Pimavanserin
Chemical formula: C₂₅H₃₄FN₃O₂ Molecular mass: 427.564 g/mol PubChem compound: 10071196
Mechanism of action
The mechanism of action of pimavanserin in the treatment of hallucinations and delusions associated with Parkinson's disease psychosis is unclear. However, the effect of pimavanserin could be mediated through a combination of inverse agonist and antagonist activity at serotonin 5-HT2A receptors and to a lesser extent at serotonin 5-HT2C receptors.
Pharmacodynamic properties
In vitro, pimavanserin acts as an inverse agonist and antagonist at serotonin 5-HT2A receptors with high binding affinity (Ki value 0.087 nM) and at serotonin 5-HT2C receptors with lower binding affinity (Ki value 0.44 nM). Pimavanserin shows low binding to sigma 1 receptors (Ki value 120 nM) and has no appreciable affinity (Ki value >300 nM), to serotonin 5-HT2B, dopaminergic (including D2), muscarinic, histaminergic, or adrenergic receptors, or to calcium channels.
Cardiac Electrophysiology
The effect of pimavanserin on the QTc interval was evaluated in a randomized placebo- and positive-controlled double-blind, multiple-dose parallel thorough QTc study in 252 healthy subjects. A central tendency analysis of the QTc data at steady-state demonstrated that the maximum mean change from baseline (upper bound of the two-sided 90% CI) was 13.5 (16.6) msec at a dose of twice the therapeutic dose. A pharmacokinetic/pharmacodynamic analysis with pimavanserin suggested a concentration-dependent QTc interval prolongation in the therapeutic range.
In the 6-week, placebo-controlled effectiveness studies, mean increases in QTc interval of ~5-8 msec were observed in patients receiving once-daily doses of pimavanserin 34 mg. These data are consistent with the profile observed in a thorough QT study in healthy subjects. Sporadic QTcF values ≥500 msec and change from baseline values ≥60 msec were observed in subjects treated with pimavanserin 34 mg; although the incidence was generally similar for pimavanserin and placebo groups. There were no reports of torsade de pointes or any differences from placebo in the incidence of other adverse reactions associated with delayed ventricular repolarization in studies of pimavanserin, including those patients with hallucinations and delusions associated with PDP.
Pharmacokinetic properties
Pimavanserin demonstrates dose-proportional pharmacokinetics after single oral doses from 17 to 255 mg (0.5- to 7.5-times the recommended dosage). The pharmacokinetics of pimavanserin are similar in both the study population and healthy subjects. The mean plasma half-lives for pimavanserin and the active metabolite (N-desmethylated metabolite) are approximately 57 hours and 200 hours, respectively.
Absorption
The median Tmax of pimavanserin was 6 (range 4-24) hours and was generally unaffected by dose. The bioavailability of pimavanserin oral tablet and pimavanserin solution was essentially identical. The formation of the major circulating N-desmethylated metabolite AC-279 (active) from pimavanserin occurs with a median Tmax of 6 hours.
Administration of one 34 mg capsule once daily results in plasma pimavanserin concentrations that are similar to exposure with two 17 mg tablets once daily.
Effect of Food
Ingestion of a high-fat meal had no significant effect on rate (Cmax) and extent (AUC) of pimavanserin exposure. Cmax decreased by about 9% while AUC increased by about 8% with a high-fat meal.
Distribution
Pimavanserin is highly protein bound (~95%) in human plasma. Protein binding appeared to be dose-independent and did not change significantly over dosing time from Day 1 to Day 14. Following administration of a single dose of pimavanserin (34 mg), the mean (SD) apparent volume of distribution was 2173 (307) L.
Elimination
Metabolism
Pimavanserin is predominantly metabolized by CYP3A4 and CYP3A5 and to a lesser extent by CYP2J2, CYP2D6, and various other CYP and FMO enzymes. CYP3A4 is the major enzyme responsible for the formation of its major active metabolite (AC-279). Pimavanserin does not cause clinically significant CYP inhibition or induction of CYP3A4. Based on in vitro data, pimavanserin is not an irreversible inhibitor of any of the major hepatic and intestinal human CYP enzymes involved in drug metabolism (CYP1A2, 2B6, 2C8, 2C9, 2C19, 2D6, and 3A4).
Based on in vitro studies, transporters play no significant role in the disposition of pimavanserin.
AC-279 is neither a reversible or irreversible (metabolism-dependent) inhibitor of any of the major hepatic and intestinal human CYP enzymes involved in drug metabolism (CYP1A2, 2B6, 2C8, 2C9, 2C19, 2D6, and 3A4). AC-279 does not cause clinically significant CYP3A induction and is not predicted to cause induction of any other CYP enzymes involved in drug metabolism.
Excretion
Approximately 0.55% of the 34 mg oral dose of 14C-pimavanserin was eliminated as unchanged drug in urine and 1.53% was eliminated in feces after 10 days.
Less than 1% of the administered dose of pimavanserin and its active metabolite AC-279 were recovered in urine.
Specific Populations
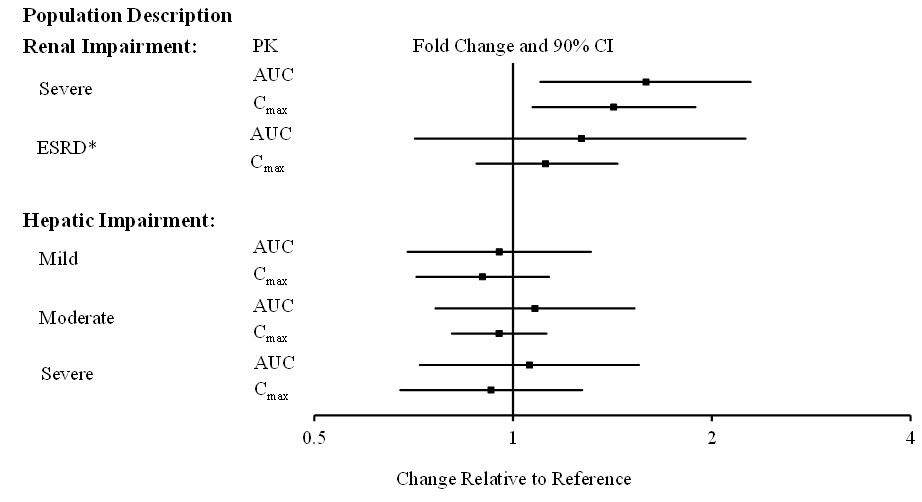
Population PK analysis indicated that age, sex, ethnicity, and weight do not have clinically relevant effect on the pharmacokinetics of pimavanserin. In addition, the analysis indicated that exposure of pimavanserin in patients with mild to moderate renal impairment was similar to exposure in patients with normal renal function.
The effects of other intrinsic factors on pimavanserin pharmacokinetics is shown in Figure 1.
Figure 1. Effects of Intrinsic Factors on Pimavanserin Pharmacokinetics:
* Less than 10% of the administered dose of pimavanserin was recovered in the dialysate.
Drug Interaction Studies
CYP3A4 Inhibitor: ketoconazole, a strong inhibitor of CYP3A4, increased pimavanserin Cmax by 1.5-fold and AUC by 3-fold. Population PK modeling and simulation show that steady-state exposure (Cmax,ss and AUCtau) for 10 mg pimavanserin with ketoconazole is similar to exposure for 34 mg pimavanserin alone.
CYP3A4 Inducer: In a clinical study where single doses of 34 mg pimavanserin were administered on Days 1 and 22, and 600 mg rifampin, a strong inducer of CYP3A4, was given daily on Days 15 through 21, pimavanserin Cmax and AUC decreased by 71% and 91%, respectively, compared to pre-rifampin plasma concentrations. In a simulation with a moderate CYP3A4 inducer (efavirenz), physiologically based pharmacokinetic (PBPK) models predicted pimavanserin Cmax,ss and AUCtau at steady state decreased by approximately 60% and 70%, respectively.
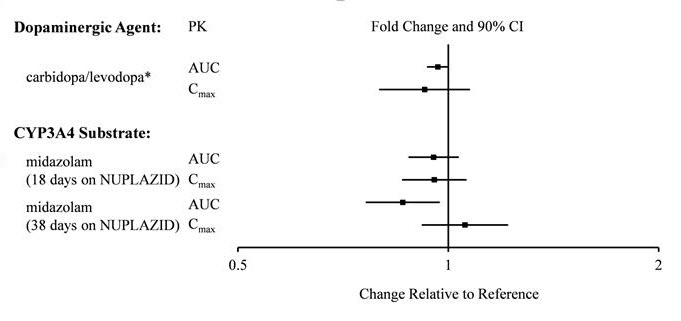
There is no effect of pimavanserin on the pharmacokinetics of midazolam, a CYP3A4 substrate, or carbidopa/levodopa as shown in Figure 2.
Figure 2. Effects of Pimavanserin on the Pharmacokinetics of Other Drugs:
* AUC and Cmax depict levodopa levels.
Preclinical safety data
Phospholipidosis (foamy macrophages and/or cytoplasmic vacuolation) was observed in multiple tissues and organs of mice, rats, and monkeys following oral daily administration of pimavanserin. The occurrence of phospholipidosis was both dose- and duration-dependent. The most severely affected organs were the lungs and kidneys. In rats, diffuse phospholipidosis was associated with increased lung and kidney weights, respiratory-related clinical signs including rales, labored breathing, and gasping, renal tubular degeneration, and, in some animals, focal/multifocal chronic inflammation in the lungs at exposures ≥10-times those at the maximum recommended human dose (MRHD) of 34 mg/day based on AUC. Phospholipidosis caused mortality in rats at exposures ≥16-times the MRHD of 34 mg/day based on AUC. The chronic inflammation in the rat lung was characterized by minimal to mild focal collagen positive fibroplasia as shown by specialized staining. Chronic inflammation of the lungs was not seen in monkeys treated for 12 months (exposures 9-times the MRHD). Based on the exposures at the estimated No Observed Effect Level (NOEL) for chronic lung inflammation in rats, there is a 5- to 9-times safety margin after 6-months of treatment and a 2- to 4-times safety margin after 24-months (lifetime) treatment compared to exposure at the MRHD. The relevance of these findings to human risk is not clear.
Related medicines
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.