XIGDUO Film-coated tablet Ref.[50780] Active ingredients: Dapagliflozin Metformin Metformin and Dapagliflozin
Source: European Medicines Agency (EU) Revision Year: 2023 Publisher: AstraZeneca AB, SE-151 85 Södertälje, Sweden
5.1. Pharmacodynamic properties
Pharmacotherapeutic group: Drugs used in diabetes, Combinations of oral blood glucose-lowering drugs
ATC code: A10BD15
Mechanism of action
Xigduo combines two anti-hyperglycaemic medicinal products with different and complementary mechanisms of action to improve glycaemic control in patients with type 2 diabetes: dapagliflozin, a SGLT2 inhibitor, and metformin hydrochloride, a member of the biguanide class.
Dapagliflozin
Dapagliflozin is a highly potent (Ki: 0.55 nM), selective and reversible inhibitor of SGLT2.
Inhibition of SGLT2 by dapagliflozin reduces reabsorption of glucose from the glomerular filtrate in the proximal renal tubule with a concomitant reduction in sodium reabsorption leading to urinary excretion of glucose and osmotic diuresis. Dapagliflozin therefore increases the delivery of sodium to the distal tubule which increases tubuloglomerular feedback and reduces intraglomerular pressure. This combined with osmotic diuresis leads to a reduction in volume overload, reduced blood pressure, and lower preload and afterload, which may have beneficial effects on cardiac remodelling and preserve renal function. Other effects include an increase in haematocrit and reduction in body weight. The cardiac and renal benefits of dapagliflozin are not solely dependent on the blood glucose-lowering
effect.
Dapagliflozin improves both fasting and post-prandial plasma glucose levels by reducing renal glucose reabsorption leading to urinary glucose excretion. This glucose excretion (glucuretic effect) is observed after the first dose, is continuous over the 24-hour dosing interval and is sustained for the duration of treatment. The amount of glucose removed by the kidney through this mechanism is dependent upon the blood glucose concentration and GFR. Thus, in subjects with normal blood glucose, dapagliflozin has a low propensity to cause hypoglycaemia. Dapagliflozin does not impair normal endogenous glucose production in response to hypoglycaemia. Dapagliflozin acts independently of insulin secretion and insulin action. Improvement in homeostasis model assessment for beta cell function (HOMA beta-cell) has been observed in clinical studies with dapagliflozin.
The SGLT2 is selectively expressed in the kidney. Dapagliflozin does not inhibit other glucose transporters important for glucose transport into peripheral tissues and is >1,400 times more selective for SGLT2 versus SGLT1, the major transporter in the gut responsible for glucose absorption.
Metformin
Metformin is a biguanide with anti-hyperglycaemic effects, lowering both basal and postprandial plasma glucose. It does not stimulate insulin secretion and therefore does not produce hypoglycaemia.
Metformin may act via three mechanisms:
- by reduction of hepatic glucose production by inhibiting gluconeogenesis and glycogenolysis;
- by modestly increasing insulin sensitivity, improving peripheral glucose uptake and utilisation in muscle;
- by delaying intestinal glucose absorption.
Metformin stimulates intracellular glycogen synthesis by acting on glycogen synthase. Metformin increases the transport capacity of specific types of membrane glucose transporters (GLUT-1 and GLUT-4).
Pharmacodynamic effects
Dapagliflozin
Increases in the amount of glucose excreted in the urine were observed in healthy subjects and in subjects with type 2 diabetes mellitus following the administration of dapagliflozin. Approximately 70 g of glucose was excreted in the urine per day (corresponding to 280 kcal/day) at a dapagliflozin dose of 10 mg/day in subjects with type 2 diabetes mellitus for 12 weeks. Evidence of sustained glucose excretion was seen in subjects with type 2 diabetes mellitus given dapagliflozin 10 mg/day for up to 2 years.
This urinary glucose excretion with dapagliflozin also results in osmotic diuresis and increases in urinary volume in subjects with type 2 diabetes mellitus. Urinary volume increases in subjects with type 2 diabetes mellitus treated with dapagliflozin 10 mg were sustained at 12 weeks and amounted to approximately 375 mL/day. The increase in urinary volume was associated with a small and transient increase in urinary sodium excretion that was not associated with changes in serum sodium concentrations.
Urinary uric acid excretion was also increased transiently (for 3-7 days) and accompanied by a sustained reduction in serum uric acid concentration. At 24 weeks, reductions in serum uric acid concentrations ranged from -48.3 to -18.3 micromoles/L (-0.87 to -0.33 mg/dL).
The pharmacodynamics of 5 mg dapagliflozin twice daily and 10 mg dapagliflozin once daily were compared in healthy subjects. The steady-state inhibition of renal glucose reabsorption and the amount of urinary glucose excretion over a 24-hour period was the same for both dosing regimens.
Metformin
In humans, independently of its action on glycaemia, metformin has favourable effects on lipid metabolism. This has been shown at therapeutic doses in controlled, medium-term or long-term clinical studies: metformin reduces total cholesterol, LDL cholesterol and triglyceride levels.
In clinical studies, use of metformin was associated with either a stable body weight or modest weight loss.
Clinical efficacy and safety
Both improvement of glycaemic control and reduction of cardiovascular morbidity and mortality are an integral part of the treatment of type 2 diabetes.
The coadministration of dapagliflozin and metformin has been studied in subjects, with type 2 diabetes, inadequately controlled on diet and exercise alone, and in subjects inadequately controlled on metformin alone or in combination with a DPP-4 inhibitor (sitagliptin), sulphonylurea or insulin.
Treatment with dapagliflozin plus metformin at all doses produced clinically relevant and statistically significant improvements in HbA1c and fasting plasma glucose (FPG) compared with control. Clinically relevant glycaemic effects were sustained in long-term extensions up to 104 weeks. HbA1c reductions were seen across subgroups including gender, age, race, duration of disease, and baseline body mass index (BMI). Additionally, at Week 24, clinically relevant and statistically significant improvements in mean changes from baseline in body weight were seen with dapagliflozin and metformin combination treatments compared with control. Body weight reductions were sustained in long-term extensions up to 208 weeks. Additionally, dapagliflozin twice-daily treatment added to metformin was shown to be effective and safe in type 2 diabetic subjects. Furthermore, two 12-week, placebo-controlled studies were conducted in patients with inadequately controlled type 2 diabetes and hypertension.
In a cardiovascular outcomes study (DECLARE), dapagliflozin as adjunct to standard care therapy reduced cardiovascular and renal events in patients with type 2 diabetes.
Glycaemic control
Add-on combination therapy
In a 52-week, active-controlled non-inferiority study (with 52- and 104-week extension periods), dapagliflozin 10 mg was evaluated as add-on therapy to metformin compared with a sulphonylurea (glipizide) as add-on therapy to metformin in subjects with inadequate glycaemic control (HbA1c >6.5% and ≤10%). The results showed a similar mean reduction in HbA1c from baseline to Week 52, compared with glipizide, thus demonstrating non-inferiority (Table 3). At Week 104, adjusted mean change from baseline in HbA1c was -0.32% for dapagliflozin and -0.14% for glipizide, respectively. At Week 208, adjusted mean change from baseline in HbA1c was -0.10% for dapagliflozin and 0.20% for glipizide, respectively. At 52, 104 and 208 weeks, a significantly lower proportion of subjects in the group treated with dapagliflozin (3.5%, 4.3% and 5.0%, respectively) experienced at least one event of hypoglycaemia compared with the group treated with glipizide (40.8%, 47% and 50.0%, respectively). The proportion of subjects remaining in the study at Week 104 and Week 208 was 56.2% and 39.7% for the group treated with dapagliflozin and 50.0% and 34.6% for the group treated with glipizide.
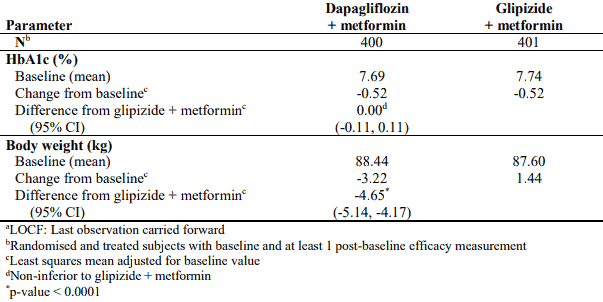
Table 3. Results at Week 52 (LOCFa) in an active-controlled study comparing dapagliflozin with glipizide as add-on to metformin:
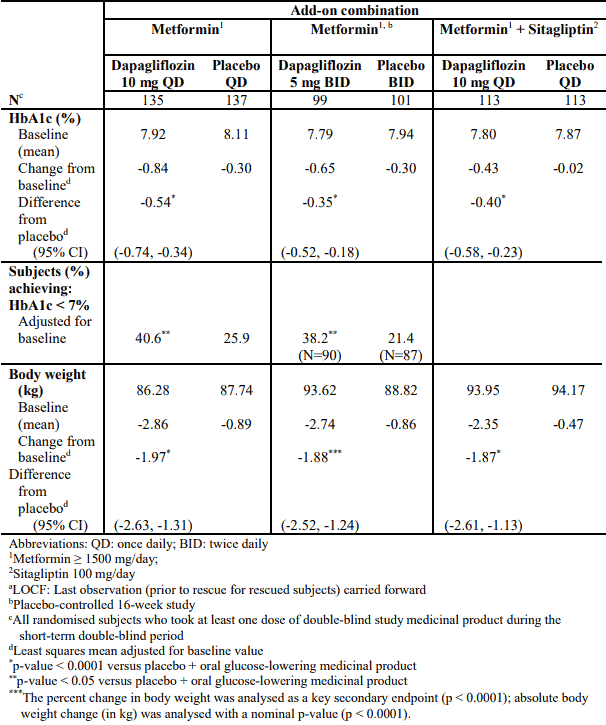
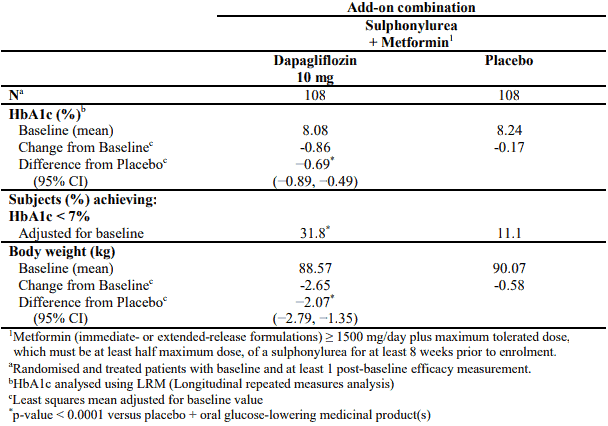
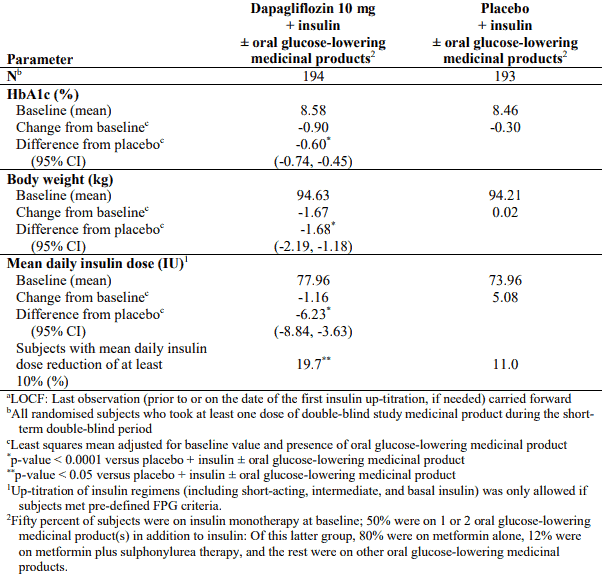
Dapagliflozin as an add-on with either metformin alone, metformin in combination with sitagliptin, sulphonylurea or insulin (with or without additional oral glucose-lowering medicinal products, including metformin) resulted in statistically significant mean reductions in HbA1c at 24 weeks compared with subjects receiving placebo (p <0.0001; Tables 4, 5 and 6). Dapagliflozin 5 mg twice daily provided statistically significant reductions in HbA1c at 16 weeks compared with subjects receiving placebo (p <0.0001; Table 4).
The reductions in HbA1c observed at Week 24 were sustained in the add-on combination studies. For the add-on to metformin study, HbA1c reductions were sustained through Week 102 (-0.78% and 0.02% adjusted mean change from baseline for dapagliflozin 10 mg and placebo, respectively). At Week 48 for metformin plus sitagliptin, the adjusted mean change from baseline for dapagliflozin 10 mg and placebo was -0.44% and 0.15%, respectively. At Week 104 for insulin (with or without additional oral glucose-lowering medicinal products, including metformin), the HbA1c reductions were -0.71% and -0.06% adjusted mean change from baseline for dapagliflozin 10 mg and placebo, respectively. At Weeks 48 and 104, the insulin dose remained stable compared to baseline in subjects treated with dapagliflozin 10 mg at an average dose of 76 IU/day. In the placebo group there was an increase of 10.5 IU/day and 18.3 IU/day from baseline (mean average dose of 84 and 92 IU/day) at Weeks 48 and 104, respectively. The proportion of subjects remaining in the study at Week 104 was 72.4% for the group treated with dapagliflozin 10 mg and 54.8% for the placebo group.
In a separate analysis of subjects on insulin plus metformin, similar reductions in HbA1c to those seen in the total study population were seen in subjects treated with dapagliflozin with insulin plus metformin. At Weeks 24, HbA1c change from baseline in subjects treated with dapagliflozin plus insulin with metformin was -0.93%.
Table 4. Results of (LOCFa) placebo-controlled studies up to 24 weeks of dapagliflozin in add-on combination with metformin or metformin plus sitagliptin:
Table 5. Results of a 24-week placebo-controlled study of dapagliflozin in add-on combination with metformin and a sulphonylurea:
Table 6. Results at Week 24 (LOCFa) in a placebo-controlled study of dapagliflozin in combination with insulin (alone or with oral glucose-lowering medicinal products, including metformin):
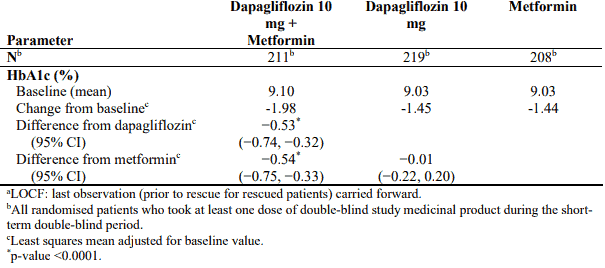
In combination with metformin in drug-naive patients
A total of 1,236 drug-naive patients with inadequately controlled type 2 diabetes (HbA1c ≥7.5% and ≤12%) participated in two active-controlled studies of 24 weeks duration to evaluate the efficacy and safety of dapagliflozin (5 mg or 10 mg) in combination with metformin in drug-naive patients versus therapy with the monocomponents.
Treatment with dapagliflozin 10 mg in combination with metformin (up to 2,000 mg per day) provided significant improvements in HbA1c compared to the individual components (Table 7), and led to greater reductions in FPG (compared to the individual components) and body weight (compared to metformin).
Table 7. Results at Week 24 (LOCFa) in an active-controlled study of dapagliflozin and metformin combination therapy in drug-naive patients:
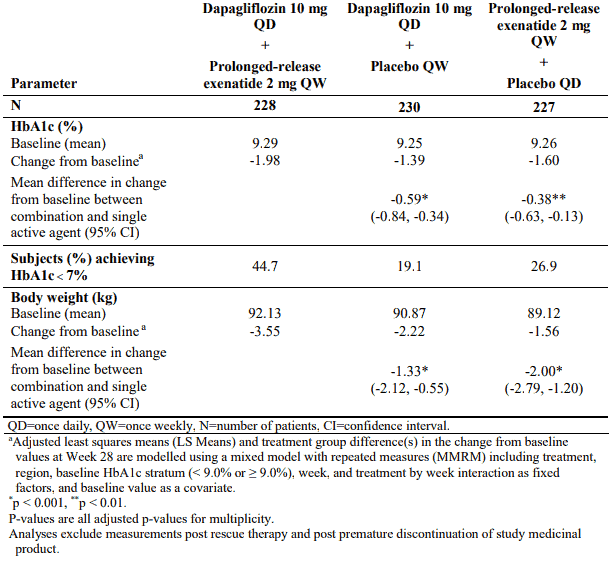
Combination therapy with prolonged-release exenatide
In a 28-week, double-blind, active comparator-controlled study, the combination of dapagliflozin and prolonged-release exenatide (a GLP-1 receptor agonist) was compared to dapagliflozin alone and prolonged-release exenatide alone in subjects with inadequate glycaemic control on metformin alone (HbA1c ≥8% and ≤12%). All treatment groups had a reduction in HbA1c compared to baseline. The combination treatment with dapagliflozin 10 mg and prolonged-release exenatide group showed superior reductions in HbA1c from baseline compared to dapagliflozin alone and prolonged-release exenatide alone (Table 8).
Table 8. Results of one 28-week trial of dapagliflozin and prolonged-release exenatide versus dapagliflozin alone and prolonged-release exenatide alone, in combination with metformin (intent to treat patients):
Fasting plasma glucose
Treatment with dapagliflozin as an add-on to either metformin alone (dapagliflozin 10 mg QD or dapagliflozin 5 mg BID) or metformin plus sitagliptin, sulphonylurea or insulin resulted in statistically significant reductions in FPG (-1.90 to -1.20 mmol/L [-34.2 to -21.7 mg/dL]) compared with placebo (-0.58 to 0.18 mmol/L [-10.4 to 3.3 mg/dL]) at Week 16 (5 mg BID) or Week 24. This effect was observed at Week 1 of treatment and maintained in studies extended through Week 104.
Combination therapy of dapagliflozin 10 mg and prolonged-release exenatide resulted in significantly greater reductions in FPG at Week 28: -3.66 mmol/L (-65.8 mg/dL), compared to -2.73 mmol/L (-49.2 mg/dL) for dapagliflozin alone (p <0.001) and -2.54 mmol/L (-45.8 mg/dL) for exenatide alone (p <0.001).
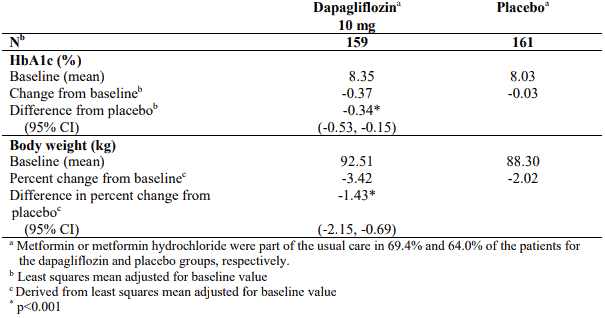
In a dedicated study in diabetic patients with an eGFR ≥45 to <60 mL/min/1.73 m², treatment with dapagliflozin demonstrated reductions in FPG at Week 24: -1.19 mmol/L (-21.46 mg/dL) compared to -0.27 mmol/L (-4.87 mg/dL) for placebo (p=0.001).
Post-prandial glucose
Treatment with dapagliflozin 10 mg as an add-on to sitagliptin plus metformin resulted in reductions in 2-hour post-prandial glucose at 24 weeks that were maintained up to Week 48.
Combination therapy of dapagliflozin 10 mg and prolonged-release exenatide resulted in significantly greater reductions in 2-hour post-prandial glucose at Week 28 compared to either agent alone.
Body weight
Dapagliflozin as an add-on to metformin alone or metformin plus sitagliptin, sulphonylurea or insulin (with or without additional oral glucose-lowering medicinal products, including metformin) resulted in statistically significant body weight reduction up to 24 weeks (p <0.0001, Tables 4, 5 and 6). These effects were sustained in longer-term trials. At 48 weeks, the difference for dapagliflozin as add-on to metformin plus sitagliptin compared with placebo was -2.07 kg. At 102 weeks, the difference for dapagliflozin as add-on to metformin compared with placebo or as add-on to insulin compared with placebo was -2.14 and -2.88 kg, respectively.
As an add-on therapy to metformin in an active-controlled non-inferiority study, dapagliflozin resulted in a statistically significant body weight change compared with glipizide of -4.65 kg at 52 weeks (p <0.0001, Table 3) that was sustained at 104 and 208 weeks (-5.06 kg and -4.38 kg, respectively).
The combination of dapagliflozin 10 mg and prolonged-release exenatide demonstrated significantly greater weight reductions compared to either agent alone (Table 8).
A 24-week study in 182 diabetic subjects using dual energy X-ray absorptiometry (DXA) to evaluate body composition demonstrated reductions with dapagliflozin 10 mg plus metformin compared with placebo plus metformin, respectively, in body weight and body fat mass as measured by DXA rather than lean tissue or fluid loss. Treatment with dapagliflozin 10 mg plus metformin showed a numerical decrease in visceral adipose tissue compared with placebo plus metformin treatment in a magnetic resonance imaging substudy.
Blood pressure
In a pre-specified pooled analysis of 13 placebo-controlled studies, treatment with dapagliflozin 10 mg resulted in a systolic blood pressure change from baseline of –3.7 mmHg and diastolic blood pressure of –1.8 mmHg versus –0.5 mmHg systolic and -0.5 mmHg diastolic blood pressure for placebo group at Week 24. Similar reductions were observed at up to 104 weeks.
Combination therapy of dapagliflozin 10 mg and prolonged-release exenatide resulted in a significantly greater reduction in systolic blood pressure at Week 28 (-4.3 mmHg) compared to dapagliflozin alone (-1.8 mmHg, p <0.05) and prolonged-release exenatide alone (-1.2 mmHg, p <0.01).
In two 12-week, placebo-controlled studies a total of 1,062 patients with inadequately controlled type 2 diabetes and hypertension (despite pre-existing stable treatment with an ACE-I or ARB in one study and an ACE-I or ARB plus one additional antihypertensive treatment in another study) were treated with dapagliflozin 10 mg or placebo. At Week 12 for both studies, dapagliflozin 10 mg plus usual antidiabetic treatment provided improvement in HbA1c and decreased the placebo-corrected systolic blood pressure on average by 3.1 and 4.3 mmHg, respectively.
In a dedicated study in diabetic patients with an eGFR ≥45 to <60 mL/min/1.73 m², treatment with dapagliflozin demonstrated reductions in seated systolic blood pressure at Week 24: -4.8 mmHg compared to -1.7 mmHg for placebo (p <0.05).
Patients with baseline HbA1c ≥9%
In a pre-specified analysis of subjects with baseline HbA1c ≥ 9.0%, treatment with dapagliflozin 10 mg resulted in statistically significant reductions in HbA1c at Week 24 as an add-on to metformin (adjusted mean change from baseline: -1.32% and -0.53% for dapagliflozin and placebo, respectively).
Glycaemic control in patients with moderate renal impairment CKD 3A (eGFR ≥45 to <60 mL/min/1.73 m²)
The efficacy of dapagliflozin was assessed in a dedicated study in diabetic patients with an eGFR ≥45 to <60 mL/min/1.73 m² who had inadequate glycaemic control on usual care. Treatment with dapagliflozin resulted in reductions in HbA1c and body weight compared with placebo (Table 9).
Table 9. Results at Week 24 of a placebo-controlled study of dapagliflozin in diabetic patients with an eGFR ≥45 to <60 mL/min/1.73 m²:
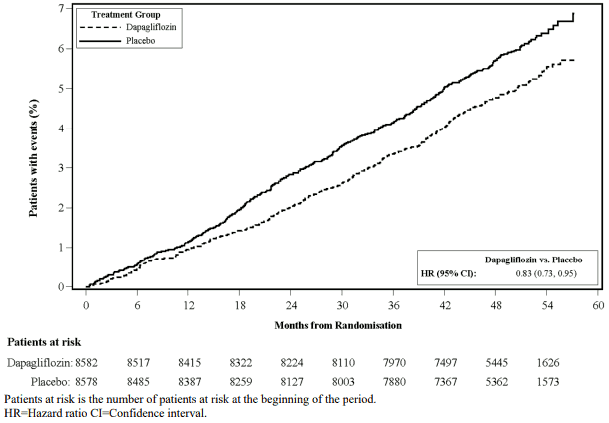
Cardiovascular and renal outcomes
Dapagliflozin Effect on Cardiovascular Events (DECLARE) was an international, multicentre, randomised, double-blind, placebo-controlled clinical study conducted to determine the effect of dapagliflozin compared with placebo on cardiovascular outcomes when added to current background therapy. All patients had type 2 diabetes mellitus and either at least two additional cardiovascular risk factors (age ≥55 years in men or ≥60 years in women and one or more of dyslipidaemia, hypertension or current tobacco use) or established cardiovascular disease.
Of 17,160 randomised patients, 6,974 (40.6%) had established cardiovascular disease and 10,186 (59.4%) did not have established cardiovascular disease. 8,582 patients were randomised to dapagliflozin 10 mg and 8,578 to placebo, and were followed for a median of 4.2 years.
The mean age of the study population was 63.9 years, 37.4% were female. In total, 22.4% had had diabetes for ≤5 years, mean duration of diabetes was 11.9 years. Mean HbA1c was 8.3% and mean BMI was 32.1 kg/m².
At baseline, 10.0% of patients had a history of heart failure. Mean eGFR was 85.2 mL/min/1.73 m², 7.4% of patients had eGFR <60 mL/min/1.73 m², and 30.3% of patients had micro- or macroalbuminuria (urine albumin to creatinine ratio [UACR] ≥30 to ≤300 mg/g or >300 mg/g, respectively).
Most patients (98%) used one or more diabetic medications at baseline, including metformin (82%), insulin (41%) and sulfonylurea (43%).
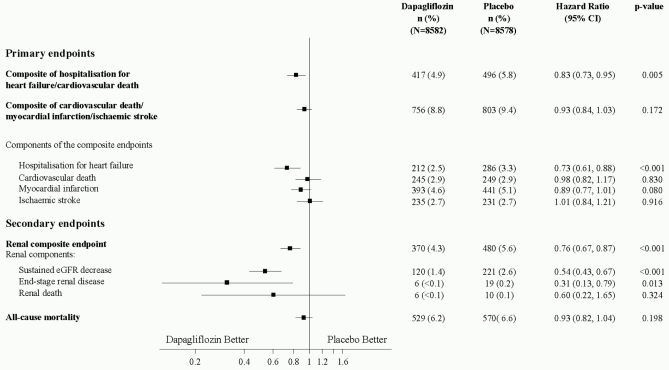
The primary endpoints were time to first event of the composite of cardiovascular death, myocardial infarction or ischaemic stroke (MACE) and time to first event of the composite of hospitalisation for heart failure or cardiovascular death. The secondary endpoints were a renal composite endpoint and all-cause mortality.
Major adverse cardiovascular events
Dapagliflozin 10 mg demonstrated non-inferiority versus placebo for the composite of cardiovascular death, myocardial infarction or ischaemic stroke (one-sided p <0.001).
Heart failure or cardiovascular death
Dapagliflozin 10 mg demonstrated superiority versus placebo in preventing the composite of hospitalisation for heart failure or cardiovascular death (Figure 1). The difference in treatment effect was driven by hospitalisation for heart failure, with no difference in cardiovascular death (Figure 2).
The treatment benefit of dapagliflozin over placebo was observed both in patients with and without established cardiovascular disease, with and without heart failure at baseline, and was consistent across key subgroups, including age, gender, renal function (eGFR) and region.
Figure 1. Time to first occurrence of hospitalisation for heart failure or cardiovascular death:
Results on primary and secondary endpoints are displayed in Figure 2. Superiority of dapagliflozin over placebo was not demonstrated for MACE (p= 0.172). The renal composite endpoint and all-cause mortality were therefore not tested as part of the confirmatory testing procedure.
Figure 2. Treatment effects for the primary composite endpoints and their components, and the secondary endpoints and components:
Renal composite endpoint defined as: sustained confirmed ≥40% decrease in eGFR to eGFR <60 mL/min/1.73 m² and/or end-stage renal disease (dialysis ≥90 days or kidney transplantation, sustained confirmed eGFR <15 mL/min/1.73 m²) and/or renal or cardiovascular death. p-values are two-sided. p-values for the secondary endpoints and for single components are nominal. Time to first event was analysed in a Cox proportional hazards model. The number of first events for the single components are the actual number of first events for each component and does not add up to the number of events in the composite endpoint.
CI = confidence interval.
Nephropathy
Dapagliflozin reduced the incidence of events of the composite of confirmed sustained eGFR decrease, end-stage renal disease, renal or cardiovascular death. The difference between groups was driven by reductions in events of the renal components; sustained eGFR decrease, end-stage renal disease and renal death (Figure 2).
The hazard ratio for time to nephropathy (sustained eGFR decrease, end-stage renal disease and renal death) was 0.53 (95% CI 0.43, 0.66) for dapagliflozin versus placebo.
In addition, dapagliflozin reduced the new onset of sustained albuminuria (hazard ratio 0.79 [95% CI 0.72, 0.87]) and led to greater regression of macroalbuminuria (hazard ratio 1.82 [95% CI 1.51, 2.20]) compared with placebo.
Metformin
The prospective randomised (UKPDS) study has established the long-term benefit of intensive blood glucose control in type 2 diabetes. Analysis of the results for overweight patients treated with metformin after failure of diet alone showed:
- a significant reduction of the absolute risk of any diabetes-related complication in the metformin group (29.8 events/1,000 patient-years) versus diet alone (43.3 events/1,000 patient-years), p=0.0023, and versus the combined sulphonylurea and insulin monotherapy groups (40.1 events/1,000 patient-years), p=0.0034;
- a significant reduction of the absolute risk of any diabetes-related mortality: metformin 7.5 events/1,000 patient-years, diet alone 12.7 events/1,000 patient-years, p=0.017;
- a significant reduction of the absolute risk of overall mortality: metformin 13.5 events/1,000 patient-years versus diet alone 20.6 events/1,000 patient-years, (p=0.011), and versus the combined sulphonylurea and insulin monotherapy groups 18.9 events/1,000 patient-years (p=0.021);
- a significant reduction in the absolute risk of myocardial infarction: metformin 11 events/1,000 patient-years, diet alone 18 events/1,000 patient-years, (p=0.01).
Paediatric population
The European Medicines Agency has waived the obligation to submit the results of studies with Xigduo in all subsets of the paediatric population in the treatment of type 2 diabetes (see section 4.2 for information on paediatric use).
5.2. Pharmacokinetic properties
Xigduo combination tablets are considered to be bioequivalent to coadministration of corresponding doses of dapagliflozin and metformin hydrochloride administered together as individual tablets.
The pharmacokinetics of 5 mg dapagliflozin twice daily and 10 mg dapagliflozin once daily were compared in healthy subjects. Administration of 5 mg dapagliflozin twice daily gave similar overall exposures (AUCss) over a 24-hour period as 10 mg dapagliflozin administered once daily. As expected, dapagliflozin 5 mg administered twice daily compared with 10 mg dapagliflozin once daily resulted in lower peak dapagliflozin plasma concentrations (Cmax) and higher trough plasma dapagliflozin concentrations (Cmin).
Interaction with food
The administration of this medicinal product in healthy volunteers after a high fat meal compared to after the fasted state resulted in the same extent of exposure for both dapagliflozin and metformin. The meal resulted in a delay of 1 to 2 hours in the peak concentrations and a decrease in the maximum plasma concentration of 29% of dapagliflozin and 17% of metformin. These changes are not considered to be clinically meaningful.
Paediatric population
Pharmacokinetics in the paediatric population have not been studied.
The following statements reflect the pharmacokinetic properties of the individual active substances of this medicinal product.
Dapagliflozin
Absorption
Dapagliflozin was rapidly and well absorbed after oral administration. Maximum dapagliflozin plasma concentrations (Cmax) were usually attained within 2 hours after administration in the fasted state. Geometric mean steady-state dapagliflozin Cmax and AUCτ values following once daily 10 mg doses of dapagliflozin were 158 ng/mL and 628 ng h/mL, respectively. The absolute oral bioavailability of dapagliflozin following the administration of a 10 mg dose is 78%.
Distribution
Dapagliflozin is approximately 91% protein bound. Protein binding was not altered in various disease states (e.g. renal or hepatic impairment). The mean steady-state volume of distribution of dapagliflozin was 118 liters.
Biotransformation
Dapagliflozin is extensively metabolised, primarily to yield dapagliflozin 3-O-glucuronide, which is an inactive metabolite. Dapagliflozin 3-O-glucuronide or other metabolites do not contribute to the glucose-lowering effects. The formation of dapagliflozin 3-O-glucuronide is mediated by UGT1A9, an enzyme present in the liver and kidney, and CYP-mediated metabolism was a minor clearance pathway in humans.
Elimination
The mean plasma terminal half-life (t½) for dapagliflozin was 12.9 hours following a single oral dose of dapagliflozin 10 mg to healthy subjects. The mean total systemic clearance of dapagliflozin administered intravenously was 207 mL/min. Dapagliflozin and related metabolites are primarily eliminated via urinary excretion with less than 2% as unchanged dapagliflozin. After administration of a 50 mg [14C]-dapagliflozin dose, 96% was recovered, 75% in urine and 21% in faeces. In faeces, approximately 15% of the dose was excreted as parent drug.
Linearity
Dapagliflozin exposure increased proportional to the increment in dapagliflozin dose over the range of 0.1 to 500 mg and its pharmacokinetics did not change with time upon repeated daily dosing for up to 24 weeks.
Special populations
Renal impairment
At steady-state (20 mg once-daily dapagliflozin for 7 days), subjects with type 2 diabetes mellitus and mild, moderate or severe renal impairment (as determined by iohexol plasma clearance) had mean systemic exposures of dapagliflozin of 32%, 60% and 87% higher, respectively, than those of subjects with type 2 diabetes mellitus and normal renal function. The steady-state 24-hour urinary glucose excretion was highly dependent on renal function and 85, 52, 18 and 11 g of glucose/day was excreted by subjects with type 2 diabetes mellitus and normal renal function or mild, moderate or severe renal impairment, respectively. The impact of haemodialysis on dapagliflozin exposure is not known.
Hepatic impairment
In subjects with mild or moderate hepatic impairment (Child-Pugh classes A and B), mean Cmax and AUC of dapagliflozin were up to 12% and 36% higher, respectively, compared with healthy matched control subjects. These differences were not considered to be clinically meaningful. In subjects with severe hepatic impairment (Child-Pugh class C) mean Cmax and AUC of dapagliflozin were 40% and 67% higher than matched healthy controls, respectively.
Elderly (≥65 years)
There is no clinically meaningful increase in exposure based on age alone in subjects up to 70 years old. However, an increased exposure due to age-related decrease in renal function can be expected. There are insufficient data to draw conclusions regarding exposure in patients >70 years old.
Gender
The mean dapagliflozin AUCss in females was estimated to be about 22% higher than in males.
Race
There were no clinically relevant differences in systemic exposures between White, Black or Asian races.
Body weight
Dapagliflozin exposure was found to decrease with increased weight. Consequently, low-weight patients may have somewhat increased exposure and patients with high weight somewhat decreased exposure. However, the differences in exposure were not considered clinically meaningful.
Paediatric population
Pharmacokinetics in the paediatric population have not been studied.
Metformin
Absorption
After an oral dose of metformin, tmax is reached in 2.5 h. Absolute bioavailability of a 500 mg or 850 mg metformin tablet is approximately 50-60% in healthy subjects. After an oral dose, the non-absorbed fraction recovered in faeces was 20-30%.
After oral administration, metformin absorption is saturable and incomplete. It is assumed that the pharmacokinetics of metformin absorption is non-linear. At the usual metformin doses and dosing schedules, steady-state plasma concentrations are reached within 24-48 hours and are generally less than 1 μg/mL. In controlled clinical trials, maximum metformin plasma levels (Cmax) did not exceed 5 μg/mL, even at maximum doses.
Distribution
Plasma protein binding is negligible. Metformin partitions into erythrocytes. The blood peak is lower than the plasma peak and appears at approximately the same time. The red blood cells most likely represent a secondary compartment of distribution. The mean Vd ranged between 63-276 l.
Biotransformation
Metformin is excreted unchanged in the urine. No metabolites have been identified in humans.
Elimination
Renal clearance of metformin is >400 mL/min, indicating that metformin is eliminated by glomerular filtration and tubular secretion. Following an oral dose, the apparent terminal elimination half-life is approximately 6.5 hours.
Special populations
Renal impairment
In patients with decreased renal function (based on measured creatinine clearance), the plasma and blood half-life of metformin is prolonged and the renal clearance is decreased in proportion to the decrease in creatinine clearance, leading to increased levels of metformin in plasma.
5.3. Preclinical safety data
Coadministration of dapagliflozin and metformin
Non-clinical data reveal no special hazard for humans based on conventional studies of repeated dose toxicity.
The following statements reflect the preclinical safety data of the individual active substances of Xigduo.
Dapagliflozin
Non-clinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated dose toxicity, genotoxicity, carcinogenic potential and fertility. Dapagliflozin did not induce tumours in either mice or rats at any of the doses evaluated in two-year carcinogenicity studies.
Reproductive and developmental toxicity
Direct administration of dapagliflozin to weanling juvenile rats and indirect exposure during late pregnancy (time periods corresponding to the second and third trimesters of pregnancy with respect to human renal maturation) and lactation are each associated with increased incidence and/or severity of renal pelvic and tubular dilatations in progeny.
In a juvenile toxicity study, when dapagliflozin was dosed directly to young rats from postnatal day 21 until postnatal day 90, renal pelvic and tubular dilatations were reported at all dose levels; pup exposures at the lowest dose tested were ≥15 times the maximum recommended human dose. These findings were associated with dose-related increases in kidney weight and macroscopic kidney enlargement observed at all doses. The renal pelvic and tubular dilatations observed in juvenile animals did not fully reverse within the approximate 1-month recovery period.
In a separate study of pre- and postnatal development, maternal rats were dosed from gestation day 6 through postnatal day 21, and pups were indirectly exposed in utero and throughout lactation. (A satellite study was conducted to assess dapagliflozin exposures in milk and pups.) Increased incidence or severity of renal pelvic dilatation was observed in adult offspring of treated dams, although only at the highest dose tested (associated maternal and pup dapagliflozin exposures were 1,415 times and 137 times, respectively, the human values at the maximum recommended human dose). Additional developmental toxicity was limited to dose-related reductions in pup body weights, and observed only at doses ≥15 mg/kg/day (associated with pup exposures that are ≥29 times the human values at the maximum recommended human dose). Maternal toxicity was evident only at the highest dose tested, and limited to transient reductions in body weight and food consumption at dose. The no observed adverse effect level (NOAEL) for developmental toxicity, the lowest dose tested, is associated with a maternal systemic exposure multiple that is approximately 19 times the human value at the maximum recommended human dose.
In additional studies of embryo-foetal development in rats and rabbits, dapagliflozin was administered for intervals coinciding with the major periods of organogenesis in each species. Neither maternal nor developmental toxicities were observed in rabbits at any dose tested; the highest dose tested is associated with a systemic exposure multiple of approximately 1,191 times the maximum recommended human dose. In rats, dapagliflozin was neither embryolethal nor teratogenic at exposures up to 1,441 times the maximum recommended human dose.
Metformin
Non-clinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated dose toxicity, genotoxicity, carcinogenic potential, toxicity to reproduction and development.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.