MEKTOVI Film-coated tablet Ref.[8686] Active ingredients: Binimetinib
Source: European Medicines Agency (EU) Revision Year: 2024 Publisher: PIERRE FABRE MEDICAMENT, Les Cauquillous, 81500 Lavaur, France
Pharmacodynamic properties
Pharmacotherapeutic group: Antineoplastic agents, protein kinase inhibitors
ATC code: L01EE03
Mechanism of action
Binimetinib is an ATP-uncompetitive, reversible inhibitor of the kinase activity of mitogen-activated extracellular signal regulated kinase 1 (MEK1) and MEK2. In cell free system, binimetinib inhibits MEK1 and MEK2 with the half maximal inhibitory concentration (IC50)'s in the 12-46 nM. MEK proteins are upstream regulators of the extracellular signal-related kinase (ERK) pathway, which promotes cellular proliferation. In melanoma and other cancers, this pathway is often activated by mutated forms of BRAF which activates MEK. Binimetinib inhibits activation of MEK by BRAF and inhibits MEK kinase activity. Binimetinib inhibits growth of BRAF V600 mutant melanoma cell lines and demonstrates anti-tumour effects in BRAF V600 mutant melanoma animal models.
Combination with encorafenib
Binimetinib and encorafenib (a BRAF inhibitor, see section 5.1 of encorafenib SmPC) both inhibit the MAPK pathway resulting in higher anti-tumour activity, compared to treatment with either drug alone.
Clinical efficacy and safety
BRAF V600 mutant unresectable or metastatic melanoma
The safety and efficacy of binimetinib in combination with encorafenib were evaluated in a 2-part Phase III, randomised (1:1:1) active-controlled, open-label, multicenter study in patients with unresectable or metastatic BRAF V600 E or K mutant melanoma (Study CMEK162B2301), as detected using a BRAF assay. Patients had histologically confirmed cutaneous or unknown primary melanoma but those with uveal or mucosal melanoma were excluded. Patients were permitted to receive prior adjuvant therapy and one prior line of immunotherapy for unresectable locally advanced or metastatic disease. Prior treatment with BRAF/MEK inhibitors was not allowed.
Study CMEK162B2301, Part 1
In part 1, patients in the study were randomised to receive binimetinib 45 mg orally twice daily plus encorafenib 450 mg orally daily (Combo 450, n=192), encorafenib 300 mg orally daily (hereafter referred to as Enco 300, n=194), or vemurafenib 960 mg orally twice daily (hereafter referred to as Vem, n=191). Treatment continued until disease progression or unacceptable toxicity. Randomisation was stratified by American Joint Committee on Cancer (AJCC) Stage (IIIB, IIIC, IVM1a or IVM1b, vs IVM1c) and Eastern Cooperative Oncology Group (ECOG) performance status (0 vs 1) and prior immunotherapy for unresectable or metastatic disease (yes vs no).
The primary efficacy outcome measure was progression-free survival (PFS) of Combo 450 compared with vemurafenib as assessed by a blinded independent review committee (BIRC). PFS as assessed by investigators (investigator assessment) was a supportive analysis. An additional secondary endpoint included PFS of Combo 450 compared with Enco 300. Other secondary efficacy comparisons between Combo 450 and either vemurafenib or Enco 300 included overall survival (OS), objective response rate (ORR), duration of response (DoR) and disease control rate (DCR) as assessed by BIRC and by investigator assessment.
The median age of patients was 56 years (range 20-89), 58% were male, 90% were Caucasian, and 72% of patients had baseline ECOG performance status of 0. Most patients had metastatic disease (95%) and were Stage IVM1c (64%); 27% of patients had elevated baseline serum lactate dehydrogenase (LDH), and 45% of patients had at least 3 organs with tumour involvement at baseline and 3.5% had brain metastases. 27 patients (5%) had received prior checkpoint inhibitors (anti-PD1/PDL1 or ipilimumab) (8 patients in Combo 450 arm (4%); 7 patients in vemurafenib arm (4%); 12 patients in Enco 300 arm (6%) including 22 patients in the metastatic setting (6 patients in Combo 450 arm; 5 patients in vemurafenib arm; 11 patients in Enco 300 arm) and 5 patients in the adjuvant setting (2 patients in Combo 450 arm; 2 patients in vemurafenib arm; 1 patient in Enco 300 arm.
The median duration of exposure was 11.7 months in patients treated with Combo 450, 7.1 months in patients treated with encorafenib 300 mg and 6.2 months in patients treated with vemurafenib. The median relative dose intensity (RDI) for Combo 450 was 99.6% for binimetinib and 100% for encorafenib the median RDI was 86.2% for Enco 300 and 94.5% for vemurafenib.
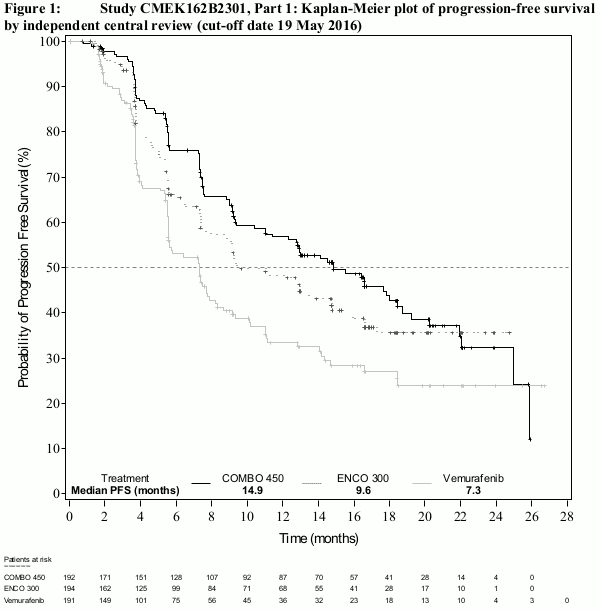
Part 1 of study CMEK162B2301 demonstrated a statistically significant improvement in PFS in the patients treated with Combo 450 compared with patients treated with vemurafenib. Table 4 and Figure 1 summarise the PFS and other efficacy results based on central review of the data by a blinded independent radiology committee.
The efficacy results based on investigator assessment were consistent with the independent central assessment. Unstratified subgroup analyses demonstrated point estimates in favour of Combo 450, including LDH at baseline, ECOG performance status and AJCC stage.
Table 4. Study CMEK162B2301, Part 1: Progression-free survival and confirmed overall response results (independent central review):
| Encorafenib + binimetinib n=192 (Combo 450) | Encorafenib n=194 (Enco 300) | Vemurafenib n=191 (Vem) | |
|---|---|---|---|
| Cut-off date: 19 May 2016 | |||
| PFS (primary analysis) | |||
| Number of events (progressive disease(PD)) (%) | 98 (51.0) | 96 (49.5) | 106 (55.5) |
| Median, months (95% CI) | 14.9 (11.0, 18.5) | 9.6 (7.5,14.8) | 7.3 (5.6, 8.2) |
| HRa (95% CI) (vs Vem) p value (stratified log-rank)b | 0.54 (0.41, 0.71) <0.001 | ||
| HRa (95% CI) (vs. Vem) Nominal p-value | 0.68 (0.52, 0.90) 0.007 | ||
| HRa (95% CI) (vs Enco 300) p value (stratified log-rank)b | 0.75 (0.56, 1.00) 0.051 | ||
| Confirmed overall responses | |||
| Overall response rate, n (%) (95% CI) | 121 (63.0) (55.8, 69.9) | 98 (50.5) (43.3, 57.8) | 77 (40.3) (33.3, 47.6) |
| CR, n (%) | 15 (7.8) | 10 (5.2) | 11 (5.8) |
| PR, n (%) | 106 (55.2) | 88 (45.4) | 66 (34.6) |
| SD, n (%) | 46 (24.0) | 53 (27.3) | 73 (38.2) |
| DCR, n (%) (95% CI) | 177 (92.2) (87.4, 95.6) | 163 (84.0) (78.1, 88.9) | 156 (81.7) (75.4, 86.9) |
| Duration of response | |||
| Median, months (95% CI) | 16.6 (12.2, 20.4) | 14.9 (11.1, NE) | 12.3 (6.9, 16.9) |
| Updated analysis, cut-off date: 07 November 2017 | |||
| PFS | |||
| Number of events (progressive disease) (%) | 113 (58.9) | 112 (57.7) | 118 (61.8) |
| Median, months (95% CI) | 14.9 (11.0, 20.2) | 9.6 (7.4,14.8) | 7.3 (5.6, 7.9) |
| HRa (95% CI) (vs Vem) Nominal p-value | 0.51 (0.39, 0.67) <0.001 | ||
| HRa (95% CI) (vs Vem) Nominal p-value | 0.68 (0.52, 0.88) 0.0038 | ||
| HRa (95% CI) (vs Enco 300) Nominal p-value | 0.77 (0.59,1.00) 0.0498 | ||
CI = confidence interval; CR = complete response; DCR = disease control rate (CR+PR+SD+Non-CR/Non-PD; Non-CR/Non-PD applies only to patients without a target lesion who did not achieve CR or have PD); HR = hazard ratio; NE = not estimable; PFS = progression-free survival; PR = partial response; SD = stable disease. Vem = vemurafenib.
a Hazard ratio based on a stratified Cox proportional hazard model
b Log-rank p-value (2-sided)
Figure 1. Study CMEK162B2301, Part 1: Kaplan-Meier plot of progression-free survival by independent central review (cut-off date 19 May 2016):
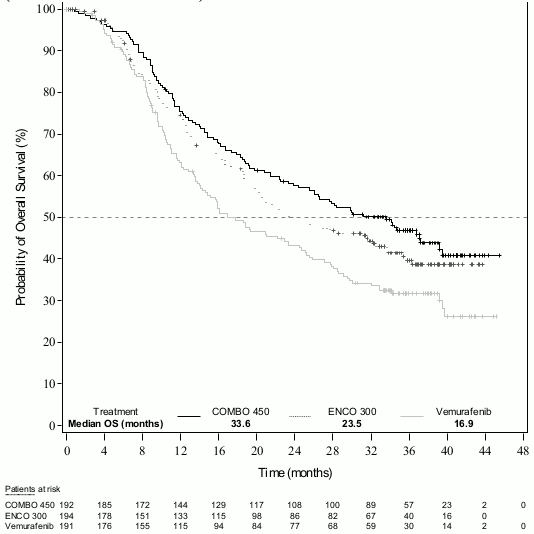
An interim OS analysis of study CMEK162B2301 Part 1, (cut-off date 07 November 2017) demonstrated a statistically significant improvement in OS for Combo 450 compared with vemurafenib (see Table 5 and Figure 2).
A similar proportion of patients in each treatment arm received subsequent treatment with checkpoint inhibitors, mainly pembrolizumab, nivolumab and ipilimumab (34.4% Combo 450 arm, 36.1% encorafenib arm, 39.8% vemurafenib arm).
Table 5. Study CMEK162B2301, Part 1: Overall survival interim results (cut-off date: 7 November 2017):
| Encorafenib + binimetinib n=192 (Combo 450) | Encorafenib n=194 (Enco 300) | Vemurafenib n=191 (Vem) | |||||
|---|---|---|---|---|---|---|---|
| OS | |||||||
| Number of Events (%) | 105 (54.7) | 106 (54.6) | 127 (66.5) | ||||
| Median, months (95% CI) | 33.6 (24.4, 39.2) | 23.5 (19.6, 33.6) | 16.9 (14.0, 24.5) | Survival at 12 months (95% CI) | 75.5% (68.8, 81.0) | 74.6% (67.6, 80.3) | 63.1% (55.7, 69.6) |
| Survival at 24 months (95% CI) | 57.6% (50.3, 64.3) | 49.1% (41.5, 56.2) | 43.2% (35.9, 50.2) | ||||
| HRa (95% CI) (vs Vem) p-value (stratified log-rank) | 0.61 (0.47, 0.79) <0.0001 | ||||||
| HRa (95% CI) (vs. Enco 300) p-value (stratified log-rank) | 0.81 (0.61,1.06) 0.061 | ||||||
a Hazard ratio based on a stratified Cox proportional hazard mode
Figure 2. Study CMEK162B2301, Part 1: Kaplan-Meier plot of interim overall survival:
Quality of Life (QoL) (cut-off date: 19 May 2016)
The Functional Assessment of Cancer Therapy-Melanoma (FACT-M), the European Organisation for Research and Treatment of Cancer's core quality of life questionnaire (EORTC QLQ-C30) and the EuroQoL-5 Dimension-5 Level examination (EQ-5D-5L) were used to explore patient-reported outcomes (PRO) measures of health-related Quality of Life, functioning, melanoma symptoms, and treatment-related adverse reaction. A definitive 10% deterioration in FACT-M and in EORTC QLQ-C30 was significantly delayed in patients treated with Combo 450 relative to other treatments. The median time to definitive 10% deterioration in the FACT-M score was not reached in the Combo 450 arm and was 22.1 months (95% CI: 15.2, NE) in the vemurafenib arm with a HR for the difference of 0.46 (95% CI: 0.29, 0.72). An analysis of time to definitive 10% deterioration in EORTC QLQ-C30 score provided with similar results.
Patients receiving Combo 450 reported no change or a slight improvement in the mean change from baseline EQ-5D-5L index score at all visits, whilst patients receiving vemurafenib or encorafenib reported decreases at all visits (with statistical significant differences). An evaluation of change over time in score yielded the same trend for EORTC QLQ-C30 and at all visit for FACT-M.
Study CMEK162B2301, Part 2
Part 2 of study CMEK162B2301 was designed to assess the contribution of binimetinib to the encorafenib and binimetinib combination.
The PFS for encorafenib 300 mg orally daily used in combination with binimetinib 45 mg orally twice daily (Combo 300, n=258) was compared to the PFS for Enco 300 (n=280, including 194 patients from Part 1 and 86 patients from Part 2). Enrolment in Part 2 started after all Part 1 patients were randomised.
Preliminary Part 2 data at a cut-off date of 9 November 2016 demonstrated the contribution of binimetinib with an improved median PFS estimate of 12.9 months (95% CI: 10.1, 14.0) for Combo 300 compared to 9.2 months (95% CI: 7.4, 11.0) for Enco 300 (Parts 1 and 2) per independent central review (BIRC). Similar results were observed per Investigator assessment. The confirmed ORR per BIRC was 65.9% (95% CI: 59.8, 71.7) for Combo 300, and 50.4% (95% CI 44.3, 56.4) for Enco 300 (Parts 1 and 2). Median DOR for confirmed responses per BIRC was 12.7 months [95% CI: 9.3, 15.1] for Combo 300 and 12.9 months [95% CI: 8.9, 15.5] for Enco 300. The median duration of treatment was longer for Combo 300 vs. Enco 300, 52.1 weeks vs 31.5 weeks.
BRAF V600E Mutant advanced Non-small cell lung cancer – Study ARRAY-818-202
The safety and efficacy of binimetinib in combination with encorafenib were studied in a Phase II, open-label, multicentre, non-comparative study (Study ARRAY-818-202, PHAROS). Patients were required to have histologically-confirmed metastatic NSCLC with a BRAF V600E mutation, ECOG performance status of 0 or 1, and measurable disease. Patients had received 0 or 1 prior line of systemic therapy in the metastatic setting. Prior use of BRAF inhibitors or MEK inhibitors was prohibited.
Patients were enrolled based on the determination of a BRAF V600E mutation in tumour tissue or blood (e.g., ctDNA genetic testing) by a local laboratory assay. Central confirmation of the BRAF V600E mutation status (i.e. any short variant with protein effect V600E) was performed on archival or fresh tumour tissue collected at enrolment and utilized the FoundationOne CDx – F1CDx (tissue) assay.
The analytical sensitivity was assessed through the Limit of Detection (LoD) study for F1CDx using the hit rate method (defined as the lowest level with ≥95% detection) by evaluating variant allele frequency (VAF) for short variants. For F1CDx, the median LoD for substitution was determined to be 3.2% VAF.
A total of 98 patients were enrolled and treated with binimetinib 45 mg orally twice daily and encorafenib 450 mg orally once daily. Treatment continued until disease progression or unacceptable toxicity.
The primary efficacy outcome measure was objective response rate (ORR) and was according to RECIST v1.1 as evaluated by an Independent Radiology Review (IRR). Secondary endpoints included duration of response (DoR), disease control rate (DCR), PFS and OS. Results of the primary analysis with 18.2 months for treatment naïve and 12.8 months previously treated patients are presented below.
Of the 98 patients enrolled in this study, 59 (60.2%) were treatment naïve. The median age of patients was 70 years (47-86), 53% were female, 88% were white and 30% had never smoked. 74% had a baseline ECOG performance status of 1 (67.8% of participants had a baseline PS 1 in the treatment naïve population and 82.1% in the previously treated population). All patients had metastatic disease of which 8% had brain metastases at baseline and 97% had adenocarcinoma.
At the time of the primary analysis, the median duration of exposure was 15.1 months in treatment naïve patients and 5.4 months in previously treated patients. In the overall population, the median relative dose intensity (RDI) was 95.4% for binimetinib and 99.2% for encorafenib.
At the time of the primary analysis, the primary endpoint of IRR-assessed ORR in the treatment naïve population was 74.6% (95% CI: 61.6, 85.0), including 9 (15.3%) CRs and 35 (59.3%) PRs. The ORR by IRR in the previously treated population was 46.2% (95% CI: 30.1, 62.8), including 4 (10.3%) CRs and 14 (35.9%) PRs.
Results updated with an additional 10-month follow-up (median duration of exposure of 16.3 months in treatment naïve patients and 5.5 months in previously treated patients) are provided in Table 6.
Table 6. Study ARRAY-818-202: Efficacy Results:
| Binimetinib with Encorafenib | ||
|---|---|---|
| Treatment Naïve (N=59) | Previously Treated (N=39) | |
| ORR per IRR | ||
| ORR, % (95% CI) | 75% (62, 85) | 46% (30, 63) |
| CR, % | 15% | 10% |
| PR, % | 59% | 36% |
| DoR per IRR | N=44 | N=18 |
| Median DoR, months (95% CI) | 40.0 (23.1, NE)* | 16.7 (7.4, NE)* |
| % with DoR ≥12 months | 64% | 44% |
* Results from a sensitivity analysis considering new anti-cancer therapy as an event in addition to progression and death are 23.1 months in treatment naïve patients (14.8; NE) and 12.0 months (6.3; NE) in previously treated patients.
N = number of patients; ORR = Objective Response Rate; CI = Confidence Interval; CR = Complete Response; PR = Partial Response; DoR = Duration of Response; IRR= Independent Radiology Review; NE = not estimable
Cardiac electrophysiology
In the safety analysis of pooled studies, the incidence of new QTcF prolongation >500 ms was 1.1% (4/363) in the Combo 450 ISP (n=372), and 2.5% (5/203) in the encorafenib single agent group of patients with melanoma. QTcF prolongation of >60 ms compared to pre-treatment values was observed in 6.0% (22/364) patients in the Combo 450 ISP, and in 3.4% (7/204) in the encorafenib single agent group (see section 5.1 of encorafenib SmPC).
Paediatric population
The European Medicines Agency has deferred the obligation to submit the results of studies with binimetinib in one or more subsets of the paediatric population in melanoma (see section 4.2 for information on paediatric use).
The European Medicines Agency has waived the obligation to submit the results of studies with binimetinib in all subsets of the paediatric population in lung cancer (see section 4.2 for information on paediatric use).
Pharmacokinetic properties
The pharmacokinetics of binimetinib were studied in healthy subjects and patients with solid tumours. After repeat twice-daily dosing concomitantly with encorafenib, steady-state conditions for binimetinib were reached within 15 days with no major accumulation. The mean (CV %) Cmax,ss was 654 ng/mL (34.7%) and mean AUCss was 2.35 ug.h/mL (28.0%) in combination with encorafenib as estimated by population PK modelling in patients with unresectable or metastatic BRAF V600 mutant melanoma. Binimetinib pharmacokinetics have been shown to be approximately dose-linear.
Absorption
After oral administration, binimetinib is rapidly absorbed with a median Tmax of 1.5 hours. Following a single oral dose of 45 mg [14C] binimetinib in healthy subjects, at least 50% of the binimetinib dose was absorbed. Administration of a single 45 mg dose of binimetinib with a high-fat, high-calorie meal decreased the maximum binimetinib concentration (Cmax) by 17%, while the area under the concentration-time curve (AUC) was unchanged. A drug interaction study in healthy subjects indicated that the extent of binimetinib exposure is not altered in the presence of a gastric pH-altering agent (rabeprazole).
Distribution
Binimetinib is 97.2% bound to human plasma proteins in vitro. Binimetinib is more distributed in plasma than blood. In humans, the blood-to-plasma ratio is 0.718. Following a single oral dose of 45 mg [14C] binimetinib in healthy subjects, the apparent volume of distribution (Vz/F) of binimetinib is 374 L.
Biotransformation
Following a single oral dose of 45 mg [14C] binimetinib in healthy subjects, the primary biotransformation pathways of binimetinib observed in humans include glucuronidation, N-dealkylation, amide hydrolysis, and loss of ethane-diol from the side chain. The maximum contribution of direct glucuronidation to the clearance of binimetinib was estimated to have been 61.2%. Following a single oral dose of 45 mg [14C] binimetinib in healthy subjects, approximately 60% of the circulating radioactivity AUC in plasma was attributable to binimetinib. In vitro, CYP1A2 and CYP2C19 catalyse the formation of the active metabolite, which represents less than 20% of the binimetinib exposure clinically.
Elimination
Following a single oral dose of 45 mg [14C] binimetinib in healthy subjects, a mean of 62.3% of the radioactivity was eliminated in the feces while 31.4% was eliminated in the urine. In urine, 6.5% of the radioactivity was excreted as binimetinib. The mean (CV %) apparent clearance (CL/F) of binimetinib was 28.2 L/h (17.5%). The median (range) binimetinib terminal half-life (T1/2) was 8.66 h (8.10 to 13.6 h).
Medicinal product interactions
Effect of UGT1A1 inducers or inhibitors on binimetinib
Binimetinib is primarily metabolised through UGT1A1 mediated glucuronidation. In clinical study sub-analysis, however, there was no apparent relationship observed between binimetinib exposure and UGT1A1 mutation status. In addition, simulations to investigate the effect of 400 mg atazanavir (UGT1A1 inhibitor) on the exposure of 45 mg binimetinib predicted similar binimetinib Cmax in the presence or absence of atazanavir. Therefore, the extent of drug interactions mediated by UGT1A1 is minimal, and unlikely clinically relevant; however, as this has not been evaluated in a formal clinical study, UGT1A1 inducers or inhibitors should be administered with caution.
Effect of CYP enzymes on binimetinib
In vitro, CYP1A2 and CYP2C19 catalyse the formation of the active metabolite, AR00426032 (M3) by oxidative N-desmethylation.
Effect of binimetinib on CYP substrates
Binimetinib is a weak reversible inhibitor of CYP1A2 and CYP2C9.
Effect of transporters on binimetinib
In vitro experiments indicate that binimetinib is a substrate of P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP). Inhibition of P-gp or BCRP is unlikely to result in a clinically important increase in binimetinib concentrations as binimetinib exhibits moderate to high passive permeability.
Effect of binimetinib on transporters
Binimetinib is a weak inhibitor of OAT3. No clinicallly significant drug-drug interactions caused by binimetinib on other transporters is expected.
Binimetinib is metabolised by UGTs and CYP1A2 and is a substrate for Pgp. Specific inducers of these enzymes have not been studied and may result in a loss of efficacy.
Special populations
Age, body weight
Based on a population pharmacokinetic analysis, age or body weight do not have a clinically important effect on the systemic exposure of binimetinib.
Gender
Based on a population pharmacokinetic (PK) analysis, the PK of binimetinib were similar in males as compared with females.
Race
There are insufficient data to evaluate potential differences in the exposure of binimetinib by race or ethnicity.
Hepatic impairment
As binimetinib is primarily metabolised and eliminated via the liver, patients with moderate to severe hepatic impairment may have increased exposure. Results from a dedicated clinical study with binimetinib only indicate similar exposures in patients with mild impairment (Child-Pugh Class A) and subjects with normal liver function. A two-fold increase in total binimetinib exposure (AUC) was observed in patients with moderate (Child-Pugh Class B) and severe (Child-Pugh Class C) hepatic impairment (see section 4.2). This increase expends to three fold in both moderate and severe hepatic impairment when considering unbound binimetinib exposure (see section 4.2).
Gilbert's syndrome
Binimetinib has not been evaluated in patients with Gilbert's disease. The main route of hepatic transformation of binimetinib being glucoronidation, the decision for treatement should be made by the treating physician taking into account the individual benefit-risk.
Renal impairment
Binimetinib undergoes minimal renal elimination. Results from a dedicated clinical study showed that patients with severe renal impairment (eGFR ≤29 mL/min/1.73 m²), had a 29% increase in exposure (AUCinf), a 21% increase in Cmax, and a 22% decrease in CL/F compared to matching healthy subjects. These differences were within the variability observed for these parameters in both cohorts of this study (25% - 49%) and the variability previously observed in patient clinical studies, hence these differences are unlikely to be clinically relevant.
The effects of renal impairment on the pharmacokinetics of binimetinib in combination with encorafenib have not been evaluated clinically.
Preclinical safety data
Repeated oral administration of binimetinib in rats for up to 6 months was associated with soft tissue mineralisation, gastric mucosal lesions and reversible minimal to mild clinical pathology changes at 7 to 12.5 times human therapeutic exposures. In a gastric irritation study in rats, an increased incidence of superficial mucosal lesions and of hemorrhagic ulcers were observed. In cynomolgus monkeys, oral administration of binimetinib was associated with gastro-intestinal intolerance, moderate clinical pathology changes, bone marrow hypercellularity and microscopic findings of gastrointestinal inflammation, reversible at the lowest doses which were below human therapeutic exposures.
Carcinogenic potential of binimetinib was not evaluated. Standard genotixicity studies with binimetinib were negative.
The potential embryo-foetal effects of binimetinib were evaluated in rats and rabbits. In rats, lower gestational body weight gain and fetal body weights and a decreased number of ossified fetal sternebrae were noted. No effects were noted at 14-times the human therapeutic exposure. In rabbits, mortality, maternal physical signs of toxicity, lower gestational body weight and abortion were noted. The number of viable foetuses and foetal body weights were reduced and post-implantation loss and resorptions were increased. An increased litter incidence of foetal ventricular septal defects and pulmonary trunk alterations was noted at the highest doses. No effects were observed at 3times the human therapeutic exposure.
Fertility studies were not conducted with binimetinib. In repeat-dose toxicity studies, no concern in terms of fertility was raised from pathological examination of reproductive organs in rats and monkeys.
Binimetinib has phototoxic potential in vitro.
A minimal risk for photosensitisation was shown in vivo at an oral dose providing 3.8-fold higher exposure than that achieved with the recommended dose in humans. These data indicate that there is minimal risk for phototoxicity with binimetinib at therapeutic doses in patients.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.