CLARITHROMYCIN Film-coated tablets Ref.[6721] Active ingredients: Clarithromycin
Source: Medicines & Healthcare Products Regulatory Agency (GB) Revision Year: 2018 Publisher: Milpharm Limited, Ares Block, Odyssey Business Park, West End Road, Ruislip HA4 6QD, United Kingdom
Pharmacodynamic properties
Pharmacotherapeutic group: Macrolides
ATC code: J01FA09
Mode of action
Clarithromycin is a semi-synthetic derivative of erythromycin A. It exerts its antibacterial action by binding to the 50s ribosomal sub-unit of susceptible bacteria and suppresses protein synthesis. It is highly potent against a wide variety of aerobic and anaerobic gram-positive and gram-negative organisms. The minimum inhibitory concentrations (MICs) of clarithromycin are generally two-fold lower than the MICs of erythromycin.
The 14-hydroxy metabolite of clarithromycin also has antimicrobial activity. The MICs of this metabolite are equal or twofold higher than the MICs of the parent compound, except for H. influenzae where the 14-hydroxy metabolite is two-fold more active than the parent compound.
PK/PD relationship
Clarithromycin is extensively distributed into body tissues and fluids. Due to the high tissue penetration, intracellular concentrations higher than serum concentrations. The main pharmacodynamic parameters to predict macrolidenactiviteit are unconvincing established. The time above the MIC (T/MIC) is the best determinant for the efficacy of clarithromycin. Because the concentrations of clarithromycin in the lung tissues and epithelial tissue fluid reaches the plasma concentrations exceed, the use of plasma concentrations based parameters are insufficient to accurately predict response for respiratory infections.
Mechanisms of resistance
Resistance mechanisms against macrolide antibiotics include alteration of the target site of the antibiotic or are based on modification and/or the active efflux of the antibiotic. Resistance development can be mediated via chromosomes or plasmids, be induced or exist constitutively.
Macrolideresistant bacteria generate enzymes which lead to methylation of residual adenine at ribosomal RNA and consequently to inhibition of the antibiotic binding to the ribosome. Macrolide-resistant organisms are generally cross-resistant to lincosamides and streptogramine B based on methylation of the ribosomal binding site. Clarithromycin ranks among the strong inducers of this enzyme as well. Furthermore, macrolides have a bacteriostatic action by inhibiting the peptidyl transferase of ribosomes. A complete cross-resistance exists among clarithromycin, erythromycin and azithromycin. Methicillin-resistant staphylococci and penicillin-resistant Streptococcus pneumoniae are resistant to macrolides such as clarithromycin.
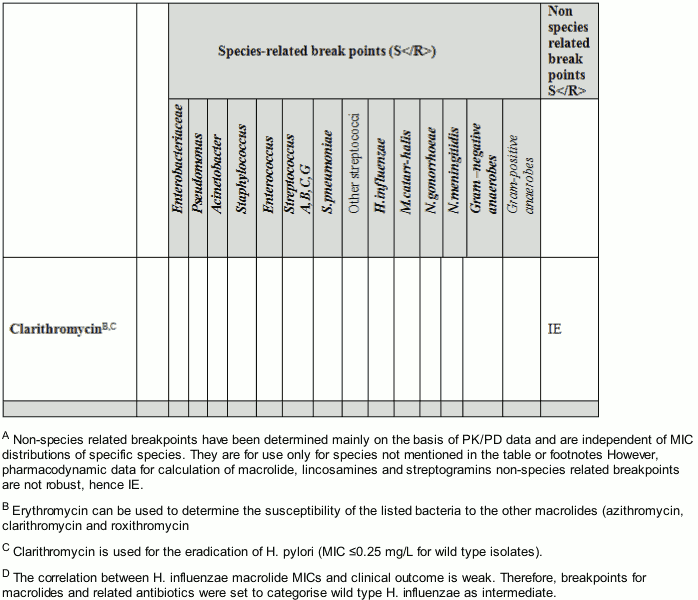
Breakpoints
The following breakpoints for clarithromycin, separating susceptible organisms from resistant organisms, have been established by the European Committee for Antimicrobial Susceptibility Testing (EUCAST) 2010-04-27 (v 1.1).
Clarithromycin is used for the eradication of H. pylori; minimum inhibitory concentration (MIC) ≤0.25 μg/ml which has been established as the susceptible breakpoint by the Clinical and Laboratory Standards Institute (CLSI).
Susceptibility
The prevalence of acquired resistance may vary geographically and with time for selected species and local information on resistance is desirable, particularly when treating severe infections. As necessary, expert advice should be sought when the local prevalance of resistance is such that the utility of the agent in atleast some types of infections is questionable.
Commonly susceptible species
Aerobic, Gram-positive microorganisms:
Streptococcus group F
Corynebacterium diptheriae
Aerobic, Gram-negative microorganisms:
Bordetella pertusis
Moraxella catarrhalis
Pasteurella multocida
Legionella spp.
Anaerobic microorganisms:
Clostridium spp., other than C. difficile
Other microorganisms:
Mycoplasma pneumoniae
Chlamydia trachomatis
Clamydophila pneumoniae
Clamydophilapsitacci
Mycobacterium spp.
Species for which acquired resistance may be a problem#
Aerobic, Gram-positive microorganisms:
Streptococcus group A*, C, G
Streptococcus group B
Streptococcus viridans
Enterococcus spp+
Staphylococcus aureus, methicillin-susceptible and methicillin-resistant+
Streptococcus pneumoniae*+
Staphylococcus epidermidis+
Aerobic, Gram-negative microorganisms:
Haemophilus influenzae$
Helicobacter pylori
Anaerobic microorganisms:
Bacteroides spp.
Peptococcus/Peptostreptococcus spp.
Inherently resistant microorganisms
Aerobic, Gram-negative microorganisms:
Pseudomonas aeruginosa
Acinetobacter
Enterobacteriacea
Anaerobic microorganisms:
Fusobacterium spp.
Other microorganisms:
Mycobacterium tuberculosis
# ≥10% resistance in at least one country of the European Union
* Species against efficacy has been demonstrated in clinical investigations (if susceptible).
+ Indicates species for which a high rate of resistance (i.e. greater than 50%) have been observed in one or more area/country/region(s) of the EU.
§ Breakpoints for macrolides and related antibiotics were set to categorise wild type H. influenzae as intermediate.
Other information
Susceptibility and resistance of Streptococcus pneumoniae and Streptococcus spp. to clarithromycin can be predicted by testing erythromycin.
Most available clinical experience from controlled randomised clinical trials indicate that clarithromycin 500 mg twice daily in combination with another antibiotic e.g. amoxicillin or metronidazole and e.g. omeprazole (given at approved levels) for 7 days achieve >80% H. pylori eradication rate in patients with gastro-duodenal ulcers. As expected, significantly lower eradication rates were observed in patients with baseline metronidazole-resistant H. pylori isolates. Hence, local information on the prevalence of resistance and local therapeutic guidelines should be taken into account in the choice of an appropriate combination regimen for H. pylori eradication therapy. Furthermore, in patients with persistent infection, potential development of secondary resistance (in patients with primary susceptible strains) to an antimicrobial agent should be taken into the considerations for a new retreatment regimen.
Pharmacokinetic properties
Absorption
Clarithromycin is rapidly and well absorbed from the gastrointestinal tract – primarily in the jejunum – but undergoes extensive first-pass metabolism after oral administration. The absolute bioavailability of a 250 mg clarithromycin tablet is approximately 50%. Food slightly delays the absorption but does not affect the extent of bioavailability. Therefore, clarithromycin tablets may be given without regard to food. Due to its chemical structure (6-O-Methylerythromycin) clarithromycin is quite resistant to degradation by stomach acid. Peak plasma levels of 1–2 μg/ml clarithromycin were observed in adults after oral administration of 250 mg twice daily. After administration of 500 mg clarithromycin twice daily the peak plasma level was 2.8 μg/ml. After administration of 250 mg clarithromycin twice daily the microbiologically active 14-hydroxy metabolite attains peak plasma concentrations of 0.6 μg/ml. Steady state is attained within 2 days of dosing.
Distribution
Clarithromycin penetrates well into different compartments with an estimated volume of distribution of 200-400 l. Clarithromycin provides concentrations in some tissues that are several times higher than the circulating drug levels. Increased levels have been found in both tonsils and lung tissue. Clarithromycin also penetrates the gastric mucus.
Clarithromycin is approximately 70% bound to plasma proteins at therapeutic levels.
Biotransformation and elimination
Clarithromycin is rapidly and extensively metabolised in the liver. Metabolism is in the liver involving the P450 cytochrome system. Three metabolites are described: N-demethyl clarithromycin, decladinosyl clarithromycin and 14-hydroxy clarithromycin. The pharmacokinetics of clarithromycin is non-linear due to saturation of hepatic metabolism at high doses. Elimination half-life increased from 2-4 hours following administration of 250 mg clarithromycin twice daily to 5 hours following administration of 500 mg clarithromycin twice daily. The half-life of the active 14-hydroxy metabolite ranges between 5 to 6 hours following administration of 250 mg clarithromycin twice daily.
Approximately 20-40% of clarithromycin is excreted as the unchanged active substance in the urine. This proportion is increased when the dose is increased. An additional 10% to 15% is excreted in the urine as 14-hydroxy metabolite. The rest is excreted in the faeces.Renal insufficiency increases clarithromycin levels in plasma, if the dose is not decreased. Total plasma clearance has been estimated to approximately 700 mL/min (11,7 mL/s), with a renal clearance of approximately 170 mL/min (2,8 mL/s).
Special populations
Renal impairment
Reduced renal insufficiency function results in increased plasma levels of clarithromycin and the active metabolite levels in plasma.
Preclinical safety data
In 4-week-studies in animals, toxicity of clarithromycin was found to be related to the dose and to the duration of the treatment. In all species, the first signs of toxicity were observed in the liver, in which lesions were seen within 14 days in dogs and monkeys. The systemic levels of exposure, related to this toxicity, are not known in detail, but toxic doses were clearly higher than the therapeutic doses recommended for humans. Other tissues affected included the stomach, thymus and other lymphoid tissues as well as the kidneys. At near therapeutic doses conjunctival injection and lacrimation occurred only in dogs. At a dose of 400 mg/kg/day some dogs and monkeys developed corneal opacities and/or oedema.
No mutagenic effects were found in in vitro- and in vivo-studies with clarithromycin
Studies on reproduction toxicity showed that administration of clarithromycin at doses 2x the clinical dose in rabbit (i.v.) and x10 the clinical dose in monkey (p.o.) resulted in an increased incidence of spontaneous abortions. These doses were related to maternal toxicity. No embryotoxicity or teratogenicity was noted in rat studies. Cardiovascular malformations were observed in rats treated with doses of 150 mg/kg/d. In mouse at doses x70 the clinical dose cleft palate occurred at varying incidence (3-30%).
Clarithromycin has been found in the milk of lactating animals.
In 3-day old mice and rats, the LD50 values were approximately half those in adult animals. Juvenile animals presented similar toxicity profiles to mature animals although enhanced nephrotoxicity in neonatal rats has been reported in some studies. Slight reductions in erythrocytes, platelets and leukocytes have also been found in juvenile animals.
Clarithromycin has not been tested for carcinogenicity.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.