RYTHMOL SR Capsule Ref.[11059] Active ingredients: Propafenone
Source: FDA, National Drug Code (US) Revision Year: 2018
12.1. Mechanism of Action
Propafenone is a Class 1C antiarrhythmic drug with local anesthetic effects and a direct stabilizing action on myocardial membranes. The electrophysiological effect of propafenone manifests itself in a reduction of upstroke velocity (Phase 0) of the monophasic action potential. In Purkinje fibers, and, to a lesser extent, myocardial fibers, propafenone reduces the fast inward current carried by sodium ions. Diastolic excitability threshold is increased and effective refractory period prolonged. Propafenone reduces spontaneous automaticity and depresses triggered activity.
Studies in anesthetized dogs and isolated organ preparations show that propafenone has beta-sympatholytic activity at about 1/50 the potency of propranolol. Clinical studies employing isoproterenol challenge and exercise testing after single doses of propafenone indicate a beta-adrenergic blocking potency (per mg) about 1/40 that of propranolol in man. In clinical trials with the immediate-release formulation, resting heart rate decreases of about 8% were noted at the higher end of the therapeutic plasma concentration range. At very high concentrations in vitro, propafenone can inhibit the slow inward current carried by calcium, but this calcium antagonist effect probably does not contribute to antiarrhythmic efficacy. Moreover, propafenone inhibits a variety of cardiac potassium currents in in vitro studies (i.e., the transient outward, the delayed rectifier, and the inward rectifier current). Propafenone has local anesthetic activity approximately equal to procaine. Compared with propafenone, the main metabolite, 5-hydroxypropafenone, has similar sodium and calcium channel activity, but about 10 times less beta-blocking activity. (N-depropylpropafenone has weaker sodium channel activity but equivalent affinity for beta-receptors.)
12.2. Pharmacodynamics
Cardiac Electrophysiology
Electrophysiology trials in patients with ventricular tachycardia have shown that propafenone prolongs atrioventricular conduction while having little or no effect on sinus node function. Both atrioventricular nodal conduction time (AH interval) and His-Purkinje conduction time (HV interval) are prolonged. Propafenone has little or no effect on the atrial functional refractory period, but AV nodal functional and effective refractory periods are prolonged. In patients with Wolff-Parkinson-White syndrome, RYTHMOL immediate-release tablets reduce conduction and increase the effective refractory period of the accessory pathway in both directions.
Electrocardiograms: Propafenone prolongs the PR and QRS intervals. Prolongation of the QRS interval makes it difficult to interpret the effect of propafenone on the QT interval.
Table 1. Mean Change ± SD in 12-Lead Electrocardiogram Results (RAFT):
| RYTHMOL SR Twice-Daily Dosing | Placebo | |||
|---|---|---|---|---|
| 225 mg | 325 mg | 425 mg | ||
| n=126 | n=135 | n=136 | n=126 | |
| PR (ms) | 9 ± 22 | 12 ± 23 | 21 ± 24 | 1 ± 16 |
| QRS (ms) | 4 ± 14 | 6 ± 15 | 6 ± 15 | -2 ± 12 |
| Heart rate | 5 ± 24 | 7 ± 23 | 2 ± 22 | 8 ± 27 |
| QTca (ms) | 2 ± 30 | 5 ± 36 | 6 ± 37 | 5 ± 35 |
a Calculated using Bazett’s correction factor
In RAFT [see Clinical Studies (14)], the distribution of the maximum changes in QTc compared with baseline over the trial in each patient was similar in the groups receiving RYTHMOL SR 225 mg twice daily, 325 mg twice daily, and 425 mg twice daily, and placebo. Similar results were seen in the ERAFT trial.
Table 2. Number of Patients According to the Range of Maximum QTc Change Compared with Baseline over the Trial in Each Dose Group (RAFT Trial):
| Range Maximum QTc Change | RYTHMOL SR | Placebo N=100 n (%) | ||
|---|---|---|---|---|
| 225 mg Twice Daily | 325 mg Twice Daily | 425 mg Twice Daily | ||
| N=119 | N=129 | N=123 | ||
| n (%) | n (%) | n (%) | ||
| >20% | 1 (1) | 6 (5) | 3 (2) | 5 (4) |
| 10-20% | 19 (16) | 28 (22) | 32 (26) | 24 (20) |
| 0 ≤10% | 99 (83) | 95 (74) | 88 (72) | 91 (76) |
Hemodynamics
Trials in humans have shown that propafenone exerts a negative inotropic effect on the myocardium. Cardiac catheterization trials in patients with moderately impaired ventricular function (mean CI: 2.61 L/min/m²) utilizing intravenous propafenone infusions (loading dose of 2 mg/kg over 10 min + followed by 2 mg/min for 30 min) that gave mean plasma concentrations of 3.0 mcg/mL (a dose that produces plasma levels of propafenone greater than recommended oral dosing) showed significant increases in pulmonary capillary wedge pressure, systemic and pulmonary vascular resistances, and depression of cardiac output and cardiac index.
12.3. Pharmacokinetics
Absorption/Bioavailability
Maximal plasma levels of propafenone are reached between 3 to 8 hours following the administration of RYTHMOL SR. Propafenone is known to undergo extensive and saturable presystemic biotransformation which results in a dose-dependent and dosage-form-dependent absolute bioavailability; e.g., a 150-mg immediate-release tablet had an absolute bioavailability of 3.4%, while a 300-mg immediate-release tablet had an absolute bioavailability of 10.6%. Absorption from a 300-mg solution dose was rapid, with an absolute bioavailability of 21.4%. At still larger doses, above those recommended, bioavailability of propafenone from immediate-release tablets increased still further.
Relative bioavailability assessments have been performed between RYTHMOL SR capsules and RYTHMOL immediate-release tablets. In extensive metabolizers, the bioavailability of propafenone from the SR formulation was less than that of the immediate-release formulation as the more gradual release of propafenone from the prolonged-release preparations resulted in an increase of overall first-pass metabolism (see Metabolism). As a result of the increased first-pass effect, higher daily doses of propafenone were required from the SR formulation relative to the immediate-release formulation to obtain similar exposure to propafenone. The relative bioavailability of propafenone from the 325-mg twice-daily regimens of RYTHMOL SR approximates that of RYTHMOL immediate-release 150-mg 3-times-daily regimen. Mean exposure to 5-hydroxypropafenone was about 20% to 25% higher after SR capsule administration than after immediate-release tablet administration.
Food increased the exposure to propafenone 4-fold after single-dose administration of 425 mg of RYTHMOL SR. However, in the multiple-dose trial (425-mg dose twice daily), the difference between the fed and fasted state was not significant.
Distribution
Following intravenous administration of propafenone, plasma levels decline in a bi-phasic manner consistent with a 2-compartment pharmacokinetic model. The average distribution half-life corresponding to the first phase was about 5 minutes. The volume of the central compartment was about 88 liters (1.1 L/kg) and the total volume of distribution about 252 liters.
In serum, propafenone is greater than 95% bound to proteins within the concentration range of 0.5 to 2 mcg/mL.
Metabolism
There are 2 genetically determined patterns of propafenone metabolism. In over 90% of patients, the drug is rapidly and extensively metabolized with an elimination half-life from 2 to 10 hours. These patients metabolize propafenone into 2 active metabolites: 5-hydroxypropafenone, which is formed by CYP2D6, and N-depropylpropafenone (norpropafenone), which is formed by both CYP3A4 and CYP1A2.
In less than 10% of patients, metabolism of propafenone is slower because the 5-hydroxy metabolite is not formed or is minimally formed. In these patients, the estimated propafenone elimination half-life ranges from 10 to 32 hours. Decreased ability to form the 5-hydroxy metabolite of propafenone is associated with a diminished ability to metabolize debrisoquine and a variety of other drugs, such as encainide, metoprolol, and dextromethorphan, whose metabolism is mediated by the CYP2D6 isozyme. In these patients, the N-depropylpropafenone metabolite occurs in quantities comparable to the levels occurring in extensive metabolizers.
As a consequence of the observed differences in metabolism, administration of RYTHMOL SR to slow and extensive metabolizers results in significant differences in plasma concentrations of propafenone, with slow metabolizers achieving concentrations about twice those of the extensive metabolizers at daily doses of 850 mg/day. At low doses the differences are greater, with slow metabolizers attaining concentrations about 3 to 4 times higher than extensive metabolizers. In extensive metabolizers, saturation of the hydroxylation pathway (CYP2D6) results in greater-than-linear increases in plasma levels following administration of RYTHMOL SR capsules. In slow metabolizers, propafenone pharmacokinetics is linear. Because the difference decreases at high doses and is mitigated by the lack of the active 5-hydroxymetabolite in the slow metabolizers, and because steady-state conditions are achieved after 4 to 5 days of dosing in all patients, the recommended dosing regimen of RYTHMOL SR is the same for all patients. The larger inter-subject variability in blood levels requires that the dose of the drug be titrated carefully in patients with close attention paid to clinical and ECG evidence of toxicity [see Dosage and Administration (2)].
The 5-hydroxypropafenone and norpropafenone metabolites have electrophysiologic properties similar to propafenone in vitro. In man after administration of RYTHMOL SR, the 5-hydroxypropafenone metabolite is usually present in concentrations less than 40% of propafenone. The norpropafenone metabolite is usually present in concentrations less than 10% of propafenone.
Inter-Subject Variability
With propafenone, there is a considerable degree of inter-subject variability in pharmacokinetics which is due in large part to the first-pass hepatic effect and non-linear pharmacokinetics in extensive metabolizers. A higher degree of inter-subject variability in pharmacokinetic parameters of propafenone was observed following both single- and multiple-dose administration of RYTHMOL SR capsules. Inter-subject variability appears to be substantially less in the poor-metabolizer group than in the extensive-metabolizer group, suggesting that a large portion of the variability is intrinsic to CYP2D6 polymorphism rather than to the formulation.
Stereochemistry
RYTHMOL is a racemic mixture. The R- and S-enantiomers of propafenone display stereoselective disposition characteristics. In vitro and in vivo studies have shown that the R-isomer of propafenone is cleared faster than the S-isomer via the 5-hydroxylation pathway (CYP2D6). This results in a higher ratio of S-propafenone to R-propafenone at steady state. Both enantiomers have equivalent potency to block sodium channels; however, the S-enantiomer is a more potent beta-antagonist than the R-enantiomer. Following administration of RYTHMOL immediate-release tablets or RYTHMOL SR capsules, the S/R ratio for the area under the plasma concentration-time curve was about 1.7. The S/R ratios of propafenone obtained after administration of 225-mg, 325-mg, and 425-mg RYTHMOL SR are independent of dose. In addition, no difference in the average values of the S/R ratios is evident between genotypes or over time.
Specific Populations
Patients with Hepatic Impairment
Decreased liver function increases the bioavailability of propafenone. Absolute bioavailability assessments have not been determined for the capsule formulation of RYTHMOL SR. Absolute bioavailability of RYTHMOL immediate-release tablets is inversely related to indocyanine green clearance, reaching 60% to 70% at clearances of 7 mL/min and below. Protein binding decreases to about 88% in patients with severe hepatic dysfunction. The clearance of propafenone is reduced and the elimination half-life increased in patients with significant hepatic dysfunction [see Warnings and Precautions (5.9)].
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Lifetime maximally tolerated oral dose studies in mice (up to 360 mg/kg/day, approximately twice the MRHD on a mg/m² basis) and rats (up to 270 mg/kg/day, approximately 3 times the MRHD on a mg/m² basis) provided no evidence of a carcinogenic potential for propafenone.
Propafenone was not mutagenic in the Ames (salmonella) test and the in vivo mouse dominant lethal test. Propafenone was not clastogenic in the human lymphocyte chromosome aberration assay in vitro, the rat and Chinese hamster micronucleus tests, and other in vivo tests for chromosomal aberrations in rat bone marrow and Chinese hamster bone marrow and spermatogonia.
Propafenone, administered intravenously, has been shown to decrease spermatogenesis at lethal doses in rabbits (≥3.5 mg/kg/day) or at near-lethal dose levels in monkeys and dogs (≤5 mg/kg/day); doses were less than the MRHD on a mg/m² basis. These effects were reversible and did not impair fertility in rabbits at an intravenous dose of 3.5 mg/kg/day (a spermatogenesis-impairing dose). Effects on spermatogenesis were not found when propafenone was administered to rats either orally or intravenously up to 360 mg/kg/day or 6 mg/kg/day, respectively, or in dogs at oral doses up to 240 mg/kg/day (up to approximately 4 or 9 times the MRHD on a mg/m² basis in rats and dogs, respectively). Treatment of male rabbits for 10 weeks prior to mating at an oral dose of 120 mg/kg/day (approximately 2 times the MRHD on a mg/m² basis) did not result in evidence of impaired fertility. Nor was there evidence of impaired fertility when propafenone was administered orally to male and female rats at dose levels up to 270 mg/kg/day (approximately 3 times the MRHD on a mg/m² basis) for 10 weeks (males) or 2 weeks (females) prior to mating through mating.
13.2. Animal Toxicology and/or Pharmacology
Renal changes have been observed in the rat following 6 months of oral administration of propafenone HCl at doses of 180 and 360 mg/kg/day (about 2 and 4 times, respectively, the MRHD on a mg/m² basis). Both inflammatory and non-inflammatory changes in the renal tubules, with accompanying interstitial nephritis, were observed. These changes were reversible, as they were not found in rats allowed to recover for 6 weeks. Fatty degenerative changes of the liver were found in rats following longer durations of administration of propafenone HCl at a dose of 270 mg/kg/day (about 3 times the MRHD on a mg/m² basis). There were no renal or hepatic changes at 90 mg/kg/day equivalent to the MRHD on a mg/m² basis).
14. Clinical Studies
RYTHMOL SR has been evaluated in patients with a history of electrocardiographically documented recurrent episodes of symptomatic AF in 2 randomized, double-blind, placebo-controlled trials.
RAFT
In one U.S. multicenter trial (RAFT), 3 doses of RYTHMOL SR (225 mg twice daily, 325 mg twice daily, and 425 mg twice daily) and placebo were compared in 523 patients with symptomatic, episodic AF. The patient population in this trial was 59% male with a mean age of 63 years, 91% white, and 6% black. The patients had a median history of AF of 13 months and documented symptomatic AF within 12 months of trial entry. Over 90% were NYHA Class I, and 21% had a prior electrical cardioversion. At baseline, 24% were treated with calcium channel blockers, 37% with beta-blockers, and 38% with digoxin. Symptomatic arrhythmias after randomization were documented by transtelephonic electrocardiogram and centrally read and adjudicated by a blinded adverse event committee. RYTHMOL SR administered for up to 39 weeks was shown to prolong significantly the time to the first recurrence of symptomatic atrial arrhythmia, predominantly AF, from Day 1 of randomization (primary efficacy variable) compared with placebo, as shown in Table 3.
Table 3. Analysis of Tachycardia-Free Period (Days) from Day 1 of Randomization:
| Parameter | Dose of RYTHMOL SR | |||
|---|---|---|---|---|
| 225 mg Twice Daily (N=126) n (%) | 325 mg Twice Daily (N=135) n (%) | 425 mg Twice Daily (N=136) n (%) | Placebo (N=126) n (%) | |
| Patients completing with terminating eventa | 66 (52) | 56 (41) | 41 (30) | 87 (69) |
| Comparison of tachycardia-free periods | ||||
| Kaplan-Meier Media | 112 | 291 | NAb | 41 |
| Range | 0-285 | 0-293 | 0-300 | 0-289 |
| P-Value (Log-rank test) | 0.014 | <0.0001 | <0.0001 | -- |
| Hazard Ratio compared with placebo | 0.67 | 0.43 | 0.35 | -- |
| 95% CI for Hazard Ratio | (0.49, 0.93) | (0.31, 0.61) | (0.24, 0.51) | -- |
a Terminating events comprised 91% AF, 5% atrial flutter, and 4% PSVT.
b Not Applicable: Fewer than 50% of the patients had events. The median time is not calculable.
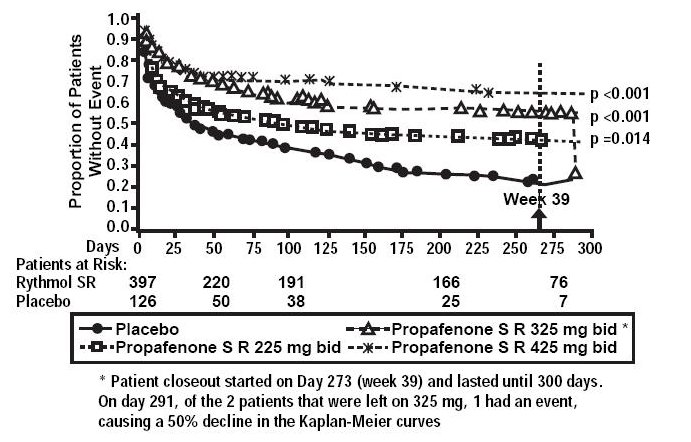
There was a dose response for RYTHMOL SR for the tachycardia-free period as shown in the proportional hazard analysis and the Kaplan-Meier curves presented in Figure 1.
Figure 1. RAFT Kaplan-Meier Analysis for the Tachycardia-Free Period from Day 1 of Randomization:
In additional analyses, RYTHMOL SR (225 mg twice daily, 325 mg twice daily, and 425 mg twice daily) was also shown to prolong time to the first recurrence of symptomatic AF from Day 5 (steady-state pharmacokinetics were attained). The antiarrhythmic effect of RYTHMOL SR was not influenced by age, gender, history of cardioversion, duration of AF, frequency of AF, or use of medication that lowers heart rate. Similarly, the antiarrhythmic effect of RYTHMOL SR was not influenced by the individual use of calcium channel blockers, beta-blockers, or digoxin. Too few non-white patients were enrolled to assess the influence of race on effects of RYTHMOL SR.
No difference in the average heart rate during the first recurrence of symptomatic arrhythmia between RYTHMOL SR and placebo was observed.
ERAFT
In a European multicenter trial (European Rythmonorm SR Atrial Fibrillation Trial [ERAFT]), 2 doses of RYTHMOL SR (325 mg twice daily and 425 mg twice daily) and placebo were compared in 293 patients with documented electrocardiographic evidence of symptomatic paroxysmal AF. The patient population in this trial was 61% male, 100% white with a mean age of 61 years. Patients had a median duration of AF of 3.3 years, and 61% were taking medications that lowered heart rate. At baseline, 15% of the patients were treated with calcium channel blockers (verapamil and diltiazem), 42% with beta-blockers, and 8% with digoxin. During a qualifying period of up to 28 days, patients had to have 1 ECG-documented incident of symptomatic AF. The double-blind treatment phase consisted of a 4-day loading period followed by a 91-day efficacy period. Symptomatic arrhythmias were documented by electrocardiogram monitoring.
In ERAFT, RYTHMOL SR was shown to prolong the time to the first recurrence of symptomatic atrial arrhythmia from Day 5 of randomization (primary efficacy analysis). The proportional hazard analysis revealed that both doses of RYTHMOL SR were superior to placebo. The antiarrhythmic effect of propafenone SR was not influenced by age, gender, duration of AF, frequency of AF, or use of medication that lowers heart rate. It was also not influenced by the individual use of calcium channel blockers, beta-blockers, or digoxin. Too few non-white patients were enrolled to assess the influence of race on the effects of RYTHMOL SR. There was a slight increase in the incidence of centrally diagnosed asymptomatic AF or atrial flutter in each of the 2 treatment groups receiving RYTHMOL SR compared with placebo.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.