BIPRETERAX Film-coated tablet Ref.[50602] Active ingredients: Indapamide Perindopril
Source: Web Search Revision Year: 2005
4.3. Contraindications
Linked to perindopril
- Hypersensitivity to the active substance or to any other ACE inhibitor
- History of angioedema (Quincke's oedema) associated with previous ACE inhibitor therapy (see section 4.4)
- Hereditary/idiopathic angioedema
- Second and third trimesters of pregnancy (see sections 4.4 and 4.6)
- Concomitant use of Bipreterax 10mg/2.5mg with aliskiren-containing products in patients with diabetes mellitus or renal impairment (GFR <60 ml/min/1.73 m²) (see sections 4.5 and 5.1)
- Concomitant use with sacubitril/valsartan (see sections 4.4 and 4.5).
- Extracorporeal treatments leading to contact of blood with negatively charged surfaces (see section 4.5)
- Significant bilateral renal artery stenosis or stenosis of the artery to a single functioning kidney (see section 4.4).
Linked to indapamide
- Hypersensitivity to the active substance or to any other sulphonamides
- Severe and moderate renal impairment (creatinine clearance below 60 ml/min)
- Hepatic encephalopathy
- Severe hepatic impairment
- Hypokalaemia
- As a general rule, this medicine is inadvisable in combination with non antiarrhythmic agents causing torsades de pointes (see section 4.5)
- Lactation (see section 4.6)
Linked to Bipreterax 10mg/2.5mg
- Hypersensitivity to any of the excipients listed in section 6.1
Due to the lack of sufficient therapeutic experience, Bipreterax 10mg/2.5mg should not be used in:
- Dialysis patients.
- Patients with untreated decompensated heart failure.
4.4. Special warnings and precautions for use
Special warnings
Common to perindopril and indapamide
Lithium
The combination of lithium and the combination of perindopril and indapamide is usually not recommended (see section 4.5).
Linked to perindopril
Dual blockade of the renin-angiotensin-aldosterone system (RAAS)
There is evidence that the concomitant use of ACE-inhibitors, angiotensin II receptor blockers or aliskiren increases the risk of hypotension, hyperkalaemia and decreased renal function (including acute renal failure). Dual blockade of RAAS through the combined use of ACE-inhibitors, angiotensin II receptor blockers or aliskiren is therefore not recommended (see sections 4.5 and 5.1). If dual blockade therapy is considered absolutely necessary, this should only occur under specialist supervision and subject to frequent close monitoring of renal function, electrolytes and blood pressure. ACE-inhibitors and angiotensin II receptor blockers should not be used concomitantly in patients with diabetic nephropathy.
Potassium-sparing drugs, potassium supplements or potassium-containing salt substitutes
The combination of perindopril and potassium-sparing drugs, potassium supplements or potassium-containg salt substitutes is usually not recommended (see section 4.5).
Neutropenia / agranulocytosis / thrombocytopenia / anaemia
Neutropenia/agranulocytosis, thrombocytopenia and anaemia have been reported in patients receiving ACE inhibitors. In patients with normal renal function and no other complicating factors, neutropenia occurs rarely. Perindopril should be used with extreme caution in patients with collagen vascular disease, immunosuppressant therapy, treatment with allopurinol or procainamide, or a combination of these complicating factors, especially if there is pre-existing impaired renal function. Some of these patients developed serious infections which in a few instances did not respond to intensive antibiotic therapy. If perindopril is used in such patients, periodical monitoring of white blood cell counts is advised and patients should be instructed to report any sign of infection (e.g. sore throat, fever) (see sections 4.5 and 4.8).
Renovascular hypertension
There is an increased risk of hypotension and renal insufficiency when patient with bilateral renal artery stenosis or stenosis of the artery to a single functioning kidney are treated with ACE inhibitors (see section 4.3). Treatment with diuretics may be a contributory factor. Loss of renal function may occur with only minor changes in serum creatinine even in patients with unilateral renal artery stenosis.
Hypersensitivity / angioedema
Angioedema of the face, extremities, lips, tongue, glottis and/or larynx has been reported rarely in patients treated with angiotensin converting enzyme inhibitors, including perindopril (see section 4.8). This may occur at any time during treatment. In such cases perindopril should be discontinued promptly and appropriate monitoring should be instituted to ensure complete resolution of symptoms prior to dismissing the patient. In those instances where swelling has been confined to the face and lips the condition generally resolved without treatment, although antihistamines have been useful in relieving symptoms. Angioedema associated with laryngeal oedema may be fatal. Where there is involvement of the tongue, glottis or larynx, likely to cause airway obstruction, appropriate therapy, which may include subcutaneous epinephrine solution 1:1000 (0.3 ml to 0.5 ml) and/or measures to ensure a patent airway, should be administered promptly.
Black patients receiving ACE inhibitors have been reported to have a higher incidence of angioedema compared to non-blacks.
Patients with a history of angioedema unrelated to ACE inhibitor therapy may be at increased risk of angioedema while receiving an ACE inhibitor (see section 4.3).
Intestinal angioedema has been reported rarely in patients treated with ACE inhibitors. These patients presented with abdominal pain (with or without nausea or vomiting); in some cases there was no prior facial angioedema and C-1 esterase levels were normal. The angioedema was diagnosed by procedures including abdominal CT scan, or ultrasound or at surgery and symptoms resolved after stopping the ACE inhibitor. Intestinal angioedema should be included in the differential diagnosis of patients on ACE inhibitors presenting with abdominal pain.
The combination of perindopril with sacubitril/valsartan is contraindicated due to the increased risk of angioedema (see section 4.3). Sacubitril/valsartan must not be initiated until 36 hours after taking the last dose of perindopril therapy. If treatment with sacubitril/valsartan is stopped, perindopril therapy must not be initiated until 36 hours after the last dose of sacubitril/valsartan (see sections 4.3 and 4.5). Concomitant use of other NEP inhibitors (e.g. racecadotril) and ACE inhibitors may also increase the risk of angioedema (see section 4.5). Hence, a careful benefit-risk assessment is needed before initiating treatment with NEP inhibitors (e.g. racecadotril) in patients on perindopril.
Concomitant use of mTOR inhibitors (e.g. sirolimus, everolimus, temsirolimus)
Patients taking concomitant mTOR inhibitors (e.g. sirolimus, everolimus, temsirolimus) therapy may be at increased risk for angioedema (e.g. swelling of the airways or tongue, with or without respiratory impairment) (see section 4.5).
Anaphylactoid reactions during desensitisation
There have been isolated reports of patients experiencing sustained, life-threatening anaphylactoid reactions while receiving ACE inhibitors during desensitisation treatment with hymenoptera (bees, wasps) venom. ACE inhibitors should be used with caution in allergic patients treated with desensitisation, and avoided in those undergoing venom immunotherapy. However these reactions could be prevented by temporary withdrawal of ACE inhibitor for at least 24 hours before treatment in patients who require both ACE inhibitors and desensitisation.
Anaphylactoid reactions during LDL apheresis
Rarely, patients receiving ACE inhibitors during low density lipoprotein (LDL)-apheresis with dextran sulphate have experienced life-threatening anaphylactoid reactions. These reactions were avoided by temporarily withholding ACE-inhibitor therapy prior to each apheresis.
Haemodialysis patients
Anaphylactoid reactions have been reported in patients dialysed with high-flux membranes (e.g., AN 69) and treated concomitantly with an ACE inhibitor. In these patients consideration should be given to using a different type of dialysis membrane or a different class of antihypertensive agent.
Primary aldosteronism
Patients with primary hyperaldosteronism generally will not respond to anti-hypertensive drugs acting through inhibition of the renin-angiotensin system. Therefore, the use of this product is not recommended.
Pregnancy
ACE inhibitors should not be initiated during pregnancy. Unless continued ACE inhibitor therapy is considered essential, patients planning pregnancy should be changed to alternative anti-hypertensive treatments which have an established safety profile for use in pregnancy. When pregnancy is diagnosed, treatment with ACE inhibitors should be stopped immediately, and, if appropriate, alternative therapy should be started (see sections 4.3 and 4.6).
Linked to indapamide:
Hepatic encephalopathy
When liver function is impaired, thiazide diuretics and thiazide-related diuretics may cause hepatic encephalopathy. Administration of the diuretic should be stopped immediately if this occurs.
Photosensitivity
Cases of photosensitivity reactions have been reported with thiazides and related thiazides diuretics (see section 4.8). If photosensitivity reaction occurs during treatment, it is recommended to stop the treatment. If a re-administration of the diuretic is deemed necessary, it is recommended to protect exposed areas to the sun or to artificial UVA.
Precautions for use
Common to perindopril and indapamide
Renal impairment
In cases of severe and moderate renal impairment (creatinine clearance < 60 ml/min), treatment is contraindicated.
In certain hypertensive patients without pre-existing apparent renal lesions and for whom renal blood tests show functional renal insufficiency, treatment should be stopped and possibly restarted either at a low dose or with one constituent only.
In these patients usual medical follow-up will include frequent monitoring of potassium and creatinine, after two weeks of treatment and then every two months during therapeutic stability period. Renal failure has been reported mainly in patients with severe heart failure or underlying renal failure including renal artery stenosis.
The drug is usually not recommended in case of bilateral renal artery stenosis or a single functioning kidney.
Hypotension and water and electrolyte depletion
There is a risk of sudden hypotension in the presence of pre-existing sodium depletion (in particular in individuals with renal artery stenosis). Therefore systematic testing should be carried out for clinical signs of water and electrolyte depletion, which may occur with an intercurrent episode of diarrhoea or vomiting. Regular monitoring of plasma electrolytes should be carried out in such patients. Marked hypotension may require the implementation of an intravenous infusion of isotonic saline. Transient hypotension is not a contraindication to continuation of treatment. After re-establishment of a satisfactory blood volume and blood pressure, treatment can be started again either at a reduced dose or with only one of the constituents.
Potassium levels
The combination of perindopril and indapamide does not prevent the onset of hypokalaemia particularly in diabetic patients or in patients with renal failure. As with any antihypertensive agent in combination with a diuretic, regular monitoring of plasma potassium levels should be carried out.
Excipients
Bipreterax 10mg/2.5mg should not be administered to patients with rare hereditary problems of galactose intolerance, total lactase deficiency or glucose-galactose malabsorption.
Level of sodium
Bipreterax 10mg/2.5mg contains less than 1 mmol sodium (23 mg) per tablet, i.e. essentially 'sodium-free'.
Linked to perindopril
Cough
A dry cough has been reported with the use of angiotensin converting enzyme inhibitors. It is characterised by its persistence and by its disappearance when treatment is withdrawn. An iatrogenic aetiology should be considered in the event of this symptom. If the prescription of an angiotensin converting enzyme inhibitor is still preferred, continuation of treatment may be considered.
Paediatric population
The efficacy and tolerability of perindopril in children and adolescents, alone or in combination, have not been established.
Risk of arterial hypotension and/or renal insufficiency (in cases of cardiac insufficiency, water and electrolyte depletion, etc...)
Marked stimulation of the renin-angiotensin-aldosterone system has been observed particularly during marked water and electrolyte depletions (strict sodium restricted diet or prolonged diuretic treatment), in patients whose blood pressure was initially low, in cases of renal artery stenosis, congestive heart failure or cirrhosis with oedema and ascites.
The blocking of this system with an angiotensin converting enzyme inhibitor may therefore cause, particularly at the time of the first administration and during the first two weeks of treatment, a sudden drop in blood pressure and/or an increase in plasma levels of creatinine, showing a functional renal insufficiency. Occasionally this can be acute in onset, although rare, and with a variable time to onset. In such cases, the treatment should then be initiated at a lower dose and increased progressively.
Elderly
Renal function and potassium levels should be tested before the start of treatment. The initial dose is subsequently adjusted according to blood pressure response, especially in cases of water and electrolyte depletion, in order to avoid sudden onset of hypotension.
Atherosclerosis
The risk of hypotension exists in all patients but particular care should be taken in patients with ischaemic heart disease or cerebral circulatory insufficiency, with treatment being started at a low dose.
Renovascular hypertension
The treatment for renovascular hypertension is revascularisation. Nonetheless, angiotensin converting enzyme inhibitors can be beneficial in patients presenting with renovascular hypertension who are awaiting corrective surgery or when such a surgery is not possible.
Treament with Bipreterax 10mg/2.5mg is not appropriate in patients with known or suspected renal artery stenosis because treatment should be started in a hospital setting at a dose lower than the Bipreterax 10mg/2.5mg one.
Cardiac failure / severe cardiac insufficiency
In patients with severe cardiac insufficiency (grade IV), treatment with Bipreterax 10mg/2.5mg is not appropriate because treatment should be started under medical supervision with a reduced initial dose. Treatment with beta-blockers in hypertensive patients with coronary insufficiency should not be stopped: the ACE inhibitor should be added to the beta-blocker.
Diabetic patients
In patients with insulin dependent diabetes mellitus (spontaneous tendency to increased levels of potassium), treatment with Bipreterax 10mg/2.5mg is not appropriate because treatment should be started under medical supervision with a reduced initial dose. The glycaemia levels should be closely monitored in diabetic patients previously treated with oral antidiabetic drugs or insulin, namely during the first month of treatment with an ACE inhibitor (see section 4.5).
Ethnic differences
As with other angiotensin converting enzyme inhibitors, perindopril is apparently less effective in lowering blood pressure in black people than in non-blacks, possibly because of a higher prevalence of low-renin states in the black hypertensive population.
Surgery / anaesthesia
Angiotensin converting enzyme inhibitors can cause hypotension in cases of anaesthesia, especially when the anaesthetic administered is an agent with hypotensive potential. It is therefore recommended that treatment with long-acting angiotensin converting enzyme inhibitors such as perindopril should be discontinued where possible one day before surgery.
Aortic or mitral valve stenosis / hypertrophic cardiomyopathy
ACE inhibitors should be used with caution in patient with an obstruction in the outflow tract of the left ventricle.
Hepatic failure
Rarely, ACE inhibitors have been associated with a syndrome that starts with cholestatic jaundice and progresses to fulminant hepatic necrosis and (sometimes) death. The mechanism of this syndrome is not understood. Patients receiving ACE inhibitors who develop jaundice or marked elevations of hepatic enzymes should discontinue the ACE inhibitor and receive appropriate medical follow-up (see section 4.8).
Hyperkalaemia
Elevations in serum potassium have been observed in some patients treated with ACE inhibitors, including perindopril. Risk factors for the development of hyperkalaemia include those with renal insufficiency, worsening of renal function, age (>70 years), diabetes mellitus, intercurrent events, in particular dehydration, acute cardiac decompensation, metabolic acidosis and concomitant use of potassium-sparing diuretics (e.g. spironolactone, eplerenone, triamterene, amiloride…), potassium supplements or potassiumcontaining salt substitutes; or those patients taking other drugs associated with increases in serum potassium (e.g. heparins, co-trimoxazole also known as trimethoprim/sulfamethoxazole, other ACE inhibitors, angiotensin-II receptor antagonists, acetylsalicylic acid ≥3 g/day, COX-2 inhibitors and non-selective NSAIDs, immunosuppressant agents such as ciclosporin or tacrolimus, trimethoprim).
The use of potassium supplements, potassium-sparing diuretics, or potassium-containing salt substitutes particularly in patients with impaired renal function may lead to a significant increase in serum potassium. Hyperkalaemia can cause serious, sometimes fatal arrhythmias. If concomitant use of the above-mentioned agents is deemed appropriate, they should be used with caution and with frequent monitoring of serum potassium (see section 4.5).
Linked to indapamide
Water and electrolyte balance:
Sodium levels
These should be tested before treatment is started, then at regular intervals. Reduction in sodium levels can be initially asymptomatic and regular testing is therefore essential. Testing should be more frequent in elderly and cirrhotic patients (see sections 4.8 and 4.9). Any diuretic treatment may cause hyponatraemia, sometimes with very serious consequences. Hyponatraemia with hypovolaemia may be responsible of dehydration and orthostatic hypotension. Concomitant loss of chloride ions may lead to secondary compensatory metabolic alkalosis: the incidence and degree of this effect are slight.
Potassium levels
Potassium depletion with hypokalaemia is a major risk with thiazide diuretics and thiazide-related diuretics. The risk of onset of lowered potassium levels (<3.4 mmol/l) should be prevented in some high risk populations such as elderly and/or malnourished subjects, whether or not they are taking multiple medications, cirrhotic patients with oedema and ascites, coronary patients and patients with heart failure. In such cases hypokalaemia increases the cardiac toxicity of cardiac glycosides and the risk of rhythm disorders.
Subjects presenting with a long QT interval are also at risk, whether the origin is congenital or iatrogenic. Hypokalaemia, as with bradycardia, acts as a factor which favours the onset of severe rhythm disorders, in particular torsades de pointes, which may be fatal.
In all cases more frequent testing of potassium levels is necessary. The first measurement of plasma potassium levels should be carried out during the first week following the start of treatment. If low potassium levels are detected, correction is required.
Calcium levels
Thiazide diuretics and thiazide-related diuretics may reduce urinary excretion of calcium and cause a mild and transient increase in plasma calcium levels. Markedly raised levels of calcium may be related to undiagnosed hyperparathyroidism. In such cases the treatment should be stopped before investigating the parathyroid function.
Blood glucose
Monitoring of blood glucose is important in diabetic patients, particularly when potassium levels are low.
Uric acid
Tendency to gout attacks may be increased in hyperuricaemic patients.
Renal function and diuretics
Thiazide diuretics and thiazide-related diuretics are only fully effective when renal function is normal or only slightly impaired (creatinine levels lower than approximately 25 mg/l, i.e. 220 µmol/l for an adult). In the elderly the value of plasma creatinine levels should be adjusted to take account of the age, weight and sex of the patient, according to the Cockroft formula:
clcr = (140 - age) x body weight / 0.814 x plasma creatinine level
with:
age expressed in years
body weight in kg
plasma creatinine level in micromol/l
This formula is suitable for an elderly male and should be adapted for women by multiplying the result by 0.85.
Hypovolaemia, resulting from the loss of water and sodium caused by the diuretic at the start of treatment, causes a reduction in glomerular filtration. It may result in an increase in blood urea and creatinine levels. This transitory functional renal insufficiency is of no adverse consequence in patients with normal renal function but may however worsen a pre-existing renal impairment.
Athletes
Athletes should note that this product contains an active substance which may cause a positive reaction in doping tests.
Acute myopia and secondary angle-closure glaucoma
Sulfonamide, or sulfonamide derivative, drugs can cause an idiosyncratic reaction resulting in transient myopia and acute angle-closure glaucoma. Untreated acute angle-closure glaucoma can lead to permanent vision loss. The primary treatment is to discontinue drug intake as rapidly as possible. Prompt medical or surgical treatments may need to be considered if the intraocular pressure remains uncontrolled. Risk factors for developing acute angle-closure glaucoma may include a history of sulfonamide or penicillin allergy.
4.5. Interaction with other medicinal products and other forms of interaction
Common to perindopril and indapamide
Concomitant use not recommended
Lithium: reversible increases in serum lithium concentrations and toxicity have been reported during concomitant administration of lithium with ACE inhibitors. Use of perindopril combined with indapamide with lithium is not recommended, but if the combination proves necessary, careful monitoring of serum lithium levels should be performed (see section 4.4).
Concomitant use which requires special care
- Baclofen: Increased antihypertensive effect. Monitor blood pressure and adapt antihypertensive dosage if necessary.
- Non-steroidal anti-inflammatory medicinal products (NSAIDs) (including aspirin ≥3g/day): when ACE-inhibitors are administered simultaneously with non-steroidal anti-inflammatory drugs (i.e. acetylsalicylic acid at anti-inflammatory dosage regimens, COX-2 inhibitors and non-selective NSAIDs), attenuation of the antihypertensive effect may occur. Concomitant use of ACE-inhibitors and NSAIDs may lead to an increased risk of worsening of renal function, including possible acute renal failure, and an increase in serum potassium, especially in patients with poor pre-existing renal function. The combination should be administered with caution, especially in the elderly. Patients should be adequately hydrated and consideration should be given to monitoring renal function after initiation of concomitant therapy, and periodically thereafter.
Concomitant use which requires some care
- Imipramine-like antidepressants (tricyclics), neuroleptics: Increased antihypertensive effect and increased risk of orthostatic hypotension (additive effect).
Linked to perindopril
Clinical trial data has shown that dual blockade of the renin-angiotensin-aldosterone-system (RAAS) through the combined use of ACE-inhibitors, angiotensin II receptor blockers or aliskiren is associated with a higher frequency of adverse events such as hypotension, hyperkalaemia and decreased renal function (including acute renal failure) compared to the use of a single RAAS-acting agent (see sections 4.3, 4.4 and 5.1).
Drugs inducing hyperkalaemia
Some drugs or therapeutic classes may increase the occurrence of hyperkalaemia: aliskiren, potassium salts, potassium-sparing diuretics, ACE inhibitors, angiotensin-II receptor antagonists, NSAIDs, heparins, immunosuppressant agents such as ciclosporin or tacrolimus, trimethoprim. The combination of these drugs increases the risk of hyperkalaemia.
Concomitant use contra-indicated (see section 4.3)
Aliskiren: In diabetic or impaired renal patients, risk of hyperkalaemia, worsening of renal function and cardiovascular morbidity and mortality increase.
Extracorporeal treatments: Extracorporeal treatments leading to contact of blood with negatively charged surfaces such as dialysis or haemofiltration with certain high-flux membranes (e.g. polyacrylonitril membranes) and low density lipoprotein apheresis with dextran sulphate due to increased risk of severe anaphylactoid reactions (see section 4.3). If such treatment is required, consideration should be given to using a different type of dialysis membrane or a different class of antihypertensive agent.
Sacubitril/valsartan: The concomitant use of perindopril with sacubitril/valsartan is contra-indicated as the concomitant inhibition of neprilysin and ACE may increase the risk of angioedema. Sacubitril/valsartan must not be started until 36 hours after taking the last dose of perindopril therapy. Perindopril therapy must not be started until 36 hours after the last dose of sacubitril/valsartan (see section 4.3 and 4.4).
Concomitant use not recommended
- Aliskiren: In patients other than diabetic or impaired renal patients, risk of hyperkalaemia, worsening of renal function and cardiovascular morbidity and mortality increase (see section 4.4).
- Concomitant therapy with ACE inhibitor and angiotensin-receptor blocker: It has been reported in the literature that in patients with established atherosclerotic disease, heart failure, or with diabetes with end organ damage, concomitant therapy with an ACE inhibitor and an angiotensin-receptor blocker is associated with a higher frequency of hypotension, syncope, hyperkalaemia, and worsening renal function (including acute renal failure) as compared to use of a single renin-angiotensin-aldosterone system agent. Dual blockade (e.g, by combining an ACE-inhibitor with an angiotensin II receptor antagonist) should be limited to individually defined cases with close monitoring of renal function, potassium levels, and blood pressure (see section 4.4).
- Estramustine: Risk of increased adverse effects such as angioneurotic oedema (angioedema).
- Co-trimoxazole (trimethoprim/sulfamethoxazole): Patients taking concomitant co-trimoxazole (trimethoprim/sulfamethoxazole) may be at increased risk for hyperkalaemia (see section 4.4).
- Potassium-sparing diuretics (e.g. triamterene, amiloride), potassium (salts): Hyperkalaemia (potentially lethal), especially in conjunction with renal impairment (additive hyperkalaemic effects). The combination of perindopril with the above-mentioned drugs is not recommended (see section 4.4). If concomitant use is nonetheless indicated, they should be used with caution and with frequent monitoring of serum potassium. For use of spironolactone in heart failure, see section "Concomitant use which requires special care".
Concomitant use which requires special care
- Antidiabetic agents (insulin, oral hypoglycaemic agents): Epidemiological studies have suggested that concomitant administration of ACE inhibitors and antidiabetic medicines (insulins, oral hypoglycaemic agents) may cause an increased blood-glucose lowering effect with risk of hypoglycaemia. This phenomenon appeared to be more likely to occur during the first weeks of combined treatment and in patients with renal impairment.
- Non-potassium-sparing diuretics: Patients on diuretics, and especially those who are volume and/or salt depleted, may experience excessive reduction in blood pressure after initiation of therapy with an ACE inhibitor. The possibility of hypotensive effects can be reduced by discontinuation of the diuretic, by increasing volume or salt intake prior to initiating therapy with low and progressive doses of perindopril.
In arterial hypertension, when prior diuretic therapy can have caused salt/volume depletion, either the diuretic must be discontinued before initiating the ACE inhibitor, in which case a non-potassium-sparing diuretic can be thereafter reintroduced or the ACE inhibitor must be initiated with a low dosage and progressively increased.
In diuretic-treated congestive heart failure, the ACE inhibitor should be initiated at a very low dosage, possibly after reducing the dosage of the associated non-potassium-sparing diuretic. In all cases, renal function (creatinine levels) must be monitored during the first few weeks of ACE inhibitor therapy.
- Potassium-sparing diuretics (eplerenone, spironolactone): With eplerenone or spironolactone at doses between 12.5 mg to 50 mg per day and with low doses of ACE inhibitors:
In the treatment of class II-IV heart failure (NYHA) with an ejection fraction <40%, and previously treated with ACE inhibitors and loop diuretics, risk of hyperkalaemia, potentially lethal, especially in case of non-observance of the prescription recommendations about this combination. Before initiating the combination, check the absence of hyperkalaemia and renal impairment. Close monitoring of the kalaemia and creatininemia is recommended in the first month of the treatment once a week at the beginning and, monthly thereafter.
- Racecadotril: ACE inhibitors (e.g. perindopril) are known to cause angioedema. This risk may be elevated when used concomitantly with racecadotril (a drug used against acute diarrhea).
- mTOR inhibitors (e.g. sirolimus, everolimus, temsirolimus): patients taking concomitant mTOR inhibitors therapy may be at increased risk for angioedema (see section 4.4).
Concomitant use which requires some care
- Antihypertensive agents and vasodilatators: Concomitant use of these agents may increase the hypotensive effects of perindopril. Concomitant use with nitroglycerin and other nitrates, or other vasodilatators, may further reduce blood pressure.
- Allopurinol, cytostatic or immunosuppressive agents, systemic corticosteroids or procainamide: Concomitant administration with ACE inhibitors may lead to an increased risk for leucopenia (see section 4.4).
- Anaesthetic drugs: ACE inhibitors may enhance the hypotensive effects of certain anaesthetic drugs (see section 4.4).
- Gliptins (linagliptin, saxagliptin, sitagliptin, vildagliptin): Increased risk of angio-oedema, due to dipeptidyl peptidase IV (DPP-IV) decreased activity by the gliptin, in patients co-treated with an ACE inhibitor.
- Sympathomimetics: Sympathomimetics may reduce the antihypertensive effects of ACE inhibitors.
- Gold: Nitritoid reactions (symptoms include facial flushing, nausea, vomiting and hypotension) have been reported rarely in patients on therapy with injectable gold (sodium aurothiomalate) and concomitant ACE inhibitor therapy including perindopril.
Linked to indapamide
Concomitant use which requires special care
- Torsades de pointes inducing drugs: Due to the risk of hypokalemia, indapamide should be administered with caution when associated with medicinal products that induced torsades de pointes such as class IA antiarrhythmic agents (quinidine, hydroquinidine, disopyramide); class III antiarrhythmic agents (amiodarone, dofetilide, ibutilide, bretylium, sotalol); some neuroleptics (chlorpromazine, cyamemazine, levomepromazine, thioridazine, trifluoperazine), benzamides (amisulpride, sulpiride, sultopride, tiapride), butyrophenones (droperidol, haloperidol), other neuroleptics (pimozide); other substances such as bepridil, cisapride, diphemanil, IV erythromycin, halofantrine, mizolastine, moxifloxacin, pentamidine, sparfloxacin, IV vincamine, methadone, astemizole, terfenadine. Prevention of low potassium levels and correction if necessary: monitoring of the QT interval.
- Potassium-lowering drugs: amphotericin B (IV route), glucocorticoids and mineralocorticoids (systemic route), tetracosactide, stimulant laxatives: Increased risk of low potassium levels (additive effect). Monitoring of potassium levels, and correction if necessary; particular consideration required in cases of treatment with digitalis. Non stimulant laxatives should be used.
- Digitalis preparations: Low potassium levels favour the toxic effects of digitalis. Potassium levels and ECG should be monitored and treatment reconsidered if necessary.
- Allopurinol: concomitant treatment with indapamide may increase the incidence of hypersensitivity reactions to allopurinol.
Concomitant use which requires some care
- Potassium-sparing diuretics (amiloride, spironolactone, triamterene): Whilst rational combinations are useful in some patients, hypokalaemia or hyperkalaemia (particularly in patients with renal failure or diabetes) may still occur. Plasma potassium and ECG should be monitored and, if necessary, treatment reviewed.
- Metformin: Lactic acidosis due to metformin caused by possible functional renal insufficiency linked to diuretics and in particular to loop diuretics. Do not use metformin when plasma creatinine levels exceed 15 mg/l (135 micromol/l) in men and 12 mg/l (110 micromol/l) in women.
- Iodinated contrast media: In cases of dehydration caused by diuretics, there is an increased risk of acute renal insufficiency, particularly when high doses of iodinated contrast media are used. Rehydration should be carried out before the iodinated compound is administered.
- Calcium (salts): Risk of increased levels of calcium due to reduced elimination of calcium in the urine.
- Ciclosporin, tacrolimus: Risk of increased creatinine levels with no change in circulating levels of ciclosporin, even when there is no salt and water depletion.
- Corticosteroids, tetracosactide (systemic route): Reduction in antihypertensive effect (salt and water retention due to corticosteroids).
4.6. Fertility, pregnancy and lactation
Given the effects of the individual components in this combination product on pregnancy and lactation, Bipreterax 10mg/2.5mg is not recommended during the first trimester of pregnancy. Bipreterax 10mg/2.5mg is contraindicated during the second and third trimesters of pregnancy.
Bipreterax 10mg/2.5mg is contraindicated during lactation. A decision should therefore be made whether to discontinue nursing or to discontinue Bipreterax 10mg/2.5mg taking account the importance of this therapy for the mother.
Pregnancy
Linked to perindopril
The use of ACE inhibitors is not recommended during the first trimester of pregnancy (see section 4.4). The use of ACE inhibitors is contra-indicated during the second and third trimesters of pregnancy (see sections 4.3 and 4.4).
Epidemiological evidence regarding the risk of teratogenicity following exposure to ACE inhibitors during the first trimester of pregnancy has not been conclusive; however a small increase in risk cannot be excluded. Unless continued ACE inhibitor therapy is considered essential, patients planning pregnancy should be changed to alternative anti-hypertensive treatments which have an established safety profile for use in pregnancy. When pregnancy is diagnosed, treatment with ACE inhibitors should be stopped immediately, and, if appropriate, alternative therapy should be started.
Exposure to ACE inhibitor therapy exposure during the second and third trimesters is known to induce human fœtotoxicity (decreased renal function, oligohydramnios, skull ossification retardation) and neonatal toxicity (renal failure, hypotension, hyperkalaemia) (see section 5.3).
Should exposure to ACE inhibitors have occurred from the second trimester of pregnancy, ultrasound check of renal function and skull is recommended.
Infants whose mothers have taken ACE inhibitors should be closely observed for hypotension (see sections 4.3 and 4.4).
Linked to indapamide
There are no or limited amount of data (less than 300 pregnancy outcomes) from the use of indapamide in pregnant women. Prolonged exposure to thiazide during the third trimester of pregnancy can reduce maternal plasma volume as well as uteroplacental blood flow, which may cause a fœto-placental ischemia and growth retardation.
Animal studies do not indicate direct or indirect harmful effects with respect to reproductive toxicity (see section 5.3). As a precautionary measure, it is preferable to avoid the use of Indapamide during pregnancy.
Breast-feeding
Bipreterax 10mg/2.5mg is contraindicated during breast-feeding.
Linked to perindopril
Because no information is available regarding the use of perindopril during breast-feeding, perindopril is not recommended and alternative treatments with better established safety profiles during breast-feeding are preferable, especially while nursing a newborn or preterm infant.
Linked to indapamide
There is insufficient information on the excretion of indapamide/metabolites in human milk. Hypersensitivity to sulfonamide-derived drugs, hypokalaemia might occur. A risk to the newborns/infants cannot be excluded.
Indapamide is closely related to thiazide diuretics which have been associated, during breast-feeding, with decrease or even suppression of milk lactation.
Indapamide is contra-indicated during breast-feeding.
Fertility
Common to perindopril and indapamide
Reproductive toxicity studies showed no effect on fertility in female and male rats (see section 5.3). No effects on human fertility are anticipated.
4.7. Effects on ability to drive and use machines
Linked to perindopril, indapamide and Bipreterax 10mg/2.5mg
The two active substances, individually or combined in Bipreterax 10mg/2.5mg, have no influence on the ability to drive and use machines but individual reactions related to low blood pressure may occur in some patients, particularly at the start of treatment or in combination with another antihypertensive medication. As a result the ability to drive or operate machinery may be impaired.
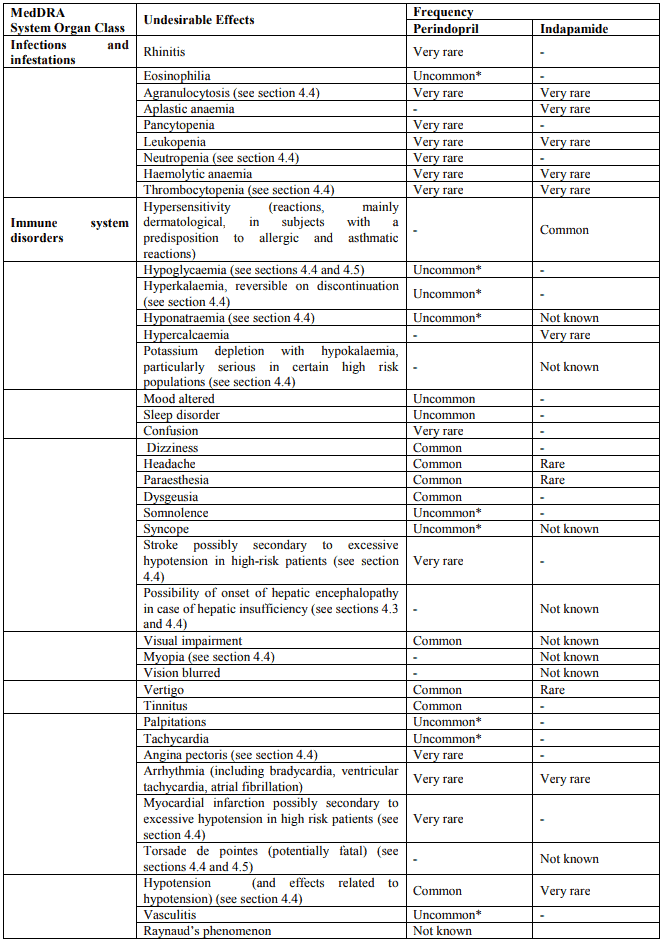
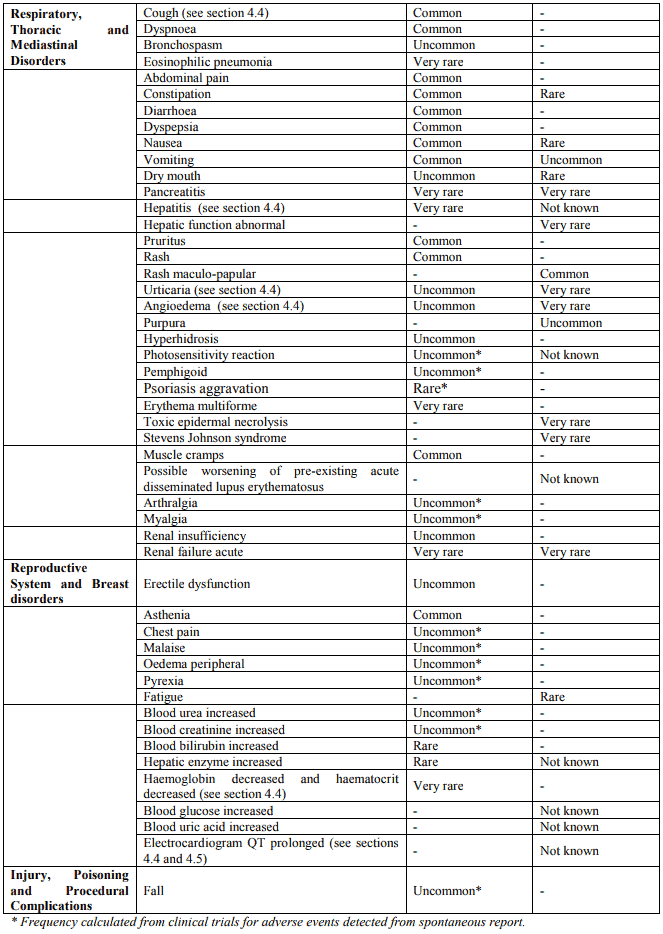
4.8. Undesirable effects
a. Summary of safety profile
The administration of perindopril inhibits the renin-angiotensin-aldosterone axis and tends to reduce the potassium loss caused by indapamide.
Six percent of the patients on treatment with Bipreterax 10mg/2.5mg experience hypokalaemia (potassium level <3.4 mmol/l).
The most commonly reported adverse reactions observed are:
- with perindopril: dizziness, headache, paraesthesia, dysgeusia, visual impairment, vertigo, tinnitus, hypotension, cough, dyspnoea, abdominal pain, constipation, dyspepsia, diarrhoea, nausea, vomiting, pruritus, rash, muscle cramps and asthenia.
- with indapamide: hypersensitivity reactions, mainly dermatological, in subjects with a predisposition to allergic and asthmatic reactions and maculopapular rashes.
b. Tabulated list of adverse reactions
The following undesirable effects have been observed during clinical trials and/or post-marketing use and ranked under the following frequency: Very common (1/10); common (1/100, <1/10); uncommon (1/1000, <1/100); rare (1/10000, <1/1000), very rare (<1/10000), not known (cannot be estimated from the available data).
Cases of SIADH have been reported with other ACE inhibitors. SIADH can be considered as a very rare but possible complication associated with ACE inhibitor therapy including perindopril.
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the national reporting system listed in Appendix V.
6.2. Incompatibilities
Not applicable.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.