Pomalidomide
Chemical formula: C₁₃H₁₁N₃O₄ Molecular mass: 273.244 g/mol PubChem compound: 134780
Interactions
Pomalidomide interacts in the following cases:
CYP1A2 inhibitors, CYP3A4/5 inhibitors
Pomalidomide is partly metabolised by CYP1A2 and CYP3A4/5. It is also a substrate for P-glycoprotein. Co-administration of pomalidomide with the strong CYP3A4/5 and P-gp inhibitor ketoconazole, or the strong CYP3A4/5 inducer carbamazepine, had no clinically relevant effect on exposure to pomalidomide. Co-administration of the strong CYP1A2 inhibitor fluvoxamine with pomalidomide in the presence of ketoconazole, increased mean exposure to pomalidomide by 107% with a 90% confidence interval [91% to 124%] compared to pomalidomide plus ketoconazole. In a second study to evaluate the contribution of a CYP1A2 inhibitor alone to metabolism changes, co-administration of fluvoxamine alone with pomalidomide increased mean exposure to pomalidomide by 125% with a 90% confidence interval [98% to 157%] compared to pomalidomide alone. If strong inhibitors of CYP1A2 (e.g. ciprofloxacin, enoxacin and fluvoxamine) are co-administered with pomalidomide, reduce the dose of pomalidomide by 50%.
Hepatic impairment
Patients with serum total bilirubin >1.5 x ULN (upper limit of normal range)were excluded from clinical studies. Hepatic impairment has a modest effect on the pharmacokinetics of pomalidomide. No adjustment of the starting dose of pomalidomide is required for patients with hepatic impairment as defined by the Child-Pugh criteria. However, patients with hepatic impairment should be carefully monitored for adverse reactions and dose reduction or interruption of pomalidomide should be used as needed.
Fertility
Pomalidomide was found to impact negatively on fertility and be teratogenic in animals. Pomalidomide crossed the placenta and was detected in foetal blood following administration to pregnant rabbits.
Interstitial lung disease (ILD)
ILD and related events, including cases of pneumonitis, have been observed with pomalidomide. Careful assessment of patients with an acute onset or unexplained worsening of pulmonary symptoms should be performed to exclude ILD. Pomalidomide should be interrupted pending investigation of these symptoms and if ILD is confirmed, appropriate treatment should be initiated. Pomalidomide should only be resumed after a thorough evaluation of the benefits and the risks.
Hepatitis
Markedly elevated levels of alanine aminotransferase and bilirubin have been observed in patients treated with pomalidomide. There have also been cases of hepatitis that resulted in discontinuation of pomalidomide. Regular monitoring of liver function is recommended for the first 6 months of treatment with pomalidomide and as clinically indicated thereafter.
Tumour lysis syndrome
Patients at greatest risk of tumour lysis syndrome are those with high tumour burden prior to treatment. These patients should be monitored closely and appropriate precautions taken.
Peripheral neuropathy
Patients with ongoing ≥ Grade 2 peripheral neuropathy were excluded from clinical studies with pomalidomide. Appropriate caution should be exercised when considering the treatment of such patients with pomalidomide.
Haemodialysis
On haemodialysis days, patients should take their pomalidomide dose following haemodialysis.
Venous thromboembolic events, arterial thrombotic events
Patients receiving pomalidomide either in combination with bortezomib and dexamethasone or in combination with dexamethasone have developed venous thromboembolic events (predominantly deep vein thrombosis and pulmonary embolism) and arterial thrombotic events (myocardial infarction and cerebrovascular accident). Patients with known risk factors for thromboembolism – including prior thrombosis – should be closely monitored. Action should be taken to try to minimise all modifiable risk factors (e.g. smoking, hypertension, and hyperlipidaemia). Patients and physicians are advised to be observant for the signs and symptoms of thromboembolism. Patients should be instructed to seek medical care if they develop symptoms such as shortness of breath, chest pain, arm or leg swelling.
Anticoagulation therapy (unless contraindicated) is recommended, (such as acetylsalicylic acid, warfarin, heparin or clopidogrel), especially in patients with additional thrombotic risk factors. A decision to take prophylactic measures should be made after a careful assessment of the individual patient's underlying risk factors. In clinical studies, patients received prophylactic acetylsalicylic acid or alternative antithrombotic therapy. The use of erythropoietic agents carries a risk of thrombotic events including thromboembolism. Therefore, erythropoietic agents, as well as other agents that may increase the risk of thromboembolic events, should be used with caution.
Non-melanoma skin cancer
Second primary malignancies, such as non-melanoma skin cancer, have been reported in patients receiving pomalidomide. Physicians should carefully evaluate patients before and during treatment using standard cancer screening for occurrence of second primary malignancies and institute treatment as indicated.
Reactivation of hepatitis B
Reactivation of hepatitis B has been reported rarely in patients receiving pomalidomide in combination with dexamethasone who have previously been infected with the hepatitis B virus (HBV). Some of these cases have progressed to acute hepatic failure, resulting in discontinuation of pomalidomide. Hepatitis B virus status should be established before initiating treatment with pomalidomide. For patients who test positive for HBV infection, consultation with a physician with expertise in the treatment of hepatitis B is recommended. Caution should be exercised when pomalidomide in combination with dexamethasone is used in patients previously infected with HBV, including patients who are anti-HBc positive but HBsAg negative. These patients should be closely monitored for signs and symptoms of active HBV infection throughout therapy.
Neutropenia, anaemia, thrombocytopenia
Neutropenia was the most frequently reported Grade 3 or 4 haematological adverse reaction in patients with relapsed/refractory multiple myeloma, followed by anaemia and thrombocytopenia. Patients should be monitored for haematological adverse reactions, especially neutropenia. Patients should be advised to report febrile episodes promptly. Physicians should observe patients for signs of bleeding including epistaxes, especially with use of concomitant medicinal products known to increase the risk of bleeding. Complete blood counts should be monitored at baseline, weekly for the first 8 weeks and monthly thereafter. A dose modification may be required. Patients may require use of blood product support and/or growth factors.
Dizziness, confusion
Dizziness and confusional state have been reported with pomalidomide. Patients must avoid situations where dizziness or confusion may be a problem and not to take other medicinal products that may cause dizziness or confusion without first seeking medical advice.
Cardiac disease
Patients with significant cardiac dysfunction (congestive heart failure [NY Heart Association Class III or IV]; myocardial infarction within 12 months of starting study; unstable or poorly controlled angina pectoris) were excluded from clinical studies with pomalidomide. Cardiac events, including congestive cardiac failure, pulmonary oedema and atrial fibrillation, have been reported, mainly in patients with pre-existing cardiac disease or cardiac risk factors.
Appropriate caution should be exercised when considering the treatment of such patients with pomalidomide, including periodic monitoring for signs or symptoms of cardiac events.
Angioedema, SJS, TEN, DRESS
Angioedema and severe dermatologic reactions including SJS, TEN and DRESS have been reported with the use of pomalidomide. Patients should be advised of the signs and symptoms of these reactions by their prescribers and should be told to seek medical attention immediately if they develop these symptoms. Pomalidomide must be discontinued for exfoliative or bullous rash, or if SJS, TEN or DRESS is suspected, and should not be resumed following discontinuation for these reactions. Patients with a prior history of serious allergic reactions associated with thalidomide or lenalidomide were excluded from clinical studies. Such patients may be at higher risk of hypersensitivity reactions and should not receive pomalidomide. Pomalidomide interruption or discontinuation should be considered for Grade 2-3 skin rash. Pomalidomide must be discontinued permanently for angioedema.
Pregnancy
A teratogenic effect of pomalidomide in humans is expected. Pomalidomide is contraindicated during pregnancy and in women of childbearing potential, except when all the conditions for pregnancy prevention have been met.
Nursing mothers
It is unknown whether pomalidomide is excreted in human milk. Pomalidomide was detected in milk of lactating rats following administration to the mother. Because of the potential for adverse reactions in breastfed infants from pomalidomide, a decision must be made whether to discontinue breast-feeding or to discontinue the medicinal product, taking into account the benefit of breast-feeding for the child and the benefit of the therapy for the woman.
Carcinogenesis, mutagenesis and fertility
Women of childbearing potential / Contraception in males and females
Women of childbearing potential should use effective method of contraception. If pregnancy occurs in a woman treated with pomalidomide, treatment must be stopped and the patient should be referred to a physician specialised or experienced in teratology for evaluation and advice. If pregnancy occurs in a partner of a male patient taking pomalidomide, it is recommended to refer the female partner to a physician specialised or experienced in teratology for evaluation and advice. Pomalidomide is present in human semen. As a precaution, all male patients taking pomalidomide should use condoms throughout treatment duration, during dose interruption and for 7 days after cessation of treatment if their partner is pregnant or of childbearing potential and has no contraception.
Fertility
Pomalidomide was found to impact negatively on fertility and be teratogenic in animals. Pomalidomide crossed the placenta and was detected in foetal blood following administration to pregnant rabbits.
Effects on ability to drive and use machines
Pomalidomide has minor or moderate influence on the ability to drive and use machines. Fatigue, depressed level of consciousness, confusion, and dizziness have been reported with the use of pomalidomide. If affected, patients should be instructed not to drive cars, use machines or perform hazardous tasks while being treated with pomalidomide.
Adverse reactions
Summary of the safety profile
Pomalidomide in combination with bortezomib and dexamethasone
The most commonly reported blood and lymphatic system disorders were neutropenia (46.8%), thrombocytopenia (36.7%) and anaemia (28.4%). The most frequently reported adverse reaction was peripheral sensory neuropathy (47.8%). The most commonly reported Grade 3 or 4 adverse reactions were blood and lymphatic system disorders including neutropenia (41.7%), thrombocytopenia (27.3%) and anaemia (14.0%). The most commonly reported serious adverse reaction was pneumonia (11.5%). Other serious adverse reactions reported included pyrexia (4.0%), lower respiratory tract infection (2.9%), pulmonary embolism (2.9%), influenza (2.9%), and acute kidney injury (2.9%).
Pomalidomide in combination with dexamethasone
The most commonly reported adverse reactions in clinical studies have been blood and lymphatic system disorders including anaemia (45.7%), neutropenia (45.3%) and thrombocytopenia (27%); in general disorders and administration site conditions including fatigue (28.3%), pyrexia (21%) and oedema peripheral (13%); and in infections and infestations including pneumonia (10.7%). Peripheral neuropathy adverse reactions were reported in 12.3% of patients and venous embolic or thrombotic (VTE) adverse reactions were reported in 3.3% of patients. The most commonly reported Grade 3 or 4 adverse reactions were in the blood and lymphatic system disorders including neutropenia (41.7%), anaemia (27%) and thrombocytopenia (20.7%); in infections and infestations including pneumonia (9%); and in general disorders and administration site conditions including fatigue (4.7%), pyrexia (3%) and oedema peripheral (1.3%). The most commonly reported serious adverse reaction was pneumonia (9.3%). Other serious adverse reactions reported included febrile neutropenia (4.0%), neutropenia (2.0%), thrombocytopenia (1.7%) and VTE adverse reactions (1.7%).
Adverse reactions tended to occur more frequently within the first 2 cycles of treatment with pomalidomide.
Tabulated list of adverse reactions
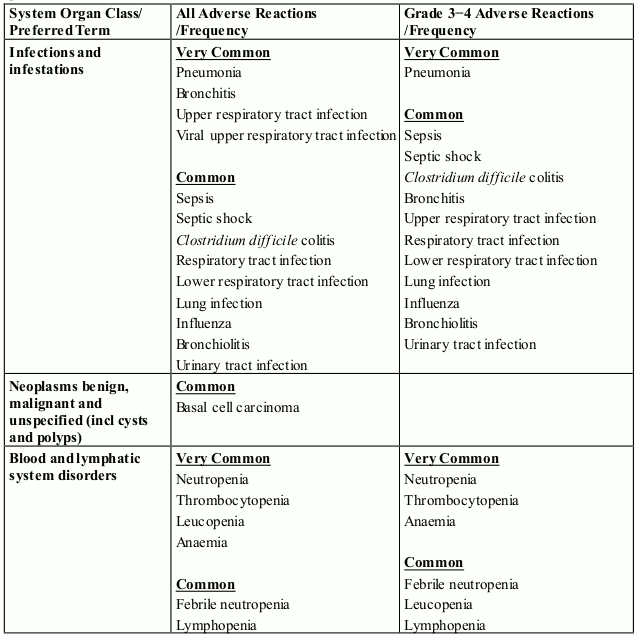
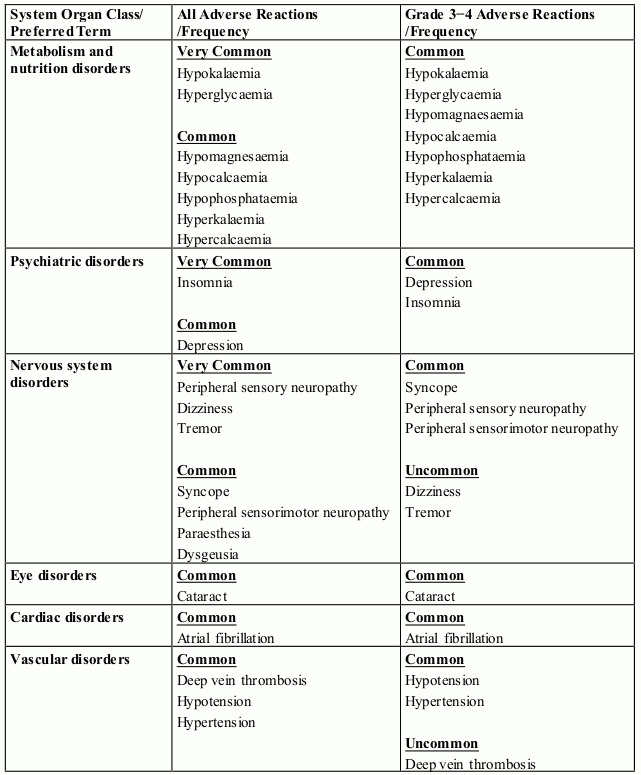
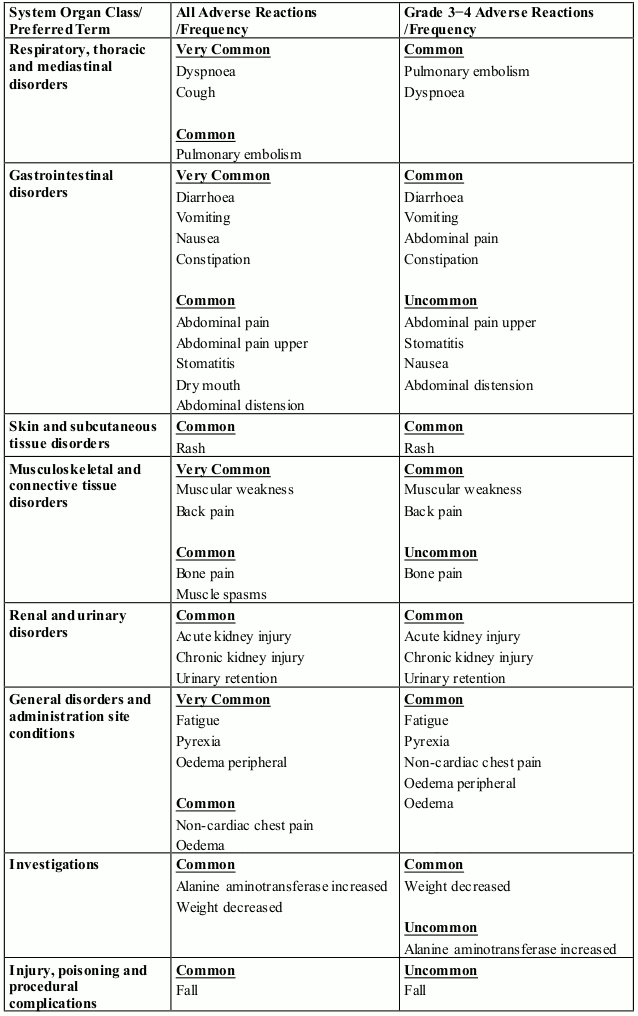
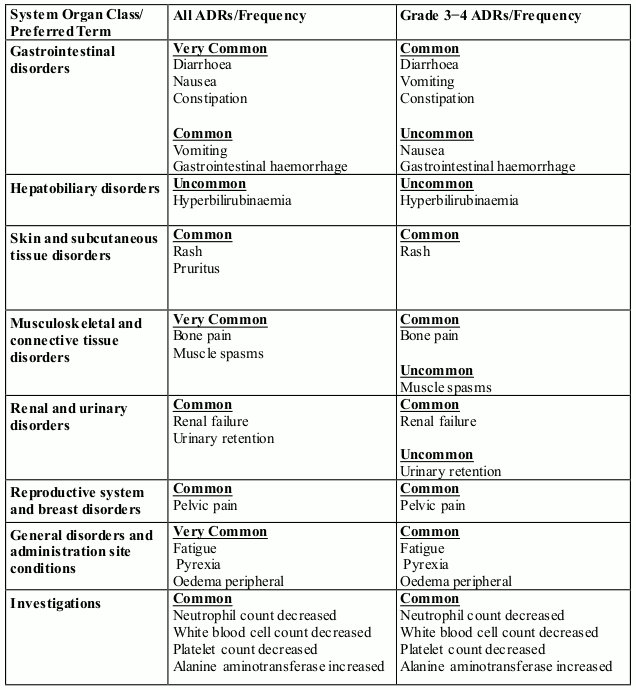
Pomalidomide in combination with bortezomib and dexamethasone
In randomised study CC-4047-MM-007, 278 patients received pomalidomide, bortezomib and dexamethasone (Pom+Btz+Dex arm).
The adverse reactions observed in patients treated with pomalidomide in combination with bortezomib and dexamethasone are listed in Table 1 by system organ class (SOC) and frequency for all adverse reactions and for Grade 3 or 4 adverse reactions.
Frequencies for Pom+Btz+Dex (any grade) are defined in accordance with current guidance, as: very common (≥1/10), common (≥1/100 to <1/10); and uncommon (≥1/1,000 to <1/100).
Table 1. All Adverse Reactions (ADRs) reported in clinical trial MM-007 in patients treated with pomalidomide in combination with bortezomib and dexamethasone:
Tabulated list of adverse reactions
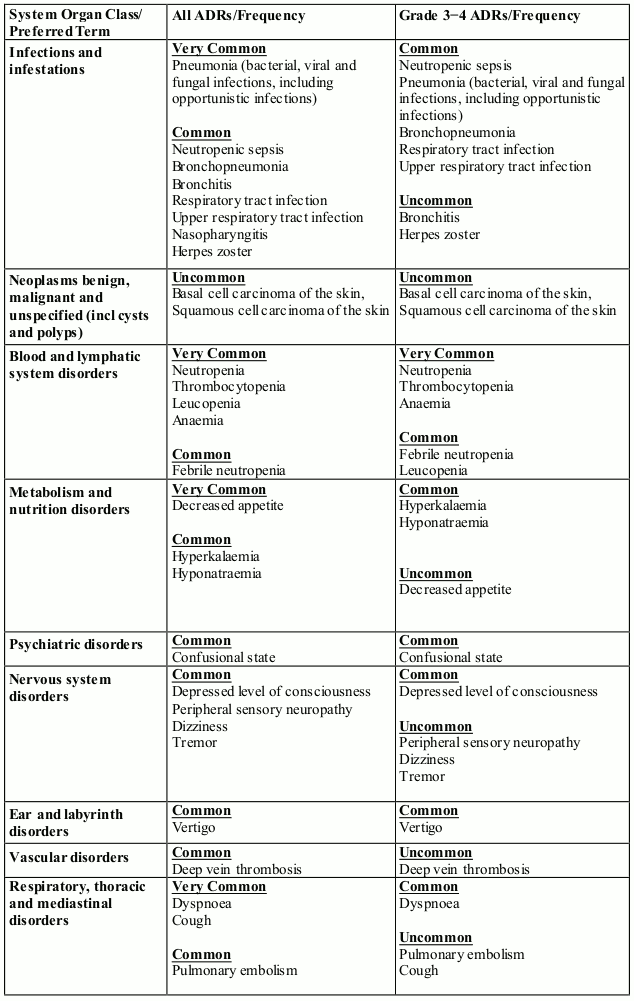
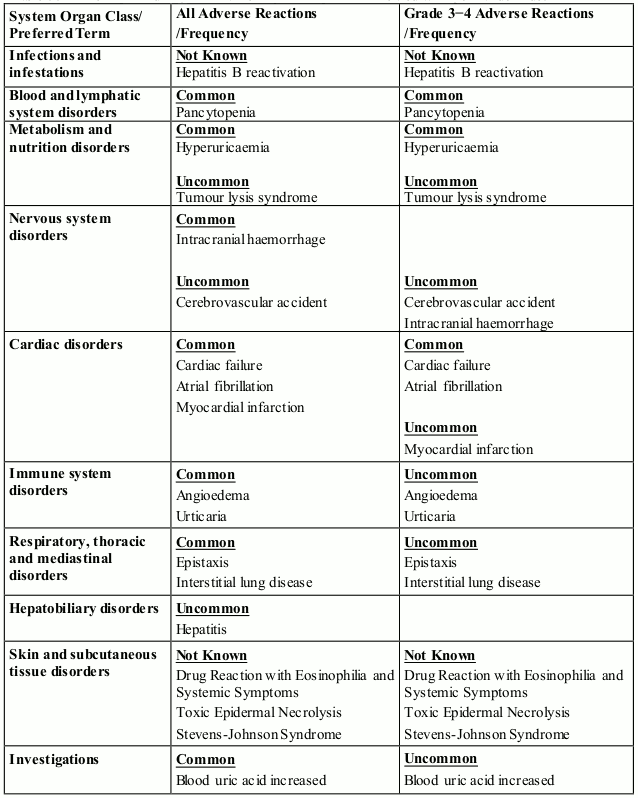
Pomalidomide in combination with dexamethasone
In randomised study CC-4047-MM-003, 302 patients with relapsed and refractory multiple myeloma were exposed to 4 mg pomalidomide administered once daily for 21 days of each 28–day cycle in combination with a weekly low dose of dexamethasone.
The adverse reactions observed in patients treated with pomalidomide plus dexamethasone are listed below in Table 2 by system organ class (SOC) and frequency for all adverse reactions (ADRs) and for Grade 3 or 4 adverse reactions.
The frequencies of adverse reactions are those reported in the pomalidomide plus dexamethasone arm of study CC-4047-MM-003 (n=302). Within each SOC and frequency grouping, adverse reactions are presented in order of decreasing seriousness. Frequencies are defined in accordance with current guidance, as: very common (≥1/10), common (≥1/100 to <1/10); and uncommon (≥1/1,000 to <1/100).
Table 2. ADRs reported in clinical study MM-003 in patients treated with pomalidomide in combination with dexamethasone:
Tabulated list of post-marketing adverse reactions
In addition to the above adverse reactions identified from the pivotal clinical trials, the following Table 3 is derived from data gathered from post-marketing surveillance.
Table 3. ADRs reported in post-marketing use in patients treated with pomalidomide:
Description of selected adverse reactions
Teratogenicity
Pomalidomide is structurally related to thalidomide. Thalidomide is a known human teratogenic active substance that causes severe life-threatening birth defects. Pomalidomide was found to be teratogenic in both rats and rabbits when administered during the period of major organogenesis. If pomalidomide is taken during pregnancy, a teratogenic effect of pomalidomide in humans is expected.
Neutropenia and thrombocytopenia
In patients receiving combination therapy with pomalidomide in clinical studies, neutropenia occurred in up to 46.8% of patients (41.7% Grade 3 or 4). Neutropenia did not lead to pomalidomide discontinuation in any patient and was infrequently serious.
Febrile neutropenia (FN) was reported in 3.2-6.7% of patients and was serious in 1.8-4.0% of patients.
In patients receiving combination therapy with pomalidomide in clinical studies, thrombocytopenia occurred in 27.0-36.7% of patients. Thrombocytopenia was Grade 3 or 4 in 20.7-27.3% of patients, led to pomalidomide discontinuation in 0.7% of patients and was serious in 0.4-1.7% of patients.
Neutropenia and thrombocytopenia tended to occur more frequently within the first 2 cycles of treatment with pomalidomide.
Infection
Infection was the most common non haematological toxicity.
In patients receiving combination therapy with pomalidomide in clinical studies, infection occurred in 55.0-80.2% of patients (24.0-30.9% Grade 3 or 4). Upper respiratory tract infection and pneumonia were the most frequently occurring infections. Fatal infections (Grade 5) occurred in 2.7-4.0% of patients. Infections led to pomalidomide discontinuation in 2.0-2.9% of patients.
Thromboembolic events
Prophylaxis with acetylsalicylic acid (and other anticoagulants in high risk patients) was mandatory for all patients in clinical studies. Anticoagulation therapy (unless contraindicated) is recommended.
In patients receiving combination therapy with pomalidomide in clinical studies, venous thromboembolic events (VTE) occurred in 3.3-11.5% of patients (1.3-5.4% Grade 3 or 4). VTE was reported as serious in 1.7-4.3% of patients, no fatal reactions were reported, and VTE was associated with pomalidomide discontinuation in up to 1.8% of patients.
Peripheral neuropathy
Pomalidomide in combination with bortezomib and dexamethasone
Patients with ongoing peripheral neuropathy ≥ Grade 2 with pain within 14 days prior to randomisation were excluded from clinical trials. Peripheral neuropathy occurred in 55.4 % of patients (10.8% Grade 3; 0.7% Grade 4). Exposure-adjusted rates were comparable across treatment arms. Approximately 30% of the patients experiencing peripheral neuropathy had a history of neuropathy at baseline. Peripheral neuropathy led to discontinuation of bortezomib in approximately 12.9% of patients, pomalidomide in 1.8% and dexamethasone in 2.2-8.9% of patients, respectively. Refer also to the bortezomib SmPC.
Pomalidomide in combination with dexamethasone
Patients with ongoing peripheral neuropathy ≥ Grade 2 were excluded from clinical studies. Peripheral neuropathy occurred in 12.3% of patients (1.0% Grade 3 or 4). No peripheral neuropathy reactions were reported as serious, and peripheral neuropathy led to dose discontinuation in 0.3% of patients.
Haemorrhage
Haemorrhagic disorders have been reported with pomalidomide, especially in patients with risk factors such as concomitant medicinal products that increase susceptibility to bleeding. Haemorrhagic events have included epistaxis, intracranial haemorrhage and gastrointestinal haemorrhage.
Allergic reactions and severe skin reactions
Angioedema and severe cutaneous reactions including SJS, TEN and DRESS has been reported with the use of pomalidomide. Patients with a history of severe rash associated with lenalidomide or thalidomide should not receive pomalidomide.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.