*,**, chest pain/angina pectoris*, atrial fibrillation*, palpitations*, mitral valve incompetence associated with clozapine related cardiomyopathy*.
Vascular disorders
Common: Syncope, postural hypotension, hypertension
Rare: Thromboembolism
Not known: Hypotension*, venous thromboembolism
Respiratory, Thoracic and Mediastinal disorders
Rare: Aspiration of ingested food, pneumonia and lower respiratory tract infection which may be fatal, sleep apnoea syndrome*
Very rare: Respiratory depression/arrest
Not known: Pleural effusion*, nasal congestion*
Gastrointestinal disorders
Very common: Constipation, hypersalivation
Common: Nausea, vomiting, anorexia, dry mouth
Rare: Dysphagia
Very rare: Intestinal obstruction/paralytic ileus/faecal impaction, parotid gland enlargement
Not known: Megacolon*,**, intestinal infarction/ischaemia*,**, intestinal necrosis*,**, intestinal ulceration*,**, and intestinal perforation*,**, diarrhoea*, abdominal discomfort/heartburn/dyspepsia*, colitis*
Hepatobiliary disorders
Common: Elevated liver enzymes
Rare: Pancreatitis, hepatitis, cholestatic jaundice
Very rare: Fulminant hepatic necrosis
Not known: Hepatic steatosis*, hepatic necrosis*, hepatotoxicity*, hepatic fibrosis*, hepatic cirrhosis*, liver disorders including those hepatic events leading to life-threatening consequences such as liver injury (hepatic, cholestatic and mixed), liver failure which may be fatal and liver transplant*.
Skin and subcutaneous tissue disorders
Very rare: Skin reactions
Not known: Pigmentation disorder*
Muscoskeletal and connective tissue disorders
Not known: Rhabdomyolysis*, muscle weakness*, muscle spasms*, muscle pain*, systemic lupus erythematosus*
Renal and urinary disorders
Common: urinary retention, urinary incontinence
Very rare: tubulointerstitial nephritis
Not known: renal failure*, nocturnal enuresis*
Pregnancy, puerperium and perinatal conditions
Not known: drug withdrawal syndrome neonatal (see 4.6)
Reproductive system and breast disorders
Very rare: priapism
Not known: retrograde ejaculation*
General disorders and administration site conditions
Common: benign hyperthermia, disturbances in sweating/temperature regulation, fever, fatigue
Very rare: sudden unexplained death
Not known: polyserositis*
Investigations
Rare: increased CPK
Injury, poisoning and procedural complications
Uncommon: falls (associated with clozapine-induced seizures, somnolence, postural hypotension, motor and sensory instability)*
* Adverse drug reactions derived from post-marketing experience via spontaneous case reports and literature cases.
** These adverse drug reactions were sometimes fatal.
Very rare events of ventricular tachycardia and QT prolongation which may be associated with Torsades De Pointes have been observed although there is no conclusive causal relationship to the use of this medicine.
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the Yellow Card Scheme Website: www.mhra.gov.uk/yellowcard or search for MHRA Yellow Card in the Google Play or Apple App Store.
Incompatibilities
Not applicable.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.