EDARBYCLOR Tablet Ref.[10008] Active ingredients: Azilsartan medoxomil Chlortalidone
Source: FDA, National Drug Code (US) Revision Year: 2020
12.1. Mechanism of Action
The active ingredients of Edarbyclor target two separate mechanisms involved in blood pressure regulation.
Azilsartan medoxomil
Angiotensin II is formed from angiotensin I in a reaction catalyzed by angiotensin-converting enzymes (ACE, kinase II). Angiotensin II is the principle pressor agent of the renin-angiotensin system, with effects that include vasoconstriction, stimulation of synthesis and release of aldosterone, cardiac stimulation, and renal reabsorption of sodium. Azilsartan medoxomil is an orally administered prodrug that is rapidly converted by esterases during absorption to the active moiety, azilsartan. Azilsartan blocks the vasoconstrictor and aldosterone-secreting effects of angiotensin II by selectively blocking the binding of angiotensin II to the AT1 receptor in many tissues, such as vascular smooth muscle and the adrenal gland. Its action is, therefore, independent of the pathway for angiotensin II synthesis.
An AT2 receptor is also found in many tissues, but this receptor is not known to be associated with cardiovascular homeostasis. Azilsartan has more than a 10,000-fold greater affinity for the AT1 receptor than for the AT2 receptor.
Blockade of the renin-angiotensin system with ACE inhibitors, which inhibit the biosynthesis of angiotensin II from angiotensin I, is widely used in the treatment of hypertension. ACE inhibitors also inhibit the degradation of bradykinin, a reaction catalyzed by ACE. Because azilsartan does not inhibit ACE (kinase II), it should not affect bradykinin levels. Whether this difference has clinical relevance is not yet known. Azilsartan does not bind to or block other receptors or ion channels known to be important in cardiovascular regulation.
Blockade of the angiotensin II receptor inhibits the negative regulatory feedback of angiotensin II on renin secretion, but the resulting increased plasma renin activity and angiotensin II circulating levels do not overcome the effect of azilsartan on blood pressure.
Chlorthalidone
Chlorthalidone produces diuresis with increased excretion of sodium and chloride. The site of action appears to be the distal renal tubule (early convoluted part), inhibiting NaCl reabsorption (by antagonizing the Na+-Cl-cotransporter) and promoting Ca++ reabsorption (by an unknown mechanism). The enhanced delivery of Na+ and water to the cortical collecting tubule and/or the increased flow rate leads to increased secretion and elimination of K+ and H+. The diuretic effects of chlorthalildone lead to decreased extracellular fluid volume, plasma volume, cardiac output, total exchangeable sodium, glomerular filtration rate, and renal plasma flow. Although the mechanism of action of chlorthalidone and related drugs is not wholly clear, sodium and water depletion appear to provide a basis for its antihypertensive effect.
12.2. Pharmacodynamics
Edarbyclor
Edarbyclor tablets have been shown to be effective in lowering blood pressure. Both azilsartan medoxomil and chlorthalidone lower blood pressure by reducing peripheral resistance but through complementary mechanisms.
Azilsartan medoxomil
Azilsartan inhibits the pressor effects of an angiotensin II infusion in a dose-related manner. An azilsartan single dose equivalent to 32 mg azilsartan medoxomil inhibited the maximal pressor effect by approximately 90% at peak, and approximately 60% at 24 hours. Plasma angiotensin I and II concentrations and plasma renin activity increased while plasma aldosterone concentrations decreased after single and repeated administration of azilsartan medoxomil to healthy subjects; no clinically significant effects on serum potassium or sodium were observed.
Chlorthalidone
The diuretic effect of chlorthalidone occurs in approximately 2.6 hours and continues for up to 72 hours.
12.3. Pharmacokinetics
Edarbyclor
Following oral administration of Edarbyclor, peak plasma concentrations of azilsartan and chlorthalidone are reached at 3 and 1 hours, respectively. The rate (Cmax and Tmax) and extent (AUC) of absorption of azilsartan are similar when it is administered alone or with chlorthalidone. The extent (AUC) of absorption of chlorthalidone is similar when it is administered alone or with azilsartan medoxomil; however, the Cmax of chlorthalidone from Edarbyclor was 45-47% higher.
There is no clinically significant effect of food on the bioavailability of azilsartan or chlorthalidone following administration of Edarbyclor.
Absorption
Azilsartan medoxomil is an orally administered prodrug that is rapidly converted by esterases during absorption to the active moiety, azilsartan. Azilsartan medoxomil is not detected in plasma after oral administration. Dose proportionality in exposure was established for azilsartan in the azilsartan medoxomil dose range of 20 mg to 320 mg after single or multiple dosing.
The estimated absolute bioavailability of azilsartan following administration of azilsartan medoxomil is approximately 60%. After oral administration of azilsartan medoxomil, peak plasma concentrations (Cmax) of azilsartan are reached within 1.5 to 3 hours. Food does not affect the bioavailability of azilsartan.
Distribution
Azilsartan medoxomil: The volume of distribution of azilsartan is approximately 16L. Azilsartan is highly bound to human plasma proteins (>99%), mainly serum albumin. Protein binding is constant at azilsartan plasma concentrations well above the range achieved with recommended doses.
In rats, minimal azilsartan-associated radioactivity crossed the blood-brain barrier. Azilsartan passed across the placental barrier in pregnant rats and was distributed to the fetus.
Chlorthalidone: In whole blood, chlorthalidone is predominantly bound to erythrocyte carbonic anhydrase. In the plasma, approximately 75% of chlorthalidone is bound to plasma proteins, 58% of the drug being bound to albumin. Chlorthalidone crosses the placental barrier and passes into breast milk. When mothers were treated before and after birth with 50 mg chlorthalidone daily, chlorthalidone levels in fetal whole blood were around 15% of those found in maternal blood. Chlorthalidone concentrations in amniotic fluid and breast milk are approximately 4% of those found in maternal blood.
Metabolism and Elimination
Azilsartan medoxomil: Azilsartan medoxomil, when administered alone or in combination with chlorthalidone is eliminated from plasma with an elimination half-life of 11-13 hours. Azilsartan is metabolized to two primary metabolites. The major metabolite in plasma is formed by O-dealkylation, referred to as metabolite M-II, and the minor metabolite is formed by decarboxylation, referred to as metabolite M-I. Systemic exposures to the major and minor metabolites in humans were approximately 50% and less than 1% of azilsartan, respectively. M-I and M-II do not contribute to the pharmacologic activity of azilsartan medoxomil. The major enzyme responsible for azilsartan metabolism is CYP2C9.
Following an oral dose of 14C-labeled azilsartan medoxomil, approximately 55% of radioactivity was recovered in feces and approximately 42% in urine, with 15% of the dose excreted in urine as azilsartan. The elimination half-life of azilsartan is approximately 11 hours and renal clearance is approximately 2.3 mL/min. Steady-state levels of azilsartan are achieved within 5 days and no accumulation in plasma occurs with repeated once-daily dosing.
Chlorthalidone: Chlorthalidone when administered alone or in combination with azilsartan medoxomil is eliminated from plasma with an elimination half-life of 42-45 hours. The elimination half-life is unaltered following repeat dosing. The majority of an absorbed quantity of chlorthalidone is excreted by the kidneys with a mean renal clearance of 46-70 mL/min. By contrast, metabolism and excretion via the liver and bile play a minor role in the elimination of the substance. Approximately 60%-70% of chlorthalidone is excreted in the urine and feces within 120 hours, mainly in unchanged form.
Specific Populations
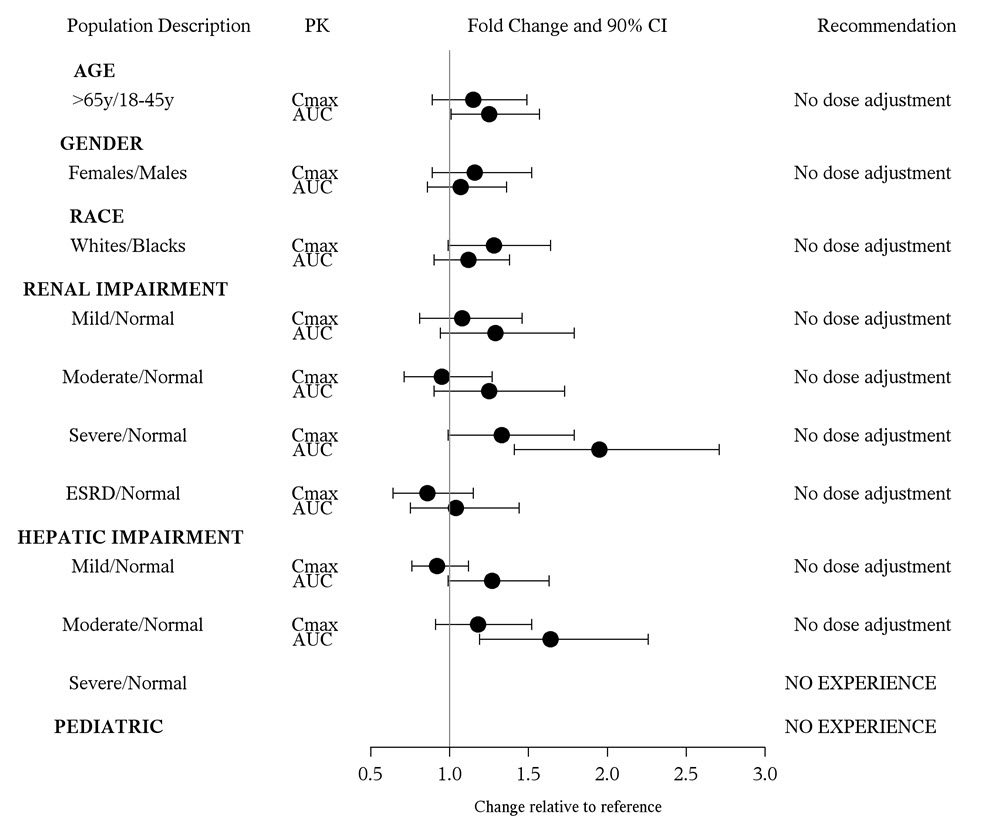
Azilsartan medoxomil: The effect of demographic and functional factors on the pharmacokinetics of azilsartan was studied in single and multiple dose studies. Pharmacokinetic measures indicating the magnitude of the effect on azilsartan are presented in Figure 2 as change relative to reference (test/reference).
Figure 2. Impact of intrinsic factors on the pharmacokinetics of azilsartan:
Drug Interactions
Azilsartan medoxomil: No clinically significant drug interactions have been observed in studies of azilsartan medoxomil or azilsartan given with amlodipine, antacids, chlorthalidone, digoxin, fluconazole, glyburide, ketoconazole, metformin, pioglitazone, and warfarin. Therefore, azilsartan medoxomil may be used concomitantly with these medications.
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenicity, mutagenicity, or fertility studies have been conducted with the combination of azilsartan medoxomil and chlorthalidone or with chlorthalidone alone. However, these studies have been conducted for azilsartan medoxomil, azilsartan and M-II.
Carcinogenesis
Azilsartan medoxomil was not carcinogenic when assessed in 26-week transgenic (Tg.rasH2) mouse and 2-year rat studies. The highest doses tested (450 mg azilsartan medoxomil/kg/day in the mouse and 600 mg azilsartan medoxomil/kg/day in the rat) produced exposures to azilsartan that are 12 (mice) and 27 (rats) times the average exposure to azilsartan in humans given the maximum recommended human dose (MRHD, 80 mg azilsartan medoxomil/day). M-II was not carcinogenic when assessed in 26-week Tg.rasH2 mouse and 2-year rat studies. The highest doses tested (approximately 8000 mg M-II/kg/day (males) and 11,000 mg M-II/kg/day (females) in the mouse and 1000 mg M-II/kg/day (males) and up to 3000 mg M-II/kg/day (females) in the rat) produced exposures that are, on average, about 30 (mice) and 7 (rats) times the average exposure to M-II in humans at the MRHD.
Mutagenesis
Chlorthalidone demonstrated no potential for mutagenic effects at non-cytotoxic concentrations and is considered not to pose a mutagenic risk to humans.
Azilsartan medoxomil, azilsartan, and M-II were positive for structural aberrations in the Chinese Hamster Lung Cytogenic Assay. In this assay, structural chromosomal aberrations were observed with the prodrug, azilsartan medoxomil, without metabolic activation. The active moiety, azilsartan, was also positive in this assay both with and without metabolic activation. The major human metabolite, M-II was also positive in this assay during a 24-hr assay without metabolic activation.
Azilsartan medoxomil, azilsartan, and M-II were devoid of genotoxic potential in the Ames reverse mutation assay with Salmonella typhimurium and Escherichia coli, the in vitro Chinese Hamster Ovary Cell forward mutation assay, the in vitro mouse lymphoma (tk) gene mutation test, the ex vivo unscheduled DNA synthesis test, and the in vivo mouse and/or rat bone marrow micronucleus assay.
Impairment of Fertility
Chlorthalidone at a dosage of 100 mg/kg had no effect on fertility in rats. There was no effect of azilsartan medoxomil on the fertility of male or female rats at oral doses of up to 1000 mg azilsartan medoxomil/kg/day [6000 mg/m2 (approximately 122 times the MRHD of 80 mg azilsartan medoxomil/60 kg on a mg/m2 basis)]. Fertility of rats also was unaffected at doses of up to 3000 mg M-II/kg/day.
14. Clinical Studies
The antihypertensive effects of Edarbyclor have been demonstrated in a total of 5 randomized controlled studies, which included 4 double-blind, active-controlled studies and 1 open-label, long-term active-controlled study. The studies ranged from 8 weeks to 12 months in duration, at doses ranging from 20/12.5 mg to 80/25 mg once daily. A total of 5310 patients (3082 given Edarbyclor and 2228 given active comparator) with moderate or severe hypertension were studied. Overall, randomized patients had a mean age of 57 years, and included 52% males, 72% whites, 21% blacks, 15% with diabetes, 70% with mild or moderate renal impairment, and a mean BMI of 31.6 kg/m2.
An 8-week, multicenter, randomized, double-blind, active-controlled, parallel group factorial trial in patients with moderate to severe hypertension compared the effect on blood pressure of Edarbyclor with the respective monotherapies. The trial randomized 1714 patients with baseline systolic blood pressure between 160 and 190 mm Hg (mean 165 mm Hg) and a baseline diastolic blood pressure <119 mm Hg (mean 95 mm Hg) to one of the 11 active treatment arms.
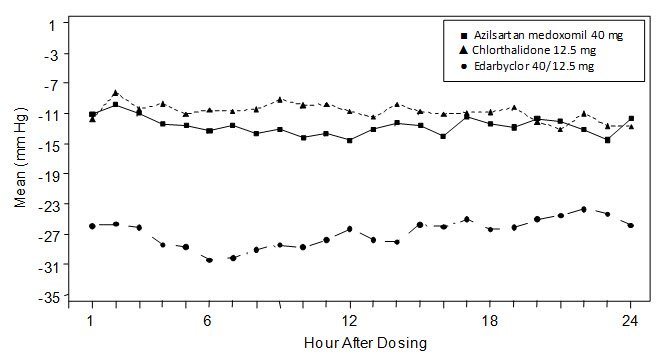
The 6 treatment combinations of azilsartan medoxomil 20, 40, or 80 mg and chlorthalidone 12.5 or 25 mg resulted in statistically significant reduction in systolic and diastolic blood pressure as determined by ambulatory blood pressure monitoring (ABPM) (Table 2) and clinic measurement (Table 3) at trough compared with the respective individual monotherapies. The clinic blood pressure reductions appear larger than those observed with ABPM, because the former include a placebo effect, which was not directly measured. Most of the antihypertensive effect of Edarbyclor occurs within 1-2 weeks of dosing. The blood pressure lowering effect was maintained throughout the 24-hour period (Figure 3).
Table 2. Mean Change from Baseline in Systolic/Diastolic Blood Pressure (mm Hg) as Measured by ABPM at Trough (22-24 Hours Post-Dose) at Week 8: Combination Therapy vs Monotherapy:
| Chlorthalidone, mg | Azilsartan Medoxomil, mg | |||
|---|---|---|---|---|
| 0 | 20 | 40 | 80 | |
| 0 | N/A | -12 / -8 | -13 / -7 | -15 / -9 |
| 12.5 | -13 / -7 | -23 / -13 | -24 / -14 | -26 / -17 |
| 25 | -16 / -8 | -26 / -15 | -30 / -17 | -28 / -16 |
Table 3. Mean Change from Baseline in Clinic Systolic/Diastolic Blood Pressure (mm Hg) at Week 8: Combination Therapy vs Monotherapy:
| Chlorthalidone, mg | Azilsartan Medoxomil, mg | |||
|---|---|---|---|---|
| 0 | 20 | 40 | 80 | |
| 0 | N/A | -20 / -7 | -23 / -9 | -24 / -10 |
| 12.5 | -21 / -7 | -34 / -14 | -37 / -16 | -37 / -17 |
| 25 | -27 / -9 | -37 / - 16 | -40 / -17 | -40 / -19 |
Figure 3. Mean Change from Baseline at Week 8 in Ambulatory Systolic Blood Pressure (mm Hg) by Treatment and Hour
Edarbyclor was effective in reducing blood pressure regardless of age, gender, or race.
Edarbyclor was effective in treating black patients (usually a low-renin population).
In a 12-week, double-blind forced-titration trial, Edarbyclor 40/25 mg was statistically superior (P<0.001) to olmesartan medoxomil-hydrochlorothiazide (OLM/HCTZ) 40/25 mg in reducing systolic blood pressure in patients with moderate to severe hypertension (Table 4). Similar results were observed in all subgroups, including age, gender, or race of patients.
Table 4. Mean Change in Systolic/Diastolic Blood Pressure (mm Hg) at Week 12
| Edarbyclor 40/25 mg N=355 | OLM/HCTZ 40/25 mg N=364 | |
|---|---|---|
| Clinic (Mean Baseline 165/96 mm Hg) | -43 / -19 | -37 / -16 |
| Trough by ABPM (22-24 hours) (Mean Baseline 153/92 mm Hg) | -33 / -20 | -26 / -16 |
Edarbyclor lowered blood pressure more effectively than OLM/HCTZ at each hour of the 24-hour interdosing period as measured by ABPM.
Cardiovascular Outcomes
There are no trials of Edarbyclor demonstrating reductions in cardiovascular risk in patients with hypertension; however, trials with chlorthalidone and at least one drug pharmacologically similar to azilsartan medoxomil have demonstrated such benefits.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.