ZYVOX Solution for injection Ref.[11116] Active ingredients: Linezolid
Source: FDA, National Drug Code (US) Revision Year: 2018
12.1. Mechanism of Action
ZYVOX is an antibacterial drug [see Microbiology (12.4)].
12.2. Pharmacodynamics
In a randomized, positive- and placebo-controlled crossover thorough QT study, 40 healthy subjects were administered a single ZYVOX 600 mg dose via a 1 hour IV infusion, a single ZYVOX 1200 mg dose via a 1 hour IV infusion, placebo, and a single oral dose of positive control. At both the 600 mg and 1200 mg ZYVOX doses, no significant effect on QTc interval was detected at peak plasma concentration or at any other time.
12.3. Pharmacokinetics
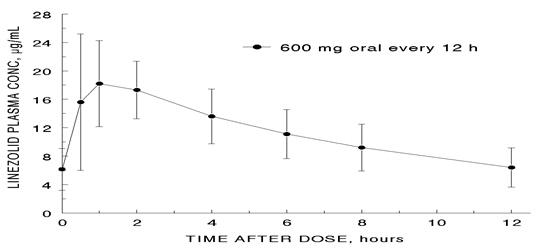
The mean pharmacokinetic parameters of linezolid in adults after single and multiple oral and intravenous doses are summarized in Table 8. Plasma concentrations of linezolid at steady-state after oral doses of 600 mg given every 12 hours are shown in Figure 1.
Table 8. Mean (Standard Deviation) Pharmacokinetic Parameters of Linezolid in Adults:
| Dose of Linezolid | C max mcg/mL | C min mcg/mL | T max hrs | AUC* mcg∙h/mL | t 1/2 hrs | CL mL/min |
|---|---|---|---|---|---|---|
| 400 mg tablet | ||||||
| single dose† | 8.10 (1.83) | --- | 1.52 (1.01) | 55.10 (25.00) | 5.20 (1.50) | 146 (67) |
| every 12 hours | 11.00 (4.37) | 3.08 (2.25) | 1.12 (0.47) | 73.40 (33.50) | 4.69 (1.70) | 110 (49) |
| 600 mg tablet | ||||||
| single dose | 12.70 (3.96) | --- | 1.28 (0.66) | 91.40 (39.30) | 4.26 (1.65) | 127 (48) |
| every 12 hours | 21.20 (5.78) | 6.15 (2.94) | 1.03 (0.62) | 138.00 (42.10) | 5.40 (2.06) | 80 (29) |
| 600 mg IV injection‡ | ||||||
| single dose | 12.90 (1.60) | --- | 0.50 (0.10) | 80.20 (33.30) | 4.40 (2.40) | 138 (39) |
| every 12 hours | 15.10 (2.52) | 3.68 (2.36) | 0.51 (0.03) | 89.70 (31.00) | 4.80 (1.70) | 123 (40) |
| 600 mg oral suspension | ||||||
| single dose | 11.00 (2.76) | --- | 0.97 (0.88) | 80.80 (35.10) | 4.60 (1.71) | 141 (45) |
Cmax = Maximum plasma concentration; C min = Minimum plasma concentration; Tmax = Time to Cmax; AUC = Area under concentration-time curve; t1/2 = Elimination half-life; CL = Systemic clearance
* AUC for single dose = AUC 0–∞; for multiple dose = AUC 0–τ
† Data dose-normalized from 375 mg
‡ Data dose-normalized from 625 mg, intravenous dose was given as 0.5-hour infusion.
Figure 1. Plasma Concentrations of Linezolid in Adults at Steady-State Following Oral Dosing Every 12 Hours (Mean ± Standard Deviation, n=16):
Absorption
Linezolid is extensively absorbed after oral dosing. Maximum plasma concentrations are reached approximately 1 to 2 hours after dosing, and the absolute bioavailability is approximately 100%. Therefore, linezolid may be given orally or intravenously without dose adjustment.
Linezolid may be administered without regard to the timing of meals. The time to reach the maximum concentration is delayed from 1.5 hours to 2.2 hours and Cmax is decreased by about 17% when high fat food is given with linezolid. However, the total exposure measured as AUC0–∞ is similar under both conditions.
Distribution
Animal and human pharmacokinetic studies have demonstrated that linezolid readily distributes to well-perfused tissues. The plasma protein binding of linezolid is approximately 31% and is concentration-independent. The volume of distribution of linezolid at steady-state averaged 40 to 50 liters in healthy adult volunteers.
Linezolid concentrations have been determined in various fluids from a limited number of subjects in Phase 1 volunteer studies following multiple dosing of linezolid. The ratio of linezolid in saliva relative to plasma was 1.2 to 1 and the ratio of linezolid in sweat relative to plasma was 0.55 to 1.
Metabolism
Linezolid is primarily metabolized by oxidation of the morpholine ring, which results in two inactive ring-opened carboxylic acid metabolites: the aminoethoxyacetic acid metabolite (A), and the hydroxyethyl glycine metabolite (B). Formation of metabolite A is presumed to be formed via an enzymatic pathway whereas metabolite B is mediated by a non-enzymatic chemical oxidation mechanism in vitro. In vitro studies have demonstrated that linezolid is minimally metabolized and may be mediated by human cytochrome P450. However, the metabolic pathway of linezolid is not fully understood.
Geriatric Patients
The pharmacokinetics of linezolid are not significantly altered in elderly patients (65 years or older). Therefore, dose adjustment for geriatric patients is not necessary.
Pediatric Patients
The pharmacokinetics of linezolid following a single intravenous dose were investigated in pediatric patients ranging in age from birth through 17 years (including premature and full-term neonates), in healthy adolescent subjects ranging in age from 12 through 17 years, and in pediatric patients ranging in age from 1 week through 12 years. The pharmacokinetic parameters of linezolid are summarized in Table 9 for the pediatric populations studied and healthy adult subjects after administration of single intravenous doses.
The Cmax and the volume of distribution (Vss) of linezolid are similar regardless of age in pediatric patients. However, plasma clearance of linezolid varies as a function of age. With the exclusion of pre-term neonates less than one week of age, weight-based clearance is most rapid in the youngest age groups ranging from <1 week old to 11 years, resulting in lower single-dose systemic exposure (AUC) and a shorter half-life as compared with adults. As the age of pediatric patients increases, the weight-based clearance of linezolid gradually decreases, and by adolescence mean clearance values approach those observed for the adult population. There is increased inter-subject variability in linezolid clearance and systemic drug exposure (AUC) across all pediatric age groups as compared with adults.
Similar mean daily AUC values were observed in pediatric patients from birth to 11 years of age dosed every 8 hours relative to adolescents or adults dosed every 12 hours. Therefore, the dosage for pediatric patients up to 11 years of age should be 10 mg/kg every 8 hours. Pediatric patients 12 years and older should receive 600 mg every 12 hours [ see Dosage and Administration (2)].
Table 9. Pharmacokinetic Parameters of Linezolid in Pediatrics and Adults Following a Single Intravenous Infusion of 10 mg/kg or 600 mg Linezolid (Mean: (%CV); [Min, Max Values]):
| Age Group | Cmax mcg/mL | V ss L/kg | AUC* mcg∙h/mL | t1/2 hrs | CL mL/min/kg |
|---|---|---|---|---|---|
| Neonatal Patients Pre-term† < 1 week (N=9)‡ | 12.7 (30%) [9.6, 22.2] | 0.81 (24%) [0.43, 1.05] | 108 (47%) [41, 191] | 5.6 (46%) [2.4, 9.8] | 2.0 (52%) [0.9, 4.0] |
| Full-term§ < 1 week (N=10)‡ | 11.5 (24%) [8.0, 18.3] | 0.78 (20%) [0.45, 0.96] | 55 (47%) [19, 103] | 3.0 (55%) [1.3, 6.1] | 3.8 (55%) [1.5, 8.8] |
| Full-term§ ≥ 1 week to ≤ 28 days (N=10)‡ | 12.9 (28%) [7.7, 21.6] | 0.66 (29%) [0.35, 1.06] | 34 (21%) [23, 50] | 1.5 (17%) [1.2, 1.9] | 5.1 (22%) [3.3, 7.2] |
| Infant Patients > 28 days to < 3 Months (N=12)‡ | 11.0 (27%) [7.2, 18.0] | 0.79 (26%) [0.42, 1.08] | 33 (26%) [17, 48] | 1.8 (28%) [1.2, 2.8] | 5.4 (32%) [3.5, 9.9] |
| Pediatric Patients 3 months through 11 years‡ (N=59) | 15.1 (30%) [6.8, 36.7] | 0.69 (28%) [0.31, 1.50] | 58 (54%) [19, 153] | 2.9 (53%) [0.9, 8.0] | 3.8 (53%) [1.0, 8.5] |
| Adolescent Subjects and Patients 12 through 17 years¶ (N=36) | 16.7 (24%) [9.9, 28.9] | 0.61 (15%) [0.44, 0.79] | 95 (44%) [32, 178] | 4.1 (46%) [1.3, 8.1] | 2.1 (53%) [0.9, 5.2] |
| Adult Subjects# (N= 29) | 12.5 (21%) [8.2, 19.3] | 0.65 (16%) [0.45, 0.84] | 91 (33%) [53, 155] | 4.9 (35%) [1.8, 8.3] | 1.7 (34%) [0.9, 3.3] |
Cmax = Maximum plasma concentration; Vss= Volume of distribution; AUC = Area under concentration-time curve; t1/2 = Apparent elimination half-life; CL = Systemic clearance normalized for body weight
* AUC = Single dose AUC0–∞
† In this data set, "pre-term" is defined as <34 weeks gestational age (Note: Only 1 patient enrolled was preterm with a postnatal age between 1 week and 28 days)
‡ Dose of 10 mg/kg
§ In this data set, "full-term" is defined as ≥34 weeks gestational age
¶ Dose of 600 mg or 10 mg/kg up to a maximum of 600 mg
# Dose normalized to 600 mg
Gender
Females have a slightly lower volume of distribution of linezolid than males. Plasma concentrations are higher in females than in males, which is partly due to body weight differences. After a 600-mg dose, mean oral clearance is approximately 38% lower in females than in males. However, there are no significant gender differences in mean apparent elimination-rate constant or half-life. Thus, drug exposure in females is not expected to substantially increase beyond levels known to be well tolerated. Therefore, dose adjustment by gender does not appear to be necessary.
Renal Impairment
The pharmacokinetics of the parent drug, linezolid, are not altered in patients with any degree of renal impairment; however, the two primary metabolites of linezolid accumulate in patients with renal impairment, with the amount of accumulation increasing with the severity of renal dysfunction (see Table 10). The pharmacokinetics of linezolid and its two metabolites have also been studied in patients with end-stage renal disease (ESRD) receiving hemodialysis. In the ESRD study, 14 patients were dosed with linezolid 600 mg every 12 hours for 14.5 days (see Table 11). Because similar plasma concentrations of linezolid are achieved regardless of renal function, no dose adjustment is recommended for patients with renal impairment. However, given the absence of information on the clinical significance of accumulation of the primary metabolites, use of linezolid in patients with renal impairment should be weighed against the potential risks of accumulation of these metabolites. Both linezolid and the two metabolites are eliminated by hemodialysis. No information is available on the effect of peritoneal dialysis on the pharmacokinetics of linezolid. Approximately 30% of a dose was eliminated in a 3-hour hemodialysis session beginning 3 hours after the dose of linezolid was administered; therefore, linezolid should be given after hemodialysis.
Table 10. Mean (Standard Deviation) AUCs and Elimination Half-lives of Linezolid and Metabolites A and B in Patients with Varying Degrees of Renal Impairment After a Single 600 mg Oral Dose of Linezolid:
| Parameter | Healthy Subjects CLCR > 80 mL/min | Moderate Renal Impairment 30 < CLCR < 80 mL/min | Severe Renal Impairment 10 < CL CR < 30 mL/min |
|---|---|---|---|
| LINEZOLID | |||
| AUC0–∞, mcg h/mL | 110 (22) | 128 (53) | 127 (66) |
| t1/2, hours | 6.4 (2.2) | 6.1 (1.7) | 7.1 (3.7) |
| METABOLITE A | |||
| AUC0–48, mcg h/mL | 7.6 (1.9) | 11.7 (4.3) | 56.5 (30.6) |
| t 1/2, hours | 6.3 (2.1) | 6.6 (2.3) | 9.0 (4.6) |
| METABOLITE B* | |||
| AUC0–48, mcg h/mL | 30.5 (6.2) | 51.1 (38.5) | 203 (92) |
| t1/2, hours | 6.6 (2.7) | 9.9 (7.4) | 11.0 (3.9) |
* Metabolite B is the major metabolite of linezolid.
Table 11. Mean (Standard Deviation) AUCs and Elimination Half-lives of Linezolid and Metabolites A and B in Subjects with End-Stage Renal Disease (ESRD) After the Administration of 600 mg Linezolid Every 12 Hours for 14.5 Days:
| Parameter | ESRD Subjects* |
|---|---|
| LINEZOLID | |
| AUC0–12, mcg h/mL (after last dose) | 181 (52.3) |
| t1/2, h (after last dose) | 8.3 (2.4) |
| METABOLITE A | |
| AUC0–12, mcg h/mL (after last dose) | 153 (40.6) |
| t1/2, h (after last dose) | 15.9 (8.5) |
| METABOLITE B† | |
| AUC0–12, mcg h/mL (after last dose) | 356 (99.7) |
| t1/2, h (after last dose) | 34.8 (23.1) |
* between hemodialysis sessions
† Metabolite B is the major metabolite of linezolid.
Hepatic Impairment
The pharmacokinetics of linezolid are not altered in patients (n=7) with mild-to-moderate hepatic impairment (Child-Pugh class A or B). On the basis of the available information, no dose adjustment is recommended for patients with mild-to-moderate hepatic impairment. The pharmacokinetics of linezolid in patients with severe hepatic impairment have not been evaluated.
Excretion
Nonrenal clearance accounts for approximately 65% of the total clearance of linezolid. Under steady-state conditions, approximately 30% of the dose appears in the urine as linezolid, 40% as metabolite B, and 10% as metabolite A. The mean renal clearance of linezolid is 40 mL/min which suggests net tubular reabsorption. Virtually no linezolid appears in the feces, while approximately 6% of the dose appears in the feces as metabolite B, and 3% as metabolite A.
A small degree of nonlinearity in clearance was observed with increasing doses of linezolid, which appears to be due to lower renal and nonrenal clearance of linezolid at higher concentrations. However, the difference in clearance was small and was not reflected in the apparent elimination half-life.
Drugs Metabolized by Cytochrome P450
Linezolid is not an inducer of cytochrome P450 (CYP450) in rats. In addition, linezolid does not inhibit the activities of clinically significant human CYP isoforms (e.g., 1A2, 2C9, 2C19, 2D6, 2E1, 3A4). Therefore, linezolid is not expected to affect the pharmacokinetics of other drugs metabolized by these major enzymes. Concurrent administration of linezolid does not substantially alter the pharmacokinetic characteristics of (S)-warfarin, which is extensively metabolized by CYP2C9. Drugs such as warfarin and phenytoin, which are CYP2C9 substrates, may be given with linezolid without changes in dosage regimen.
Antibiotics
Aztreonam: The pharmacokinetics of linezolid or aztreonam are not altered when administered together.
Gentamicin: The pharmacokinetics of linezolid or gentamicin are not altered when administered together.
Antioxidants
The potential for drug-drug interactions with linezolid and the antioxidants Vitamin C and Vitamin E was studied in healthy volunteers. Subjects were administered a 600 mg oral dose of linezolid on Day 1, and another 600 mg dose of linezolid on Day 8. On Days 2–9, subjects were given either Vitamin C (1000 mg/day) or Vitamin E (800 IU/ day). The AUC0–∞ of linezolid increased 2.3% when co-administered with Vitamin C and 10.9% when co-administered with Vitamin E. No linezolid dose adjustment is recommended during co-administration with Vitamin C or Vitamin E.
Strong CYP 3A4 Inducers
Rifampin: The effect of rifampin on the pharmacokinetics of linezolid was evaluated in a study of 16 healthy adult males. Volunteers were administered oral linezolid 600 mg twice daily for 5 doses with and without rifampin 600 mg once daily for 8 days. Co-administration of rifampin with linezolid resulted in a 21% decrease in linezolid C max [90% CI, 15%-27%] and a 32% decrease in linezolid AUC 0-12 [90% CI, 27%-37%]. The clinical significance of this interaction is unknown. The mechanism of this interaction is not fully understood and may be related to the induction of hepatic enzymes. Other strong inducers of hepatic enzymes (e.g. carbamazepine, phenytoin, phenobarbital) could cause a similar or smaller decrease in linezolid exposure.
Monoamine Oxidase Inhibition
Linezolid is a reversible, nonselective inhibitor of monoamine oxidase. Therefore, linezolid has the potential for interaction with adrenergic and serotonergic agents.
Adrenergic Agents
Some individuals receiving ZYVOX may experience a reversible enhancement of the pressor response to indirect-acting sympathomimetic agents, vasopressor or dopaminergic agents. Commonly used drugs such as phenylpropanolamine and pseudoephedrine have been specifically studied. Initial doses of adrenergic agents, such as dopamine or epinephrine, should be reduced and titrated to achieve the desired response.
Tyramine: A significant pressor response has been observed in normal adult subjects receiving linezolid and tyramine doses of more than 100 mg. Therefore, patients receiving linezolid need to avoid consuming large amounts of foods or beverages with high tyramine content [see Patient Counseling Information (17)].
Pseudoephedrine HCl or phenylpropanolamine HCl: A reversible enhancement of the pressor response of either pseudoephedrine HCl (PSE) or phenylpropanolamine HCl (PPA) is observed when linezolid is administered to healthy normotensive subjects [see Warnings and Precautions (5.6) and Drug Interactions (7)]. A similar study has not been conducted in hypertensive patients. The interaction studies conducted in normotensive subjects evaluated the blood pressure and heart rate effects of placebo, PPA or PSE alone, linezolid alone, and the combination of steady-state linezolid (600 mg every 12 hours for 3 days) with two doses of PPA (25 mg) or PSE (60 mg) given 4 hours apart. Heart rate was not affected by any of the treatments. Blood pressure was increased with both combination treatments. Maximum blood pressure levels were seen 2 to 3 hours after the second dose of PPA or PSE, and returned to baseline 2 to 3 hours after peak. The results of the PPA study follow, showing the mean (and range) maximum systolic blood pressure in mm Hg: placebo = 121 (103 to 158); linezolid alone = 120 (107 to 135); PPA alone = 125 (106 to 139); PPA with linezolid = 147 (129 to 176). The results from the PSE study were similar to those in the PPA study. The mean maximum increase in systolic blood pressure over baseline was 32 mm Hg (range: 20-52 mm Hg) and 38 mm Hg (range: 18–79 mm Hg) during co-administration of linezolid with pseudoephedrine or phenylpropanolamine, respectively.
Serotonergic Agents
Dextromethorphan: The potential drug-drug interaction with dextromethorphan was studied in healthy volunteers. Subjects were administered dextromethorphan (two 20-mg doses given 4 hours apart) with or without linezolid. No serotonin syndrome effects (confusion, delirium, restlessness, tremors, blushing, diaphoresis, hyperpyrexia) have been observed in normal subjects receiving linezolid and dextromethorphan.
12.4. Microbiology
Mechanism of Action
Linezolid is a synthetic antibacterial agent of the oxazolidinone class, which has clinical utility in the treatment of infections caused by aerobic Gram-positive bacteria. The in vitro spectrum of activity of linezolid also includes certain Gram-negative bacteria and anaerobic bacteria. Linezolid binds to a site on the bacterial 23S ribosomal RNA of the 50S subunit and prevents the formation of a functional 70S initiation complex, which is essential for bacterial reproduction. The results of time-kill studies have shown linezolid to be bacteriostatic against enterococci and staphylococci. For streptococci, linezolid was found to be bactericidal for the majority of isolates.
Mechanisms of Resistance
In vitro studies have shown that point mutations in the 23S rRNA are associated with linezolid resistance. Reports of vancomycin-resistant Enterococcus faecium becoming resistant to linezolid during its clinical use have been published. There are reports of Staphylococcus aureus (methicillin-resistant) developing resistance to linezolid during clinical use. The linezolid resistance in these organisms is associated with a point mutation in the 23S rRNA (substitution of thymine for guanine at position 2576) of the organism. Organisms resistant to oxazolidinones via mutations in chromosomal genes encoding 23S rRNA or ribosomal proteins (L3 and L4) are generally cross-resistant to linezolid. Also linezolid resistance in staphylococci mediated by the enzyme methyltransferase has been reported. This resistance is mediated by the cfr (chloramphenicol-florfenicol) gene located on a plasmid which is transferable between staphylococci.
Interaction with Other Antimicrobial Drugs
In vitro studies have demonstrated additivity or indifference between linezolid and vancomycin, gentamicin, rifampin, imipenem-cilastatin, aztreonam, ampicillin, or streptomycin.
Linezolid has been shown to be active against most isolates of the following microorganisms, both in vitro and in clinical infections [see Indications and Usage (1)].
Gram-positive bacteria
Enterococcus faecium (vancomycin-resistant isolates only)
Staphylococcus aureus (including methicillin-resistant isolates)
Streptococcus agalactiae
Streptococcus pneumoniae
Streptococcus pyogenes
The following in vitro data are available, but their clinical significance is unknown. Greater than 90% of the following bacteria exhibit an in vitro MIC less than or equal to the linezolid-susceptible breakpoint for organisms of similar genus shown in Table 12. The safety and effectiveness of linezolid in treating clinical infections due to these bacteria have not been established in adequate and well-controlled clinical trials.
Gram-positive bacteria
Enterococcus faecalis (including vancomycin-resistant isolates)
Enterococcus faecium (vancomycin-susceptible isolates)
Staphylococcus epidermidis (including methicillin-resistant isolates)
Staphylococcus haemolyticus
Viridans group streptococci
Gram-negative bacteria
Pasteurella multocida
Susceptibility Test Methods
When available, the clinical microbiology laboratory should provide the results of in vitro susceptibility test results for antimicrobial drug products used in local hospitals and practice areas to the physician as periodic reports that describe the susceptibility profile of nosocomial and community-acquired pathogens. These reports should aid the physician in selecting an antibacterial drug product for treatment.
Dilution techniques
Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized method 1,2 (broth and/or agar). The MIC values should be interpreted according to criteria provided in Table 12.
Diffusion techniques
Quantitative methods that require measurement of zone diameters can also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. The zone size provides an estimate of the susceptibility of bacteria to antimicrobial compounds. The zone size should be determined using a standardized test method 2,3. This procedure uses paper disks impregnated with 30 mcg linezolid to test the susceptibility of bacteria to linezolid. The disk diffusion interpretive criteria are provided in Table 12.
Table 12. Susceptibility Test Interpretive Criteria for Linezolid:
| Pathogen | Susceptibility Interpretive Criteria | |||||
|---|---|---|---|---|---|---|
| Minimal Inhibitory Concentrations (MIC in mcg/mL) | Disk Diffusion (Zone Diameters in mm) | |||||
| S | I | R | S | I | R | |
| Enterococcus spp | ≤2 | 4 | ≥8 | ≥23 | 21-22 | ≤20 |
| Staphylococcus spp^†^ | ≤4 | --- | ≥8 | ≥21 | --- | ≤20 |
| Streptococcus pneumoniae† | ≤2 | --- | --- | ≥21 | --- | --- |
| Streptococcus spp other than S pneumoniae† | ≤2 | --- | --- | ≥21 | --- | --- |
S=susceptible, I=intermediate, R=resistant
* For disk diffusion testing of staphylococcal species, petri plates should be held up to the light source and read with transmitted light. The zone margin should be considered the area showing no obvious, visible growth that can be detected with the unaided eye. Ignore faint growth of tiny colonies that can be detected only with a magnifying lens at the edge of the zone of inhibited growth. Any discernible growth within the zone of inhibition is indicative of resistance. Resistant results obtained by the disk diffusion method should be confirmed using an MIC method
† The current absence of data on resistant isolates precludes defining any categories other than "Susceptible." Isolates yielding test results suggestive of a "nonsusceptible" category should be retested, and if the result is confirmed, the isolate should be submitted to a reference laboratory for further testing.
A report of "Susceptible" indicates that the antimicrobial drug is likely to inhibit growth of the pathogen if the antimicrobial drug reaches the concentration usually achievable at the site of infection. A report of "Intermediate" indicates that the result should be considered equivocal, and, if the bacteria is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug product is physiologically concentrated or in situations where a high dosage of the drug product can be used. This category also provides a buffer zone that prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of "Resistant" indicates that the antimicrobial is not likely to inhibit growth of the pathogen if the antimicrobial drug reaches the concentration usually achievable at the site of infection; other therapy should be selected.
Quality Control
Standardized susceptibility test procedures require the use of laboratory controls to monitor and ensure the accuracy and precision of supplies and reagents used in the assay, and the techniques of the individuals performing the test 1,2,3. Standard linezolid powder should provide the following range of MIC values noted in Table 13. For the diffusion technique using the 30 mcg linezolid disk, the criteria in Table 13 should be achieved.
Table 13. Acceptable Quality Control Ranges for Linezolid:
| Minimum Inhibitory Ranges (MIC in mcg/mL) | Disk Diffusion Ranges Zone Diameters (mm) | |
|---|---|---|
| Enterococcus faecalis ATCC 29212 | 1-4 | Not applicable |
| Staphylococcus aureus ATCC 29213 | 1-4 | Not applicable |
| Staphylococcus aureus ATCC 25923 | Not applicable | 25-32 |
| Streptococcus pneumoniae ATCC 49619 ?footnote? | 0.25-2 | 25-34 |
* This organism may be used for validation of susceptibility test results when testing Streptococcus spp. other than S. pneumoniae.
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Lifetime studies in animals have not been conducted to evaluate the carcinogenic potential of linezolid. Neither mutagenic nor clastogenic potential was found in a battery of tests including: assays for mutagenicity (Ames bacterial reversion and CHO cell mutation), an in vitro unscheduled DNA synthesis (UDS) assay, an in vitro chromosome aberration assay in human lymphocytes, and an in vivo mouse micronucleus assay.
Linezolid did not affect the fertility or reproductive performance of adult female rats. It reversibly decreased fertility and reproductive performance in adult male rats when given at doses ≥ 50 mg/kg/day, with exposures approximately equal to or greater than the expected human exposure level (exposure comparisons are based on AUCs). The reversible fertility effects were mediated through altered spermatogenesis. Affected spermatids contained abnormally formed and oriented mitochondria and were non-viable. Epithelial cell hypertrophy and hyperplasia in the epididymis was observed in conjunction with decreased fertility. Similar epididymal changes were not seen in dogs.
In sexually mature male rats exposed to drug as juveniles, mildly decreased fertility was observed following treatment with linezolid through most of their period of sexual development (50 mg/kg/day from days 7 to 36 of age, and 100 mg/kg/day from days 37 to 55 of age), with exposures up to 1.7-fold greater than mean AUCs observed in pediatric patients aged 3 months to 11 years. Decreased fertility was not observed with shorter treatment periods, corresponding to exposure in utero through the early neonatal period (gestation day 6 through postnatal day 5), neonatal exposure (postnatal days 5 to 21), or to juvenile exposure (postnatal days 22 to 35). Reversible reductions in sperm motility and altered sperm morphology were observed in rats treated from postnatal day 22 to 35.
13.2. Animal Toxicology and/or Pharmacology
Target organs of linezolid toxicity were similar in juvenile and adult rats and dogs. Dose- and time-dependent myelosuppression, as evidenced by bone marrow hypocellularity/decreased hematopoiesis, decreased extramedullary hematopoiesis in spleen and liver, and decreased levels of circulating erythrocytes, leukocytes, and platelets have been seen in animal studies. Lymphoid depletion occurred in thymus, lymph nodes, and spleen. Generally, the lymphoid findings were associated with anorexia, weight loss, and suppression of body weight gain, which may have contributed to the observed effects.
In rats administered linezolid orally for 6 months, non-reversible, minimal to mild axonal degeneration of sciatic nerves was observed at 80 mg/kg/day; minimal degeneration of the sciatic nerve was also observed in 1 male at this dose level at a 3-month interim necropsy. Sensitive morphologic evaluation of perfusion-fixed tissues was conducted to investigate evidence of optic nerve degeneration. Minimal to moderate optic nerve degeneration was evident in 2 male rats after 6 months of dosing, but the direct relationship to drug was equivocal because of the acute nature of the finding and its asymmetrical distribution. The nerve degeneration observed was microscopically comparable to spontaneous unilateral optic nerve degeneration reported in aging rats and may be an exacerbation of common background change.
These effects were observed at exposure levels that are comparable to those observed in some human subjects. The hematopoietic and lymphoid effects were reversible, although in some studies, reversal was incomplete within the duration of the recovery period.
14. Clinical Studies
14.1 Adults
Nosocomial Pneumonia
Adult patients with clinically and radiologically documented nosocomial pneumonia were enrolled in a randomized, multi-center, double-blind trial. Patients were treated for 7 to 21 days. One group received ZYVOX I.V. Injection 600 mg every 12 hours, and the other group received vancomycin 1 g every 12 hours intravenously. Both groups received concomitant aztreonam (1 to 2 g every 8 hours intravenously), which could be continued if clinically indicated. There were 203 linezolid-treated and 193 vancomycin-treated patients enrolled in the study. One hundred twenty-two (60%) linezolid-treated patients and 103 (53%) vancomycin-treated patients were clinically evaluable. The cure rates in clinically evaluable patients were 57% for linezolid-treated patients and 60% for vancomycin-treated patients. The cure rates in clinically evaluable patients with ventilator-associated pneumonia were 47% for linezolid-treated patients and 40% for vancomycin-treated patients. A modified intent-to-treat (MITT) analysis of 94 linezolid-treated patients and 83 vancomycin-treated patients included subjects who had a pathogen isolated before treatment. The cure rates in the MITT analysis were 57% in linezolid-treated patients and 46% in vancomycin-treated patients. The cure rates by pathogen for microbiologically evaluable patients are presented in Table 14.
Table 14. Cure Rates at the Test-of-Cure Visit for Microbiologically Evaluable Adult Patients with Nosocomial Pneumonia:
| Pathogen | Cured | |
|---|---|---|
| ZYVOX n/N (%) | Vancomycin n/N (%) | |
| Staphylococcus aureus | 23/38 (61) | 14/23 (61) |
| Methicillin-resistant S. aureus | 13/22 (59) | 7/10 (70) |
| Streptococcus pneumoniae | 9/9 (100) | 9/10 (90) |
Complicated Skin and Skin Structure Infections
Adult patients with clinically documented complicated skin and skin structure infections were enrolled in a randomized, multi-center, double-blind, double-dummy trial comparing study medications administered intravenously followed by medications given orally for a total of 10 to 21 days of treatment. One group of patients received ZYVOX I.V. Injection 600 mg every 12 hours followed by ZYVOX Tablets 600 mg every 12 hours; the other group received oxacillin 2 g every 6 hours intravenously followed by dicloxacillin 500 mg every 6 hours orally. Patients could receive concomitant aztreonam if clinically indicated. There were 400 linezolid-treated and 419 oxacillin-treated patients enrolled in the study. Two hundred forty-five (61%) linezolid-treated patients and 242 (58%) oxacillin-treated patients were clinically evaluable. The cure rates in clinically evaluable patients were 90% in linezolid-treated patients and 85% in oxacillin-treated patients. A modified intent-to-treat (MITT) analysis of 316 linezolid-treated patients and 313 oxacillin-treated patients included subjects who met all criteria for study entry. The cure rates in the MITT analysis were 86% in linezolid-treated patients and 82% in oxacillin-treated patients. The cure rates by pathogen for microbiologically evaluable patients are presented in Table 15.
Table 15. Cure Rates at the Test-of-Cure Visit for Microbiologically Evaluable Adult Patients with Complicated Skin and Skin Structure Infections:
| Pathogen | Cured | |
|---|---|---|
| ZYVOX n/N (%) | Oxacillin/Dicloxacillin n/N (%) | |
| Staphylococcus aureus | 73/83 (88) | 72/84 (86) |
| Methicillin-resistant S. aureus | ⅔ (67) | 0/0 (-) |
| Streptococcus agalactiae | 6/6 (100) | 3/6 (50) |
| Streptococcus pyogenes | 18/26 (69) | 21/28 (75) |
A separate study provided additional experience with the use of ZYVOX in the treatment of methicillin-resistant Staphylococcus aureus (MRSA) infections. This was a randomized, open-label trial in hospitalized adult patients with documented or suspected MRSA infection.
One group of patients received ZYVOX I.V. Injection 600 mg every 12 hours followed by ZYVOX Tablets 600 mg every 12 hours. The other group of patients received vancomycin 1 g every 12 hours intravenously. Both groups were treated for 7 to 28 days, and could receive concomitant aztreonam or gentamicin if clinically indicated. The cure rates in microbiologically evaluable patients with MRSA skin and skin structure infection were 26/33 (79%) for linezolid-treated patients and 24/33 (73%) for vancomycin-treated patients.
Diabetic Foot Infections
Adult diabetic patients with clinically documented complicated skin and skin structure infections ("diabetic foot infections") were enrolled in a randomized (2:1 ratio), multi-center, open-label trial comparing study medications administered intravenously or orally for a total of 14 to 28 days of treatment. One group of patients received ZYVOX 600 mg every 12 hours intravenously or orally; the other group received ampicillin/sulbactam 1.5 to 3 g intravenously or amoxicillin/clavulanate 500 to 875 mg every 8 to 12 hours orally. In countries where ampicillin/sulbactam is not marketed, amoxicillin/clavulanate 500 mg to 2 g every 6 hours was used for the intravenous regimen. Patients in the comparator group could also be treated with vancomycin 1 g every 12 hours intravenously if MRSA was isolated from the foot infection. Patients in either treatment group who had Gram-negative bacilli isolated from the infection site could also receive aztreonam 1 to 2 g every 8–12 hours intravenously. All patients were eligible to receive appropriate adjunctive treatment methods, such as debridement and off-loading, as typically required in the treatment of diabetic foot infections, and most patients received these treatments. There were 241 linezolid-treated and 120 comparator-treated patients in the intent-to-treat (ITT) study population. Two hundred twelve (86%) linezolid-treated patients and 105 (85%) comparator-treated patients were clinically evaluable. In the ITT population, the cure rates were 68.5% (165/241) in linezolid-treated patients and 64% (77/120) in comparator-treated patients, where those with indeterminate and missing outcomes were considered failures. The cure rates in the clinically evaluable patients (excluding those with indeterminate and missing outcomes) were 83% (159/192) and 73% (74/101) in the linezolid- and comparator-treated patients, respectively. A critical post-hoc analysis focused on 121 linezolid-treated and 60 comparator-treated patients who had a Gram-positive pathogen isolated from the site of infection or from blood, who had less evidence of underlying osteomyelitis than the overall study population, and who did not receive prohibited antimicrobials. Based upon that analysis, the cure rates were 71% (86/121) in the linezolid-treated patients and 63% (38/60) in the comparator-treated patients. None of the above analyses were adjusted for the use of adjunctive therapies. The cure rates by pathogen for microbiologically evaluable patients are presented in Table 16.
Table 16. Cure Rates at the Test-of-Cure Visit for Microbiologically Evaluable Adult Patients with Diabetic Foot Infections:
| Pathogen | Cured | |
|---|---|---|
| ZYVOX n/N (%) | Comparator n/N (%) | |
| Staphylococcus aureus | 49/63 (78) | 20/29 (69) |
| Methicillin-resistant S. aureus | 12/17 (71) | ⅔ (67) |
| Streptococcus agalactiae | 25/29 (86) | 9/16 (56) |
Vancomycin-Resistant Enterococcal Infections
Adult patients with documented or suspected vancomycin-resistant enterococcal infection were enrolled in a randomized, multi-center, double-blind trial comparing a high dose of ZYVOX (600 mg) with a low dose of ZYVOX (200 mg) given every 12 hours either intravenously (IV) or orally for 7 to 28 days. Patients could receive concomitant aztreonam or aminoglycosides. There were 79 patients randomized to high-dose linezolid and 66 to low-dose linezolid. The intent-to-treat (ITT) population with documented vancomycin-resistant enterococcal infection at baseline consisted of 65 patients in the high-dose arm and 52 in the low-dose arm.
The cure rates for the ITT population with documented vancomycin-resistant enterococcal infection at baseline are presented in Table 17 by source of infection. These cure rates do not include patients with missing or indeterminate outcomes. The cure rate was higher in the high-dose arm than in the low-dose arm, although the difference was not statistically significant at the 0.05 level.
Table 17. Cure Rates at the Test-of-Cure Visit for ITT Adult Patients with Documented Vancomycin-Resistant Enterococcal Infections at Baseline
| Source of Infection | Cured | |
|---|---|---|
| ZYVOX 600 mg every 12 hours n/N (%) | ZYVOX 200 mg every 12 hours n/N (%) | |
| Any site | 39/58 (67) | 24/46 (52) |
| Any site with associated bacteremia | 10/17 (59) | 4/14 (29) |
| Bacteremia of unknown origin | 5/10 (50) | 2/7 (29) |
| Skin and skin structure | 9/13 (69) | 5/5 (100) |
| Urinary tract | 12/19 (63) | 12/20 (60) |
| Pneumonia | ⅔ (67) | 0/1 (0) |
| Other* | 11/13 (85) | 5/13 (39) |
* Includes sources of infection such as hepatic abscess, biliary sepsis, necrotic gall bladder, pericolonic abscess, pancreatitis, and catheter-related infection.
14.2 Pediatric Patients
Infections due to Gram-positive Bacteria
A safety and efficacy study provided experience on the use of ZYVOX in pediatric patients for the treatment of nosocomial pneumonia, complicated skin and skin structure infections, and other infections due to Gram-positive bacterial pathogens, including methicillin-resistant and -susceptible Staphylococcus aureus and vancomycin-resistant Enterococcus faecium. Pediatric patients ranging in age from birth through 11 years with infections caused by the documented or suspected Gram-positive bacteria were enrolled in a randomized, open-label, comparator-controlled trial. One group of patients received ZYVOX I.V. Injection 10 mg/kg every 8 hours followed by ZYVOX for Oral Suspension 10 mg/kg every 8 hours. A second group received vancomycin 10 to 15 mg/kg intravenously every 6 to 24 hours, depending on age and renal clearance. Patients who had confirmed VRE infections were placed in a third arm of the study and received ZYVOX 10 mg/kg every 8 hours intravenously and/or orally. All patients were treated for a total of 10 to 28 days and could receive concomitant Gram-negative antibiotics if clinically indicated. In the intent-to-treat (ITT) population, there were 206 patients randomized to linezolid and 102 patients randomized to vancomycin. The cure rates for ITT, MITT, and clinically evaluable patients are presented in Table 18. After the study was completed, 13 additional patients ranging from 4 days through 16 years of age were enrolled in an open-label extension of the VRE arm of the study. Table 19 provides clinical cure rates by pathogen for microbiologically evaluable patients including microbiologically evaluable patients with vancomycin-resistant Enterococcus faecium from the extension of this study.
Table 18. Cure Rates at the Test-of-Cure Visit for Intent-to-Treat, Modified Intent-to-Treat, and Clinically Evaluable Pediatric Patients for the Overall Population and by Select Baseline Diagnosis:
| Population | ITT | MITT* | Clinically Evaluable | |||
|---|---|---|---|---|---|---|
| ZYVOX n/N (%) | Vancomycin n/N (%) | ZYVOX n/N (%) | Vancomycin n/N (%) | ZYVOX n/N (%) | Vancomycin n/N (%) | |
| Any diagnosis | 150/186 (81) | 69/83 (83) | 86/108 (80) | 44/49 (90) | 106/117 (91) | 49/54 (91) |
| Complicated skin and skin structure infections | 61/72 (85) | 31/34 (91) | 37/43 (86) | 22/23 (96) | 46/49 (94) | 26/27 (96) |
| Nosocomial pneumonia | 13/18 (72) | 11/12 (92) | 5/6 (83) | 4/4 (100) | 7/7 (100) | 5/5 (100) |
* MITT = ITT patients with an isolated Gram-positive pathogen at baseline
Table 19. Cure Rates at the Test-of-Cure Visit for Microbiologically Evaluable Pediatric Patients with Infections due to Gram-positive Pathogens:
| Pathogen | Microbiologically Evaluable | |
|---|---|---|
| ZYVOX n/N (%) | Vancomycin n/N (%) | |
| Vancomycin-resistant Enterococcus faecium | 6/8 (75)* | 0/0 (-) |
| Staphylococcus aureus | 36/38 (95) | 23/24 (96) |
| Methicillin-resistant S. aureus | 16/17 (94) | 9/9 (100) |
| Streptococcus pyogenes | 2/2 (100) | ½ (50) |
* Includes data from 7 patients enrolled in the open-label extension of this study.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.