IMITREX Solution for injection Ref.[10575] Active ingredients: Sumatriptan
Source: FDA, National Drug Code (US) Revision Year: 2020
12.1. Mechanism of Action
Sumatriptan binds with high affinity to human cloned 5-HT1B/1D receptors. Sumatriptan presumably exerts its therapeutic effects in the treatment of migraine and cluster headaches through agonist effects at the 5-HT1B/1D receptors on intracranial blood vessels and sensory nerves of the trigeminal system, which result in cranial vessel constriction and inhibition of pro-inflammatory neuropeptide release.
12.2. Pharmacodynamics
Blood Pressure
Significant elevation in blood pressure, including hypertensive crisis, has been reported in patients with and without a history of hypertension [see Warnings and Precautions (5.8)].
Peripheral (Small) Arteries
In healthy volunteers (N=18), a trial evaluating the effects of sumatriptan on peripheral (small vessel) arterial reactivity failed to detect a clinically significant increase in peripheral resistance.
Heart Rate
Transient increases in blood pressure observed in some patients in clinical trials carried out during sumatriptan’s development as a treatment for migraine were not accompanied by any clinically significant changes in heart rate.
12.3. Pharmacokinetics
Absorption
The bioavailability of sumatriptan via subcutaneous site injection to 18 healthy male subjects was 97% ± 16% of that obtained following intravenous injection.
After a single 6-mg subcutaneous manual injection into the deltoid area of the arm in 18 healthy males (age: 24 ± 6 years, weight: 70 kg), the maximum serum concentration (Cmax) of sumatriptan was (mean ± standard deviation) 74 ± 15 ng/mL and the time to peak concentration (Tmax) was 12 minutes after injection (range: 5 to 20 minutes). In this trial, the same dose injected subcutaneously in the thigh gave a Cmax of 61 ± 15 ng/mL by manual injection versus 52 ± 15 ng/mL by autoinjector techniques. The Tmax or amount absorbed was not significantly altered by either the site or technique of injection.
Distribution
Protein binding, determined by equilibrium dialysis over the concentration range of 10 to 1,000 ng/mL is low, approximately 14% to 21%. The effect of sumatriptan on the protein binding of other drugs has not been evaluated.
Following a 6-mg subcutaneous injection into the deltoid area of the arm in 9 males (mean age: 33 years, mean weight: 77 kg) the volume of distribution central compartment of sumatriptan was 50 ± 8 liters and the distribution half‑life was 15 ± 2 minutes.
Metabolism
In vitro studies with human microsomes suggest that sumatriptan is metabolized by MAO, predominantly the A isoenzyme. Most of a radiolabeled dose of sumatriptan excreted in the urine is the major metabolite indole acetic acid (IAA) or the IAA glucuronide, both of which are inactive.
Elimination
After a single 6-mg subcutaneous dose, 22% ± 4% was excreted in the urine as unchanged sumatriptan and 38% ± 7% as the IAA metabolite.
Following a 6-mg subcutaneous injection into the deltoid area of the arm, the systemic clearance of sumatriptan was 1,194 ± 149 mL/min and the terminal half-life was 115 ± 19 minutes.
Specific Populations
Age
The pharmacokinetics of sumatriptan in the elderly (mean age: 72 years, 2 males and 4 females) and in subjects with migraine (mean age: 38 years, 25 males and 155 females) were similar to that in healthy male subjects (mean age: 30 years).
Patients with Hepatic Impairment
The effect of mild to moderate hepatic disease on the pharmacokinetics of subcutaneously administered sumatriptan has been evaluated. There were no significant differences in the pharmacokinetics of subcutaneously administered sumatriptan in moderately hepatically impaired subjects compared with healthy controls. The pharmacokinetics of subcutaneously administered sumatriptan in patients with severe hepatic impairment has not been studied. The use of IMITREX injection in this population is contraindicated [see Contraindications (4)].
Racial Groups
The systemic clearance and Cmax of subcutaneous sumatriptan were similar in black (n=34) and Caucasian (n=38) healthy male subjects.
Drug Interaction Studies
Monoamine Oxidase-A Inhibitors
In a trial of 14 healthy females, pretreatment with an MAO-A inhibitor decreased the clearance of subcutaneous sumatriptan, resulting in a 2-fold increase in the area under the sumatriptan plasma concentration-time curve (AUC), corresponding to a 40% increase in elimination half-life.
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
In carcinogenicity studies in mouse and rat, sumatriptan was administered orally for 78 weeks and 104 weeks, respectively, at doses up to 160 mg/kg/day (the high dose in rat was reduced from 360 mg/kg/day during Week 21). The highest dose to mice and rats was approximately 130 and 260 times the single MRHD of 6 mg administered subcutaneously on a mg/m 2 basis. There was no evidence in either species of an increase in tumors related to sumatriptan administration.
Mutagenesis
Sumatriptan was negative in in vitro (bacterial reverse mutation [Ames], gene cell mutation in Chinese hamster V79/HGPRT, chromosomal aberration in human lymphocytes) and in vivo (rat micronucleus) assays.
Impairment of Fertility
When sumatriptan (5, 50, 500 mg/kg/day) was administered orally to male and female rats prior to and throughout the mating period, there was a treatment-related decrease in fertility secondary to a decrease in mating in animals treated with doses greater than 5 mg/kg/day. It is not clear whether this finding was due to an effect on males or females or both.
When sumatriptan was administered by subcutaneous injection to male and female rats prior to and throughout the mating period, there was no evidence of impaired fertility at doses up to 60 mg/kg/day.
13.2. Animal Toxicology and/or Pharmacology
Corneal Opacities
Dogs receiving oral sumatriptan developed corneal opacities and defects in the corneal epithelium. Corneal opacities were seen at the lowest dose tested, 2 mg/kg/day, and were present after 1 month of treatment. Defects in the corneal epithelium were noted in a 60-week study. Earlier examinations for these toxicities were not conducted and no-effect doses were not established; however, the relative plasma exposure at the lowest dose tested was approximately 3 times the human exposure after a 6-mg subcutaneous dose.
14. Clinical Studies
14.1 Migraine
In controlled clinical trials enrolling more than 1,000 patients during migraine attacks who were experiencing moderate or severe pain and 1 or more of the symptoms enumerated in Table 3, onset of relief began as early as 10 minutes following a 6-mg IMITREX injection. Lower doses of IMITREX injection may also prove effective, although the proportion of patients obtaining adequate relief was decreased and the latency to that relief is greater with lower doses.
In Study 1, 6 different doses of IMITREX injection (n=30 each group) were compared with placebo (n=62) in a single-attack, parallel-group design; the dose-response relationship was found to be as shown in Table 2.
Table 2. Proportion of Patients with Migraine Relief and Incidence of Adverse Reactions by Time and by Dose of IMITREX in Study 1:
| Dose of IMITREX Injection | Percent Patients with Reliefa | Adverse Reactions Incidence (%) | |||
|---|---|---|---|---|---|
| at 10 Minutes | at 30 Minutes | at 1 Hour | at 2 Hours | ||
| Placebo | 5 | 15 | 24 | 21 | 55 |
| 1 mg | 10 | 40 | 43 | 40 | 63 |
| 2 mg | 7 | 23 | 57 | 43 | 63 |
| 3 mg | 17 | 47 | 57 | 60 | 77 |
| 4 mg | 13 | 37 | 50 | 57 | 80 |
| 6 mg | 10 | 63 | 73 | 70 | 83 |
| 8 mg | 23 | 57 | 80 | 83 | 93 |
a Relief is defined as the reduction of moderate or severe pain to no or mild pain after dosing without use of rescue medication.
In 2 randomized, placebo-controlled clinical trials of IMITREX injection 6 mg in 1,104 patients with moderate or severe migraine pain (Studies 2 and 3), the onset of relief was less than 10 minutes. Headache relief, as defined by a reduction in pain from severe or moderately severe to mild or no headache, was achieved in 70% of the patients within 1 hour of a single 6-mg subcutaneous dose of IMITREX injection. Approximately 82% and 65% of patients treated with IMITREX 6 mg had headache relief and were pain free within 2 hours, respectively.
Table 3 shows the 1- and 2-hour efficacy results for IMITREX injection 6 mg in Studies 2 and 3.
Table 3. Proportion of Patients with Pain Relief and Relief of Migraine Symptoms after 1 and 2 Hours of Treatment in Studies 2 and 3:
| 1-Hour Data | Study 2 | Study 3 | ||
|---|---|---|---|---|
| Placebo (n=190) | IMITREX 6 mg (n=384) | Placebo (n=180) | IMITREX 6 mg (n=350) | |
| Patients with pain relief (Grade 0/1) | 18% | 70%a | 26% | 70%a |
| Patients with no pain | 5% | 48%a | 13% | 49%a |
| Patients without nausea | 48% | 73%a | 50% | 73%a |
| Patients without photophobia | 23% | 56%a | 25% | 58%a |
| Patients with little or no clinical disabilityb | 34% | 76%a | 34% | 76%a |
| 2-Hour Data | Study 2 | Study 3 | ||
| Placeboc | IMITREX 6 mgd | Placeboc | IMITREX 6 mgd | |
| Patients with pain relief (Grade 0/1) | 31% | 81%a | 39% | 82%a |
| Patients with no pain | 11% | 63%a | 19% | 65%a |
| Patients without nausea | 56% | 82%a | 63% | 81%a |
| Patients without photophobia | 31% | 72%a | 35% | 71%a |
| Patients with little or no clinical disabilityb | 42% | 85%a | 49% | 84%a |
a P<0.05 versus placebo.
b A successful outcome in terms of clinical disability was defined prospectively as ability to work mildly impaired or ability to work and function normally.
c Includes patients that may have received an additional placebo injection 1 hour after the initial injection.
d Includes patients that may have received an additional 6 mg of IMITREX injection 1 hour after the initial injection.
IMITREX injection also relieved photophobia, phonophobia (sound sensitivity), nausea, and vomiting associated with migraine attacks. Similar efficacy was seen when patients self-administered IMITREX injection using the IMITREX STATdose Pen.
The efficacy of IMITREX injection was unaffected by whether or not the migraine was associated with aura, duration of attack, gender or age of the patient, or concomitant use of common migraine prophylactic drugs (e.g., beta-blockers).
14.2 Cluster Headache
The efficacy of IMITREX injection in the acute treatment of cluster headache was demonstrated in 2 randomized, double-blind, placebo-controlled, 2-period crossover trials (Studies 4 and 5). Patients aged 21 to 65 years were enrolled and were instructed to treat a moderate to very severe headache within 10 minutes of onset. Headache relief was defined as a reduction in headache severity to mild or no pain. In both trials, the proportion of individuals gaining relief at 10 or 15 minutes was significantly greater among patients receiving 6 mg of IMITREX injection compared with those who received placebo (see Table 4).
Table 4. Proportion of Patients with Cluster Headache Relief by Time in Studies 4 and 5:
| Study 4 | Study 5 | |||
|---|---|---|---|---|
| Placebo (n=39) | IMITREX 6 mg (n=39) | Placebo (n=88) | IMITREX 6 mg (n=92) | |
| Patients with pain relief (no/mild) | ||||
| 5 Minutes post-injection | 8% | 21% | 7% | 23% a |
| 10 Minutes post-injection | 10% | 49%a | 25% | 49%a |
| 15 Minutes post-injection | 26% | 74%a | 35% | 75%a |
a P<0.05.
n=Number of headaches treated.
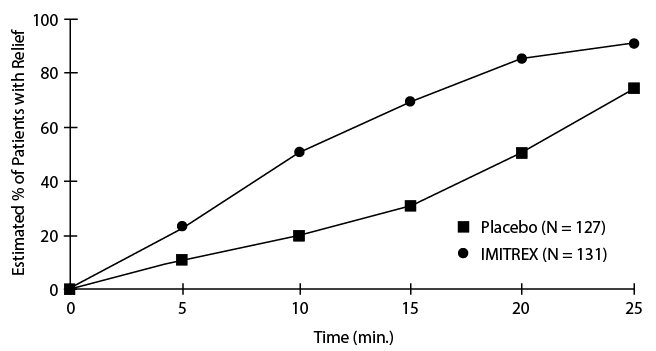
An estimate of the cumulative probability of a patient with a cluster headache obtaining relief after being treated with either IMITREX injection or placebo is presented in Figure 1.
Figure 1. Time to Relief of Cluster Headache from Time of Injectiona
a The figure uses Kaplan-Meier (product limit) Survivorship Plot. Patients taking rescue medication were censored at 15 minutes.
The plot was constructed with data from patients who either experienced relief or did not require (request) rescue medication within a period of 2 hours following treatment. As a consequence, the data in the plot are derived from only a subset of the 258 headaches treated (rescue medication was required in 52 of the 127 placebo-treated headaches and 18 of the 131 headaches treated with IMITREX injection).
Other data suggest that treatment with IMITREX injection is not associated with an increase in early recurrence of headache and has little effect on the incidence of later-occurring headaches (i.e., those occurring after 2, but before 18 or 24 hours).
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.