COMBIVENT RESPIMAT Inhalation spray Ref.[10548] Active ingredients: Ipratropium Salbutamol
Source: FDA, National Drug Code (US) Revision Year: 2020
12.1. Mechanism of Action
COMBIVENT RESPIMAT is a combination of the anticholinergic ipratropium bromide and the beta2-adrenergic agonist albuterol sulfate. The mechanisms of action described below for the individual components apply to COMBIVENT RESPIMAT. The two classes of medications (an anticholinergic and a beta2-adrenergic agonist) are both bronchodilators. Simultaneous administration of both an anticholinergic (ipratropium bromide) and a beta2-sympathomimetic (albuterol sulfate) is designed to produce a greater bronchodilator effect than when either drug is utilized alone at its recommended dosage. The efficacy of COMBIVENT RESPIMAT is likely to be due to a local effect on the muscarinic and beta2-adrenergic receptors in the lung.
Ipratropium bromide
Ipratropium bromide is an anticholinergic (parasympatholytic) agent which, based on animal studies, appears to inhibit vagally mediated reflexes by antagonizing the action of acetylcholine, the transmitter agent released at the neuromuscular junctions in the lung. Anticholinergics prevent the increases in intracellular concentration of Ca++ which is caused by interaction of acetylcholine with the muscarinic receptors on bronchial smooth muscle.
Albuterol sulfate
In vitro studies and in vivo pharmacology studies have demonstrated that albuterol has a preferential effect on beta2-adrenergic receptors compared with isoproterenol. While it is recognized that beta2-adrenergic receptors are the predominant receptors on bronchial smooth muscle, recent data indicate that there is a population of beta2-receptors in the human heart which comprise between 10% and 50% of cardiac beta-adrenergic receptors. The precise function of these receptors, however, is not yet established [see Warnings and Precautions (5.2)].
Activation of beta2-adrenergic receptors on airway smooth muscle leads to the activation of adenylyl cyclase and to an increase in the intracellular concentration of cyclic-3',5'-adenosine monophosphate (cyclic AMP). This increase of cyclic AMP leads to the activation of protein kinase, which inhibits the phosphorylation of myosin and lowers intracellular ionic calcium concentrations, resulting in relaxation. Albuterol relaxes the smooth muscles of all airways, from the trachea to the terminal bronchioles. Albuterol acts as a functional antagonist to relax the airway irrespective of the spasmogen involved, thus protecting against all bronchoconstrictor challenges. Increased cyclic AMP concentrations are also associated with the inhibition of release of mediators from mast cells in the airway.
Albuterol has been shown in most clinical trials to have more bronchial smooth muscle relaxation effect than isoproterenol at comparable doses while producing fewer cardiovascular effects. However, all beta‑adrenergic agonist drugs, including albuterol sulfate, can produce a significant cardiovascular effect in some patients [see Warnings and Precautions (5.2)].
12.2. Pharmacodynamics
Ipratropium bromide
Cardiovascular effects
At recommended doses, ipratropium bromide does not produce clinically significant changes in pulse rate or blood pressure.
Ocular effects
In studies without a positive control, ipratropium bromide did not alter pupil size, accommodation, or visual acuity.
Mucociliary clearance and respiratory secretions
Controlled clinical studies have demonstrated that ipratropium bromide does not alter either mucociliary clearance or the volume or viscosity of respiratory secretions.
Albuterol sulfate
Cardiovascular effects
Controlled clinical trials and other clinical experience have shown that inhaled albuterol, like other beta-adrenergic agonist drugs, can produce a significant cardiovascular effect in some patients, as measured by pulse rate, blood pressure, symptoms, and/or electrocardiographic changes.
12.3. Pharmacokinetics
Ipratropium bromide
Ipratropium bromide is a quaternary amine and hence, it is not readily absorbed into the systemic circulation either from the surface of the lung or from the gastrointestinal tract as confirmed by blood level and renal excretion studies.
The half-life of elimination is about 2 hours after inhalation or intravenous administration. Ipratropium bromide is minimally bound (0% to 9% in vitro) to plasma albumin and α1-acid glycoprotein. It is partially metabolized to inactive ester hydrolysis products. Following intravenous administration, approximately one-half of the dose is excreted unchanged in the urine.
Albuterol sulfate
Albuterol is longer acting than isoproterenol in most patients because it is not a substrate for the cellular uptake processes for catecholamines, nor for metabolism by catechol-O-methyl transferase. Instead, the drug is conjugatively metabolized to albuterol 4'-O-sulfate.
Intravenous pharmacokinetics of albuterol was studied in a comparable group of 16 healthy male volunteers; the mean terminal half-life following a 30-minute infusion of 1.5 mg was 3.9 hours, with a mean clearance of 439 mL/min/1.73 m².
COMBIVENT RESPIMAT Inhalation Spray
In a 12-week randomized, multicenter, double-blind, double-dummy parallel group trial, 108 US patients with COPD receiving either COMBIVENT RESPIMAT (20/100 mcg) or CFC-propelled COMBIVENT Inhalation Aerosol (36/206 mcg) four times daily participated in pharmacokinetic evaluations. Plasma ipratropium concentrations were low with an average peak plasma concentration of 33.5 pg/mL from COMBIVENT RESPIMAT. The majority of the study participants exhibited levels below the lower limit of quantitation (<10 pg/mL) by 4 to 6 hours following dosing. The steady state systemic exposure obtained for ipratropium bromide following COMBIVENT RESPIMAT was comparable to that of CFC-propelled COMBIVENT Inhalation Aerosol. Ipratropium plasma AUC and total amount of drug excreted unchanged in urine (Ae) ratios for COMBIVENT RESPIMAT/CFC-propelled COMBIVENT Inhalation Aerosol were 1.04 and 1.18, respectively. For albuterol the steady state systemic exposure was less from COMBIVENT RESPIMAT compared to that of CFC-propelled COMBIVENT Inhalation Aerosol. Albuterol plasma AUC and urine Ae ratios for COMBIVENT RESPIMAT/CFC-propelled COMBIVENT Inhalation Aerosol were 0.74 and 0.86, respectively.
Pharmacokinetic drug-drug interaction between ipratropium bromide and albuterol sulfate was evaluated in a crossover study in 12 healthy male volunteers who received CFC-propelled COMBIVENT Inhalation Aerosol and the two active components separately as individual treatments. Results from this study indicated that the coadministration of these two components from a single canister did not significantly alter the systemic absorption of either component, indicating lack of any pharmacokinetic interaction between these two drugs.
Specific Populations
Age
Consistent with CFC-propelled COMBIVENT Inhalation Aerosol (36/206 mcg), patients receiving COMBIVENT RESPIMAT (20/100 mcg) aged 65 years and over had higher steady state systemic exposures than patients aged under 65 years for both ipratropium (AUC = 166 vs. 105 pg•hr/mL, Cmax = 38.5 vs. 30.1 pg/mL) and albuterol (AUC = 5.44 vs. 3.27 ng•hr/mL, Cmax = 1.19 vs. 0.74 ng/mL).
Gender
The AUC and Cmax values for ipratropium were 131 pg.hr/mL and 35.4 pg/mL in males and 123 pg.hr/mL and 31.7 pg/mL in females, respectively. The AUC- and Cmax-values for albuterol were 4.0 ng•hr/mL and 0.89 ng/mL in males and 4.2 ng•hr/mL and 0.93 ng/mL in females, respectively.
Hepatic and Renal Impairment
The pharmacokinetics of COMBIVENT RESPIMAT or ipratropium bromide has not been studied in patients with hepatic or renal insufficiency.
Drug-Drug Interactions
No specific pharmacokinetic studies were conducted to evaluate potential drug-drug interactions with other medications.
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Ipratropium bromide
Two-year oral carcinogenicity studies in rats and mice have revealed no carcinogenic activity at doses up to 6 mg/kg/day (approximately 400 and 200 times the maximum recommended human daily inhalation dose of ipratropium bromide (MRHDID) in adults on a mg/m² basis, respectively).
Results of various mutagenicity/clastogenicity studies (Ames test, mouse dominant lethal test, mouse micronucleus test, and chromosome aberration of bone marrow in Chinese hamsters) were negative.
Fertility of male or female rats at oral doses up to 50 mg/kg/day (approximately 3400 times the MRHDID in adults on a mg/m² basis) was unaffected by ipratropium bromide administration. At an oral dose of 500 mg/kg/day (approximately 34,000 times the MRHDID in adults on a mg/m² basis), ipratropium bromide produced a decrease in the conception rate.
Albuterol
Like other agents in its class, albuterol caused a significant dose-related increase in the incidence of benign leiomyomas of the mesovarium in a 2-year study in the rat at dietary doses of 2, 10, and 50 mg/kg/day (approximately 20, 110, and 560 times the MRHDID on a mg/m² basis). In another study this effect was blocked by the coadministration of propranolol. The relevance of these findings to humans is not known. An 18-month study in mice at dietary doses up to 500 mg/kg/day (approximately 2800 times the MRHDID on a mg/m² basis) and a 99-week study in hamsters at oral doses up to 50 mg/kg/day (approximately 470 times the MRHDID on a mg/m² basis) revealed no evidence of tumorigenicity. Studies with albuterol revealed no evidence of mutagenesis.
Reproduction studies in rats with albuterol sulfate revealed no evidence of impaired fertility.
13.2. Animal Toxicology and/or Pharmacology
Preclinical
Intravenous studies in rats with albuterol sulfate have demonstrated that albuterol crosses the blood-brain barrier and reaches brain concentrations amounting to approximately 5% of the plasma concentrations. In structures outside the blood-brain barrier (pineal and pituitary glands), albuterol concentrations were found to be 100 times those in the whole brain.
Studies in laboratory animals (minipigs, rodents, and dogs) have demonstrated the occurrence of cardiac arrhythmias and sudden death (with histologic evidence of myocardial necrosis) when beta-agonists and methylxanthines were administered concurrently. The clinical significance of these findings is unknown.
14. Clinical Studies
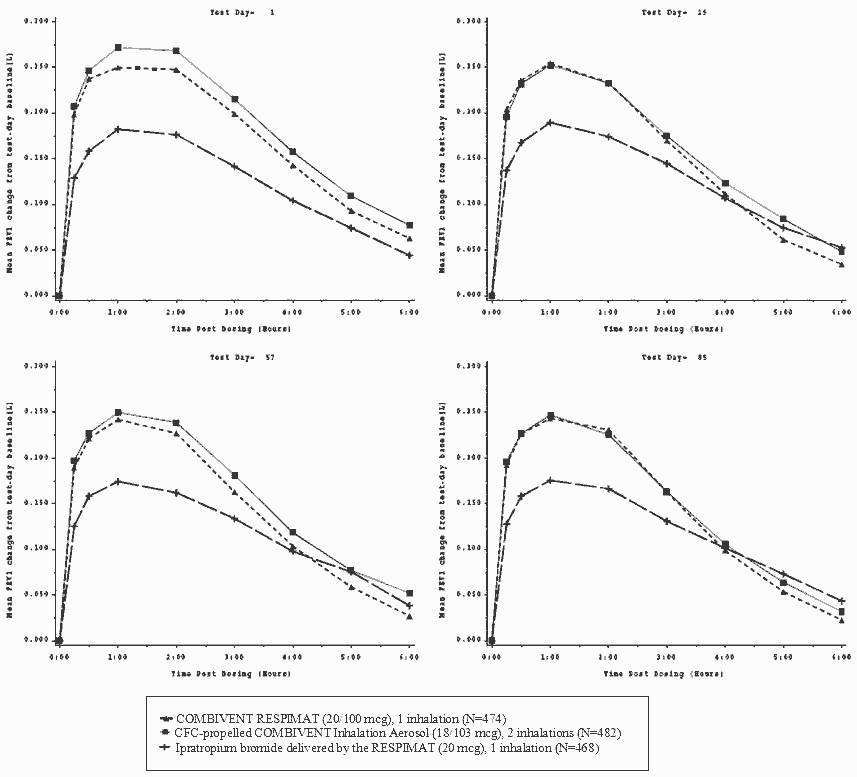
The efficacy of COMBIVENT RESPIMAT (20/100 mcg) was evaluated in COPD patients in one randomized, double-blind, double-dummy parallel group trial. This was a 12-week trial in a total of 1460 adult patients (955 males and 505 females) conducted to demonstrate the efficacy and safety of COMBIVENT RESPIMAT (20/100 mcg) in COPD. All patients were required to have a clinical diagnosis of COPD, be at least 40 years of age or older, to have an FEV1 of less than or equal to 65% predicted and an FEV1/FVC ratio of less than or equal to 0.7 at screening, and a smoking history of greater than 10 pack-years prior to entering the trial. Patients with narrow-angle glaucoma, symptomatic prostatic hypertrophy, or bladder neck obstruction were excluded from the trial. The majority of the patients (89%) were Caucasian, had a mean age of 64 years, a mean percent predicted pre-bronchodilator FEV1 of 41% and FEV1/FVC ratio of 0.45. The patients were randomized to one of the following active treatments COMBIVENT RESPIMAT (20/100 mcg) (n=486), CFC-propelled COMBIVENT Inhalation Aerosol (36/206 mcg) (n=491), and ipratropium bromide delivered by the RESPIMAT (20 mcg) (n=483) administered four times a day. Data from 1424 patients were used in the efficacy analyses.
There were three primary efficacy variables: (i) Mean FEV1 over 0 to 6 hours post-dose defined as the AUC of the change from test-day baseline in FEV1 over 0 to 6 hours post-dose divided by 6 hours (FEV1 AUC0-6h); (ii) Mean FEV1 over 0 to 4 hours post-dose defined as the AUC of the change from test-day baseline in FEV1 over 0 to 4 hours post-dose divided by 4 hours (FEV1 AUC0-4h), and (iii) Mean FEV1 over 4 to 6 hours post-dose defined as the AUC of the change from test-day baseline in FEV1 over 4 to 6 hours post-dose divided by 2 hours (FEV1 AUC4-6h). Test-day baseline was the FEV1 recorded prior to inhaling the dose of randomized treatment on test day.
The three primary efficacy comparisons were: (i) Non-inferiority of COMBIVENT RESPIMAT (20/100 mcg) to CFC-propelled COMBIVENT Inhalation Aerosol (36/206 mcg) for the FEV1 AUC0-6h on Test Day 85; (ii) Superiority of COMBIVENT RESPIMAT (20/100 mcg) to ipratropium RESPIMAT (20 mcg) for the FEV1 AUC0-4h on Test Day 85, to demonstrate the contribution of albuterol in the combination product, and (iii) Non-inferiority of COMBIVENT RESPIMAT (20/100 mcg) in comparison to ipratropium RESPIMAT (20 mcg) for FEV1 AUC4-6h on Test Day 85, to demonstrate the contribution of ipratropium in the combination product. Non-inferiority was declared if the lower bound of the 95% confidence interval for the point estimate for the difference of COMBIVENT RESPIMAT minus the comparator was more than -50 mL.
COMBIVENT RESPIMAT (20/100 mcg) was shown to be non-inferior to CFC-propelled COMBIVENT Inhalation Aerosol (36/206 mcg) in terms of mean FEV1 AUC0-6h. The LS mean (mL) (95% CI) of the treatment difference was -3 (-22, 15). The FEV1 AUC0-4h for COMBIVENT RESPIMAT (20/100 mcg), was superior to that of ipratropium bromide [LS mean (mL) (95% CI) of the treatment difference was 47 mL (28, 66)] and the mean FEV1 AUC4-6h for COMBIVENT RESPIMAT (20/100 mcg) was non-inferior to that of ipratropium bromide [LS mean (mL) (95% CI) of the treatment difference was -17 (-39, 5)]. The FEV1 results on Test Days 1, 29, 57, and 85 are shown in Figure 1.
In this trial, COMBIVENT RESPIMAT (20/100 mcg) was shown to be clinically comparable (statistically non-inferior) to CFC-propelled COMBIVENT Inhalation Aerosol (36/206 mcg).
Additionally, in this trial, no differences in these efficacy comparisons were identified in males and females or in patients over 65 years of age versus those under 65 years of age. There were too few African-American subjects to adequately assess differences in effects in that population.
The median time to onset of bronchodilation, defined as an FEV1 increase of 15% or greater from test-day baseline, for the COMBIVENT RESPIMAT (20/100 mcg) group occurred at 13 minutes post-dose on Day 1.
Figure 1. Time Profile of FEV1 at Days 1, 29, 57 and 85:
The means are adjusted for treatment baseline and investigator site. A separate ANCOVA was fitted for each time point.
The imputation method for data missing because the patient withdrew from the trial was Last Visit Carried Forward.
The imputation method for data missing at the end of test days depends on why the data were missing.
A second study was conducted in 1118 COPD patients using a higher than approved dose of COMBIVENT RESPIMAT. Patients were randomized to COMBIVENT RESPIMAT (40/200 mcg) (n=345), CFC-propelled COMBIVENT Inhalation Aerosol (36/206 mcg) (n=180), ipratropium delivered by the RESPIMAT (40 mcg) (n=252) or placebo (n= 341). The study was supportive, particularly for safety [see Adverse Reactions (6.1)].
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.