PREZCOBIX Film-coated tablet Ref.[50500] Active ingredients: Cobicistat Darunavir
Source: FDA, National Drug Code (US) Revision Year: 2022
12.1. Mechanism of Action
PREZCOBIX is a fixed-dose combination of an HIV-1 antiviral drug, darunavir and a CYP3A inhibitor, cobicistat [see Microbiology (12.4)].
12.2. Pharmacodynamics
Cardiac Electrophysiology
Separate thorough QT trials have been conducted for darunavir co-administered with ritonavir and for cobicistat. The effect of darunavir co-administered with cobicistat on the QT interval has not been evaluated.
Darunavir
In a thorough QT/QTc study in 40 healthy subjects, darunavir doses (co-administered with 100 mg ritonavir) of approximately 2 times the recommended darunavir dose did not affect the QT/QTc interval.
Cobicistat
The effect of a single dose of cobicistat 250 mg and 400 mg (approximately 1.7 and 2.7 times the recommended dose) on QTc interval was evaluated in a randomized, placebo- and active-controlled (moxifloxacin 400 mg) four-period crossover thorough QT trial in 48 healthy subjects. In this trial, no significant QTc prolongation effect of cobicistat was detected. The dose of 400 mg cobicistat is expected to provide information on a high exposure clinical scenario. Prolongation of the PR interval was noted in subjects receiving cobicistat in the same trial. The maximum mean (95% upper confidence bound) difference in PR from placebo after baseline-correction was 9.5 (12.1) msec for 250 mg and 20.2 (22.8) msec for 400 mg of cobicistat.
Effects on Serum Creatinine
Cobicistat
The effect of cobicistat on serum creatinine was investigated in a trial in subjects with normal renal function (eGFR ≥80 mL/min, N=12) and mild-to-moderate renal impairment (eGFR 50–79 mL/min, N=18). A statistically significant decrease in the estimated glomerular filtration rate, calculated by Cockcroft-Gault method (eGFRCG) from baseline, was observed after 7 days of treatment with cobicistat 150 mg among subjects with normal renal function (-9.9 ± 13.1 mL/min) and mild-to-moderate renal impairment (-11.9 ± 7.0 mL/min). No statistically significant changes in eGFRCG were observed compared to baseline for subjects with normal renal function or mild-to-moderate renal impairment 7 days after cobicistat was discontinued. The actual glomerular filtration rate, as determined by the clearance of probe drug iohexol, was not altered from baseline following treatment of cobicistat among subjects with normal renal function and mild-to-moderate renal impairment, indicating that cobicistat inhibits tubular secretion of creatinine, reflected as a reduction in eGFRCG, without affecting the actual glomerular filtration rate.
12.3. Pharmacokinetics
The pharmacokinetics of darunavir co-administered with cobicistat (150 mg) have been evaluated in healthy adult subjects and in HIV-1 infected subjects.
Darunavir is primarily metabolized by CYP3A. Cobicistat inhibits CYP3A, thereby increasing the plasma concentrations of darunavir.
Under fed (535 total kcal, 171 kcal from fat, 268 kcal from carbohydrates, 96 kcal from protein) and fasted conditions in healthy subjects, the 90% confidence intervals when comparing darunavir exposure between PREZCOBIX and darunavir 800 mg co-administered with cobicistat 150 mg as single entities were within 80–125%.
Darunavir exposure when comparing darunavir co-administered with cobicistat (as single entities) to darunavir co-administered with ritonavir was evaluated in a relative bioavailability trial [see cobicistat full prescribing information]. Table 2 displays the population pharmacokinetic estimates of darunavir after oral administration of darunavir 800 mg co-administered with ritonavir 100 mg once daily (based on sparse sampling in 335 subjects in Trial TMC114-C211 and 280 subjects in Trial TMC114-C229) and darunavir 800 mg co-administered with cobicistat 150 mg once daily administered as single entities (based on sparse sampling in 298 subjects in Trial GS-US-216-0130) to HIV-1 infected subjects.
Table 2. Population Pharmacokinetic Estimates of Darunavir as Darunavir 800 mg Co-administered with Ritonavir 100 mg Once Daily (Trial TMC114-C211, 48 Week Analysis and Trial TMC114-C229, 48 Week Analysis) and Darunavir 800 mg Co-administered with Cobicistat 150 mg Once Daily (Trial GS-US-216-130, 24 Week Analysis):
| Trial TMC114-C211 (treatment-naïve) Darunavir 800 mg co-administered with ritonavir 100 mg once daily | Trial TMC114-C229 (treatment-experienced) Darunavir 800 mg co-administered with ritonavir 100 mg once daily | Trial GS-US-216-0130 (treatment-naïve and experienced) Darunavir 800 mg co-administered with cobicistat 150 mg once daily | |
|---|---|---|---|
| Parameter | N=335 | N=280 | N=298 |
| AUC24h (ng∙h/mL) | |||
| Mean ± Standard Deviation | 93026 ± 27050 | 93334 ± 28626 | 100152 ± 32042 |
| Median (Range) | 87854 (45000–219240) | 87788 (45456–236920) | 96900 (34500–224000) |
| C0h (ng/mL) | |||
| Mean ± Standard Deviation | 2282 ± 1168 | 2160 ± 1201 | 2043 ± 1257 |
| Median (Range) | 2041 (368–7242) | 1896 (184–7881) | 1875 (70–6890) |
N=number of subjects with data
Absorption and Bioavailability
In healthy subjects, under fed conditions, when single doses of the darunavir and cobicistat fixed-dose combination tablet were administered, the maximum plasma concentration was achieved within approximately 4 to 4.5 hours for darunavir and approximately 4 to 5 hours for cobicistat.
Effects of Food on Oral Absorption
When compared to fasted conditions, administration of PREZCOBIX to healthy adult subjects with a high-fat meal (965 total kcal: 129 kcal from protein, 236 kcal from carbohydrates and 600 kcal from fat) resulted in a 70% increase in AUC(0–inf) and a 127% increase in Cmax for darunavir. Cobicistat exposures were not affected by food. PREZCOBIX should be taken with food.
Distribution
Darunavir: Darunavir is approximately 95% bound to plasma proteins. Darunavir binds primarily to plasma alpha 1-acid glycoprotein (AAG).
Cobicistat: Cobicistat is 97–98% bound to human plasma proteins and the mean blood–to-plasma ratio was approximately 0.5.
Metabolism
Darunavir: In vitro experiments with human liver microsomes (HLMs) indicate that darunavir primarily undergoes oxidative metabolism. Darunavir is extensively metabolized by CYP enzymes, primarily by CYP3A. A mass balance trial in healthy subjects showed that after single dose administration of 400 mg 14C-darunavir co-administered with 100 mg ritonavir, the majority of the radioactivity in the plasma was due to darunavir. At least 3 oxidative metabolites of darunavir have been identified in humans; all showed activity that was at least 90% less than the activity of darunavir against wild-type HIV-1.
Cobicistat: Cobicistat is metabolized by CYP3A and to a minor extent by CYP2D6 enzymes and does not undergo glucuronidation.
Elimination
Darunavir: A mass balance trial in healthy subjects showed that after single dose administration of 400 mg 14C-darunavir co-administered with 100 mg ritonavir, approximately 79.5% and 13.9% of the administered dose of 14C-darunavir was recovered in the feces and urine, respectively. Unchanged darunavir accounted for approximately 41.2% and 7.7% of the administered dose in feces and urine, respectively.
When single doses of the darunavir and cobicistat fixed-dose combination tablet were administered, the terminal elimination half-life of darunavir was approximately 7 hours under fed conditions.
Cobicistat: When single doses of the darunavir and cobicistat fixed-dose combination tablet were administered, the terminal elimination half-life of cobicistat was approximately 4 hours under fed conditions. With single dose administration of 14C-cobicistat after multiple dosing of cobicistat for six days, the mean percent of the administered dose excreted in feces and urine was 86.2% and 8.2%, respectively.
Specific Populations
Hepatic Impairment
Darunavir: Darunavir is primarily metabolized by the liver. The steady-state pharmacokinetic parameters of darunavir were similar after multiple dose co-administration of darunavir 600 mg co-administered with ritonavir 100 mg twice daily to subjects with normal hepatic function (n=16), mild hepatic impairment (Child-Pugh Class A, n=8), and moderate hepatic impairment (Child-Pugh Class B, n=8). The effect of severe hepatic impairment on the pharmacokinetics of darunavir has not been evaluated [see Use in Specific Populations (8.6)].
Cobicistat: Cobicistat is primarily metabolized by the liver. A trial evaluating the pharmacokinetics of cobicistat was performed in non-HIV-1 infected subjects with moderate hepatic impairment. No clinically relevant differences in cobicistat pharmacokinetics were observed between subjects with moderate hepatic impairment (Child-Pugh Class B) and healthy subjects. The effect of severe hepatic impairment on the pharmacokinetics of cobicistat has not been evaluated [see Use in Specific Populations (8.6)].
Hepatitis B or Hepatitis C Virus Co-Infection
Darunavir: In subjects with HIV-1 infection taking darunavir co-administered with ritonavir, the 48 week analysis of the data from clinical studies in HIV-1 infected subjects indicated that hepatitis B and/or hepatitis C virus co-infection status had no apparent effect on the exposure of darunavir.
The effect of hepatitis B and/or C virus infection on the pharmacokinetics of PREZCOBIX have not been evaluated.
Renal Impairment
Darunavir: Population pharmacokinetic analysis showed that the pharmacokinetics of darunavir were not significantly affected in HIV-1 infected subjects with moderate renal impairment taking darunavir co-administered with ritonavir (creatinine clearance between 30–60 mL/min, n=20). There are no pharmacokinetic data available in HIV-1 infected patients with severe renal impairment or end stage renal disease taking darunavir co-adminstered with either ritonavir or cobicistat [see Use in Specific Populations (8.7)].
Cobicistat: A trial of the pharmacokinetics of cobicistat was performed in non-HIV infected subjects with severe renal impairment (estimated creatinine clearance below 30 mL/min). No clinically relevant differences in cobicistat pharmacokinetics were observed between subjects with severe renal impairment and healthy subjects [see Use in Special Populations (8.7)].
Gender
Darunavir: In subjects with HIV-1 infection taking darunavir co-administered with ritonavir, population pharmacokinetic analysis showed higher mean darunavir exposure in HIV-1 infected females compared to males. This difference is not clinically relevant.
Cobicistat: No clinically relevant pharmacokinetic differences have been observed between men and women for cobicistat.
Race
Darunavir: Population pharmacokinetic analysis of darunavir in HIV-1 infected subjects taking darunavir co-administered with ritonavir indicated that race had no apparent effect on the exposure to darunavir.
Cobicistat: Population pharmacokinetic analysis of cobicistat in HIV-1 infected subjects indicated that race had no clinically relevant effect on the exposure of cobicistat.
Geriatric Patients
Darunavir: In subjects with HIV-1 infection taking darunavir co-administered with ritonavir, population pharmacokinetic analysis showed no considerable differences in darunavir pharmacokinetics for ages 18 to 75 years compared to ages greater than or equal to 65 years (n=12) [see Use in Specific Populations (8.5)].
Cobicistat: Insufficient data are available to determine whether potential differences exist in the pharmacokinetics of cobicistat in geriatric (65 years of age and older) subjects compared to younger subjects.
Pediatric Patients Weighing at Least 40 kg
Available pharmacokinetic data for the different components of PREZCOBIX indicate that there were no clinically relevant differences in exposure between adults and pediatric subjects weighing at least 40 kg.
Darunavir and cobicistat: In pediatric subjects aged 12 to less than 18 years, weighing at least 40 kg who received darunavir 800 mg co-administered with cobicistat 150 mg (N=7), geometric mean darunavir Cmax values were similar between adults and pediatric subjects. Geometric mean darunavir AUC24h and C24h values were 15% and 32% lower, with geometric mean ratios of 0.85 (90% CI: 0.64, 1.13) and 0.68 (90% CI: 0.30, 1.55) in pediatric subjects relative to adults, respectively. These differences were not considered clinically significant. Geometric mean cobicistat AUC24h, Cmax, and C24h values were comparable in pediatric subjects and adults (Table 3).
Table 3. Multiple-Dose PK Parameters of Darunavir and Cobicistat Following Administration of Darunavir with Cobicistat in HIV-1 Infected Adults and Pediatric Subjects Weighing at least 40 kg*:
| Parameter Geometric mean (CV%) | Darunavir | Cobicistat |
|---|---|---|
| Pediatric Subjects* | N=7 | N=7 |
| AUC24h (mcg.hr/mL) | 77.22 (29.5) | 8.33 (34.9) |
| Cmax (mcg/mL) | 7.32 (21.7) | 1.10 (20.0) |
| C24h (mcg/mL) | 0.68 (91.6) | 0.02 (123.9)† |
| Adults‡ | N=21 | N=21 |
| AUC24h (mcg.hr/mL) | 90.56 (45.3) | 7.69 (43.9) |
| Cmax (mcg/mL) | 8.34 (33.3) | 1.04 (35.3) |
| C24h (mcg/mL) | 1.00 (108.0) | 0.02 (135.1)§ |
CV = Coefficient of Variation; mcg = microgram
* From intensive PK analysis of trial GS-US-216-0128, where subjects with HIV-1 infection were administered darunavir 800 mg and cobicistat 150 mg once daily with 2 NRTIs
† N=5; Data from two subjects who had undetectable cobicistat C24h concentrations were excluded from summary statistics
‡ From intensive PK analysis of trial GS-US-299-0102 where subjects with HIV-1 infection were administered darunavir/cobicistat/emtricitabine/tenofovir alafenamide
§N=18
Pregnancy and Postpartum
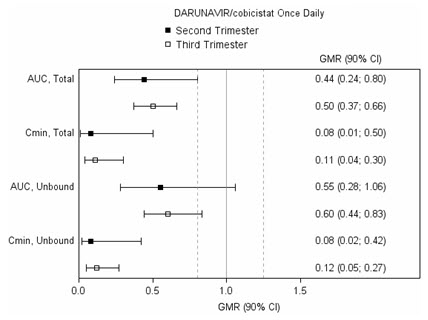
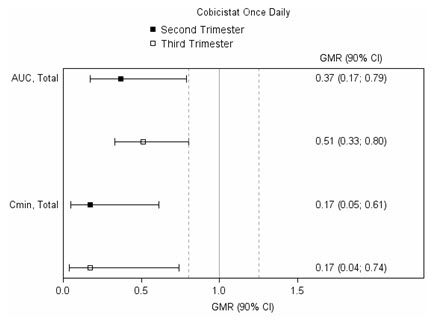
The exposure to total and unbound darunavir boosted with cobicistat after intake of PREZCOBIX as part of an antiretroviral regimen was substantially lower during the second and third trimesters of pregnancy compared with 6–12 weeks postpartum (see Table 4 and Figure 1).
Table 4. Pharmacokinetic Results of Total Darunavir after Administration of PREZCOBIX Once Daily as Part of an Antiretroviral Regimen, During the 2nd Trimester of Pregnancy, the 3 rd Trimester of Pregnancy, and Postpartum:
| Pharmacokinetics of total darunavir (mean ± SD) | 2 nd Trimester of pregnancy N=7 | 3rd Trimester of pregnancy N=6 | Postpartum (6–12 weeks) N=6 |
|---|---|---|---|
| Cmax, ng/mL | 4340 ± 1616 | 4910 ± 970 | 7918 ± 2199 |
| AUC24h, ng.h/mL | 47293 ± 19058 | 47991 ± 9879 | 99613 ± 34862 |
| Cmin, ng/mL | 168 ± 149 | 184 ± 99 | 1538 ± 1344 |
Figure 1. Pharmacokinetic Results (Within-Subject Comparison) of Total and Unbound Darunavir and Total Cobicistat after Administration of PREZCOBIX at 800/150 mg Once Daily as Part of an Antiretroviral Regimen, During the 2nd and 3rd Trimester of Pregnancy Compared to Postpartum:
Legend: 90% CI: 90% confidence interval; GMR: geometric mean ratio (i.e. second or third trimester/postpartum). Solid vertical line: ratio of 1.0; dotted vertical lines: reference lines of 0.8 and 1.25.
Drug Interactions
Darunavir is metabolized by CYP3A. Cobicistat is metabolized by CYP3A and, to a minor extent, by CYP2D6. Darunavir co-administered with cobicistat is an inhibitor of CYP3A and CYP2D6. Cobicistat inhibits the following transporters: P-gp, BCRP, MATE1, OATP1B1, and OATP1B3. Based on in vitro data, cobicistat is not expected to induce CYP1A2 or CYP2B6 and based on in vivo data, cobicistat is not expected to induce MDR1 or, in general, CYP3A to a clinically significant extent. The induction effect of cobicistat on CYP2C9, CYP2C19, or UGT1A1 is unknown, but is expected to be low based on CYP3A in vitro induction data [see Drug Interactions (7)].
A drug-drug interaction study between darunavir/cobicistat and dabigatran etexilate was conducted in healthy participants. The effects of darunavir on co-administration with dabigatran etexilate are summarized in Table 5.
Table 5. Drug Interactions: Pharmacokinetic Parameters for Co-Administered Drugs in the Presence of darunavir/cobicistat:
| Co-administered drug | Dose/Schedule | N | PK | LS Mean ratio (90% CI) of co-administered drug pharmacokinetic parameters with/without darunavir no effect =1.00 | |||
|---|---|---|---|---|---|---|---|
| Co-administered drug | Darunavir/cobicistat | Cmax | AUC | Cmin | |||
| Dabigatran etexilate | 150 mg | 800/100 mg single dose | 14 | ↑ | 2.64 (2.29–3.05) | 2.64 (2.32–3.00) | - |
| 800/100 mg q.d.* | 14 | ↑ | 1.99 (1.72–2.30) | 1.88 (1.65–2.13) | - | ||
N = number of subjects with data
q.d. = once daily
* 800/100 mg q.d. for 14 days before co-administered with dabigatran
etexilate.
12.4. Microbiology
Mechanism of Action
Darunavir: Darunavir is an inhibitor of the HIV-1 protease. It selectively inhibits the cleavage of HIV-1 encoded Gag-Pol polyproteins in infected cells, thereby preventing the formation of mature virus particles.
Cobicistat: Cobicistat is a selective, mechanism-based inhibitor of cytochromes P450 of the CYP3A subfamily. Inhibition of CYP3A-mediated metabolism by cobicistat enhances the systemic exposure of CYP3A substrates.
Antiviral Activity
Darunavir: Darunavir exhibits activity against laboratory strains and clinical isolates of HIV-1 and laboratory strains of HIV-2 in acutely infected T-cell lines, human peripheral blood mononuclear cells, and human monocytes/macrophages with median EC50 values ranging from 1.2 to 8.5 nM (0.7 to 5.0 ng/mL). Darunavir demonstrates antiviral activity in cell culture against a broad panel of HIV-1 group M (A, B, C, D, E, F, G), and group O primary isolates with EC50 values ranging from less than 0.1 to 4.3 nM. The EC50 value of darunavir increases by a median factor of 5.4 in the presence of human serum. Darunavir did not show antagonism when studied in combination with the HIV protease inhibitors (PIs) amprenavir, atazanavir, indinavir, lopinavir, nelfinavir, ritonavir, saquinavir, or tipranavir, the N(t)RTIs abacavir, didanosine, emtricitabine, lamivudine, stavudine, tenofovir, zalcitabine, or zidovudine, the NNRTIs delavirdine, efavirenz, etravirine, rilpivirine, or nevirapine, and the fusion inhibitor enfuvirtide.
Cobicistat: Cobicistat does not inhibit recombinant HIV-1 protease in a biochemical assay and has no detectable antiviral activity in cell culture against HIV-1. The antiviral activity in cell culture of approved HIV-1 antiretroviral drugs was not antagonized by cobicistat.
Resistance
Cell Culture
Darunavir: HIV-1 isolates with a decreased susceptibility to darunavir have been selected in cell culture and obtained from subjects treated with darunavir co-administered with ritonavir. Darunavir-resistant virus derived in cell culture from wild-type HIV-1 had 21- to 88-fold decreased susceptibility to darunavir and developed 2 to 4 of the following amino acid substitutions S37D, R41E/T, K55Q, H69Q, K70E, T74S, V77I, or I85V in the protease. Selection in cell culture of darunavir resistant HIV-1 from nine HIV-1 strains harboring multiple PI resistance-associated substitutions resulted in the overall emergence of 22 mutations in the protease gene, coding for amino acid substitutions L10F, V11I, I13V, I15V, G16E, L23I, V32I, L33F, S37N, M46I, I47V, I50V, F53L, L63P, A71V, G73S, L76V, V82I, I84V, T91A/S, and Q92R, of which L10F, V32I, L33F, S37N, M46I, I47V, I50V, L63P, A71V, and I84V were the most prevalent. These darunavir-resistant viruses had at least eight protease substitutions and exhibited 50- to 641-fold decreases in darunavir susceptibility with final EC50 values ranging from 125 nM to 3461 nM.
Clinical Studies
The resistance profile of PREZCOBIX is driven by darunavir. Cobicistat does not select any HIV resistance substitutions, due to its lack of antiviral activity. For the clinical resistance profile of darunavir, refer to the darunavir full prescribing information.
Cross-resistance
Cross-resistance among PIs has been observed. Darunavir has a less than 10-fold decreased susceptibility in cell culture against 90% of 3309 clinical isolates resistant to amprenavir, atazanavir, indinavir, lopinavir, nelfinavir, ritonavir, saquinavir, and/or tipranavir showing that viruses resistant to these PIs remain susceptible to darunavir. A less than 10-fold decreased susceptibility was observed for the other PIs in 26% to 96% of these PI resistant clinical isolates [nelfinavir (26%), ritonavir (34%), lopinavir (46%), indinavir (57%), atazanavir (59%), saquinavir (64%), amprenavir (70%), and tipranavir (96%)].
Cross-resistance between darunavir and nucleoside/nucleotide reverse transcriptase inhibitors, non-nucleoside reverse transcriptase inhibitors, fusion inhibitors, CCR5 co-receptor antagonists, or integrase strand transfer inhibitors is unlikely because the viral targets are different.
Baseline Genotype/Phenotype and Virologic Outcome Analyses
Baseline International AIDS Society (IAS)-defined PI resistance substitutions confer reduced virologic response to darunavir. Please refer to the “Baseline Genotype/Phenotype and Virologic Outcome Analyses” section in the darunavir full prescribing information.
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis and Mutagenesis
Darunavir: Darunavir was evaluated for carcinogenic potential by oral gavage administration to mice and rats up to 104 weeks. Daily doses of 150, 450 and 1000 mg/kg were administered to mice and doses of 50, 150 and 500 mg/kg were administered to rats. A dose-related increase in the incidence of hepatocellular adenomas and carcinomas was observed in males and females of both species and an increase in thyroid follicular cell adenomas was observed in male rats. The observed hepatocellular findings in rodents are considered to be of limited relevance to humans. Repeated administration of darunavir to rats caused hepatic microsomal enzyme induction and increased thyroid hormone elimination, which predispose rats but not humans, to thyroid neoplasms. At the highest tested doses, the systemic exposures to darunavir (based on AUC) were between 0.4- and 0.7-fold (mice) and 0.7- and 1-fold (rats) of exposures observed in humans at the recommended therapeutic doses (darunavir 600 mg co-administered with ritonavir 100 mg twice daily or darunavir 800 mg co-administered with ritonavir 100 mg once daily).
Darunavir was not mutagenic or genotoxic in a battery of in vitro and in vivo assays including bacterial reverse mutation (Ames), chromosomal aberration in human lymphocytes, and in vivo micronucleus test in mice.
Cobicistat: In a long-term carcinogenicity study in mice, no drug-related increases in tumor incidence were observed at doses up to 50 and 100 mg/kg/day in males and females, respectively. Cobicistat exposures at these doses were approximately 7 (male) and 16 (females) times, respectively, the human systemic exposure at the therapeutic daily dose. In a long-term carcinogenicity study of cobicistat in rats, an increased incidence of follicular cell adenomas and/or carcinomas in the thyroid gland was observed at doses of 25 and 50 mg/kg/day in males, and at 30 mg/kg/day in females. The follicular cell findings are considered to be rat-specific, secondary to hepatic microsomal enzyme induction and thyroid hormone imbalance, and are not relevant for humans. At the highest doses tested in the rat carcinogenicity study, systemic exposures were approximately 2 times the human systemic exposure at the therapeutic daily dose.
Cobicistat was not genotoxic in the reverse mutation bacterial test (Ames test), mouse lymphoma or rat micronucleus assays.
Impairment of Fertility
Darunavir: No effects on fertility or early embryonic development were observed with darunavir in rats.
Cobicistat: Cobicistat did not affect fertility in male or female rats at daily exposures (AUC) approximately 4-fold higher than human exposures at the recommended 150 mg daily dose.
Fertility was normal in the offspring of rats exposed daily from before birth (in utero) through sexual maturity at daily exposures (AUC) of approximately 1.2-fold higher than human exposures at the recommended 150 mg daily dose.
14. Clinical Studies
14.1 Clinical Trial Results in Adults with HIV-1 Infection
The efficacy of PREZCOBIX in adults with HIV-1 infection is based on efficacy demonstrated in clinical trials of darunavir co-administered with ritonavir [see darunavir full prescribing information].
14.2 Clinical Trial Results in Pediatric Subjects with HIV-1 Infection
Trial GS-US-216-0128 was a Phase ⅔ multicenter, open-label trial to evaluate the pharmacokinetics, safety, and efficacy of darunavir co-administered with cobicistat in adolescents aged 12 years and older with HIV-1 infection who were virolgically suppressed and had a baseline estimated creatinine clearance ≥90 mL/min/1.73 m². Subjects were on a stable antiretroviral regimen (for at least 3 months), consisting of darunavir administered with ritonavir, combined with 2 NRTIs. These subjects (N=7) were switched from ritonavir to cobicistat 150 mg once daily and continued darunavir and 2 NRTIs.
The median age of subjects was 14 years (range 12–16 years), median weight was 60 kg (range 45–78 kg), and 43% were male. At baseline, all subjects had plasma HIV-1 RNA <50 copies/mL. At Week 48, 86% (6/7) of subjects remained suppressed (HIV-1 RNA <50 copies/mL), and 1 subject had missing data. From a median baseline CD4+ cell count and CD4+% of 1,117 cells/mm³ (range 658 to 2,416 cells/mm³) and 45% (range 28% to 56%), respectively, the median change from baseline in CD4+ cell count and CD4+% at Week 48 was -342 cells/mm³ (range -1,389 to 219 cells/mm³) and -6% (range -12% to 5%), respectively. All 6 subjects with available data had CD4+ cell counts above 800 cells/mm³ at Week 48.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.