ENTEREG Capsule Ref.[9957] Active ingredients: Alvimopan
Source: FDA, National Drug Code (US) Revision Year: 2020
12.1. Mechanism of Action
Alvimopan is a selective antagonist of the cloned human μ-opioid receptor with a Ki of 0.4 nM (0.2 ng/mL) and no measurable opioid-agonist effects in standard pharmacologic assays. The dissociation of [3H]-alvimopan from the human μ-opioid receptor is slower than that of other opioid ligands, consistent with its higher affinity for the receptor. At concentrations of 1 to 10 µM, alvimopan demonstrated no activity at any of over 70 non-opioid receptors, enzymes, and ion channels.
Postoperative ileus is the impairment of gastrointestinal motility after intra-abdominal surgery or other, non-abdominal surgeries. Postoperative ileus affects all segments of the gastrointestinal tract and may last from 5 to 6 days, or even longer. This may potentially delay gastrointestinal recovery and hospital discharge until its resolution. It is characterized by abdominal distention and bloating, nausea, vomiting, pain, accumulation of gas and fluids in the bowel, and delayed passage of flatus and defecation. Postoperative ileus is the result of a multifactorial process that includes inhibitory sympathetic input and release of hormones, neurotransmitters, and other mediators (e.g., endogenous opioids). A component of postoperative ileus also results from an inflammatory reaction and the effects of opioid analgesics. Morphine and other μ-opioid receptor agonists are universally used for the treatment of acute postsurgical pain; however, they are known to have an inhibitory effect on gastrointestinal motility and may prolong the duration of postoperative ileus.
Following oral administration, alvimopan antagonizes the peripheral effects of opioids on gastrointestinal motility and secretion by competitively binding to gastrointestinal tract μ-opioid receptors. The antagonism produced by alvimopan at opioid receptors is evident in isolated guinea pig ileum preparations in which alvimopan competitively antagonizes the effects of morphine on contractility. Alvimopan achieves this selective gastrointestinal opioid antagonism without reversing the central analgesic effects of μ-opioid agonists.
12.2. Pharmacodynamics
In an exploratory study in healthy subjects, alvimopan 12 mg administered twice a day reduced the delay in small and large bowel transit induced by codeine 30 mg administered 4 times a day, as measured by gastrointestinal scintigraphy. In the same study, concomitant alvimopan did not reduce the delay in gastric emptying induced by codeine.
Cardiac Electrophysiology
At a dosage of 24 mg twice daily (two times the approved recommended dosage) for 7 days, ENTEREG does not prolong the QT interval to any clinically relevant extent. The potential for QTc effects at higher doses has not been studied.
12.3. Pharmacokinetics
Following oral administration of alvimopan, an amide hydrolysis compound is present in the systemic circulation, which is considered a product exclusively of intestinal flora metabolism. This compound is referred to as the ‘metabolite’. It is also a mu-opioid receptor antagonist with a Ki of 0.8 nM (0.3 ng/mL).
Absorption
Following oral administration of ENTEREG capsules in healthy plasma subjects, the alvimopan concentration peaked at approximately 2 hours post-dose. No significant accumulation in the concentration of alvimopan was observed following twice daily dosing. The mean peak plasma concentration was 10.98 (±6.43) ng/mL and mean AUC0–12h was 40.2 (±22.5) ng∙h/mL after dosing of alvimopan at 12 mg twice daily for 5 days. The absolute bioavailability was estimated to be 6% (range, 1% to 19%). There was a delay in the appearance of the ‘metabolite’, which had a median Tmax of 36 hours following administration of a single dose of alvimopan. Concentrations of the ‘metabolite’ were highly variable between subjects and within a subject. The ‘metabolite’ accumulated after multiple doses of ENTEREG. The mean Cmax for the ‘metabolite’ after alvimopan 12 mg twice daily for 5 days was 35.73 ± 35.29 ng/mL.
Concentrations of alvimopan and its ‘metabolite’ are higher (approximately 1.9-fold and 1.4-fold, respectively) in postoperative ileus patients than in healthy subjects.
Effect of Food: A high-fat meal decreased the extent and rate of alvimopan absorption. The Cmax and AUC were decreased by approximately 38% and 21%, respectively, and the Tmax was prolonged by approximately 1 hour. The clinical significance of this decreased bioavailability is unknown. In postoperative ileus clinical trials, the preoperative dose of ENTEREG was administered in a fasting state. Subsequent doses were given without regard to meals.
Distribution
The steady-state volume of distribution of alvimopan was estimated to be 30±10 L. Plasma protein binding of alvimopan and its ‘metabolite’ was independent of concentration over ranges observed clinically and averaged 80% and 94%, respectively. Both alvimopan and the ‘metabolite’ were bound to albumin and not to alpha-1 acid glycoprotein.
Elimination
Metabolism and Excretion: In vitro data suggest that alvimopan is not a substrate of CYP enzymes. The average plasma clearance for alvimopan was 402 (±89) mL/min. Renal excretion accounted for approximately 35% of total clearance. There was no evidence that hepatic metabolism was a significant route for alvimopan elimination. Biliary secretion was considered the primary pathway for alvimopan elimination. Unabsorbed drug and unchanged alvimopan resulting from biliary excretion were then hydrolyzed to its ‘metabolite’ by gut microflora. The ‘metabolite’ was eliminated in the feces and in the urine as unchanged ‘metabolite’, the glucuronide conjugate of the ‘metabolite’, and other minor metabolites. The mean terminal phase half-life of alvimopan after multiple oral doses of ENTEREG ranged from 10 to 17 hours. The terminal half-life of the ‘metabolite’ ranged from 10 to 18 hours.
Specific Populations
Geriatric Patients: The pharmacokinetics of alvimopan, but not its ‘metabolite’, were related to age, but this effect was not clinically significant and does not warrant dosage adjustment based on increased age.
Racial or Ethnic Groups: The pharmacokinetic characteristics of alvimopan were not affected by Hispanic or Black race. Plasma ‘metabolite’ concentrations were lower in Black and Hispanic patients (by 43% and 82%, respectively) than in Caucasian patients following alvimopan administration. These changes are not considered to be clinically significant in surgical patients. Japanese healthy male subjects had an approximately 2-fold increase in plasma alvimopan concentrations, but no change in ‘metabolite’ pharmacokinetics. The pharmacokinetics of alvimopan have not been studied in subjects of other East Asian ancestry. Dosage adjustment in Japanese patients is not required [see Use in Specific Populations (8.8)].
Male and Female Patients: There was no effect of sex on the pharmacokinetics of alvimopan or the ‘metabolite’.
Patients with Hepatic Impairment: Exposure to alvimopan following a single 12 mg dose tended to be higher (1.5- to 2-fold, on average) in patients with mild or moderate hepatic impairment (as defined by Child-Pugh Class A and B, n = 8 each) compared with healthy controls (n = 4). There were no consistent effects on the Cmax or half-life of alvimopan in patients with hepatic impairment. However, 2 of 16 patients with mild-to-moderate hepatic impairment had longer than expected half-lives of alvimopan, indicating that some accumulation may occur upon multiple dosing. The Cmax of the ‘metabolite’ tended to be more variable in patients with mild or moderate hepatic impairment than in matched normal subjects. A study of 3 patients with severe hepatic impairment (Child-Pugh Class C), indicated similar alvimopan exposure in 2 patients and an approximately 10-fold increase in Cmax and exposure in 1 patient with severe hepatic impairment when compared with healthy controls [see Warnings and Precautions (5.4), Use in Specific Populations (8.6)].
Patients with Renal Impairment: There was no relationship between renal function (i.e., creatinine clearance [CrCl]) and plasma alvimopan pharmacokinetics (Cmax, AUC, or half-life) in patients with mild (CrCl 51–80 mL/min), moderate (CrCl 31–50 mL/min), or severe (CrCl less than 30 mL/min) renal impairment (n = 6 each). Renal clearance of alvimopan was related to renal function; however, because renal clearance was only a small fraction (35%) of the total clearance, renal impairment had a small effect on the apparent oral clearance of alvimopan. The half-lives of alvimopan were comparable in the mild, moderate, and control renal impairment groups but longer in the severe renal impairment group. Exposure to the ‘metabolite’ tended to be 2- to 5-fold higher in patients with moderate or severe renal impairment compared with patients with mild renal impairment or control subjects. Thus, there may be accumulation of alvimopan and ‘metabolite’ in patients with severe renal impairment receiving multiple doses of ENTEREG. Patients with end-stage renal disease were not studied [see Warnings and Precautions (5.5), Use in Specific Populations (8.7)].
Patients with Crohn’s Disease: There was no relationship between disease activity in patients with Crohn’s disease (measured as Crohn’s Disease Activity Index or bowel movement frequency) and alvimopan pharmacokinetics (AUC or Cmax). Patients with active or quiescent Crohn’s disease had increased variability in alvimopan pharmacokinetics, and exposure tended to be 2-fold higher in patients with quiescent disease than in those with active disease or in normal subjects. Concentrations of the ‘metabolite’ were lower in patients with Crohn’s disease.
Drug Interaction Studies
Potential for Drugs to Affect Alvimopan Pharmacokinetics: Concomitant administration of ENTEREG with inducers or inhibitors of CYP enzymes is unlikely to alter the metabolism of alvimopan because ENTEREG is metabolized mainly by non-CYP enzyme pathway. No clinical studies have been performed to assess the effect of concomitant administration of inducers or inhibitors of cytochrome P450 enzymes on alvimopan pharmacokinetics.
In vitro studies suggest that alvimopan and its ‘metabolite’ are substrates for p-glycoprotein. A population pharmacokinetic analysis did not reveal any evidence that alvimopan or ‘metabolite’ pharmacokinetics were influenced by concomitant medications that are mild-to-moderate p-glycoprotein inhibitors. No clinical studies of concomitant administration of alvimopan and strong inhibitors of p-glycoprotein (e.g., verapamil, cyclosporine, amiodarone, itraconazole, quinine, spironolactone, quinidine, diltiazem, bepridil) have been conducted.
A population pharmacokinetic analysis suggests that the pharmacokinetics of alvimopan were not affected by concomitant administration of acid blockers or antibiotics. However, plasma concentrations of the ‘metabolite’ were lower in patients receiving acid blockers or preoperative oral antibiotics (49% and 81%, respectively). No dosage adjustments are necessary in these patients.
Potential for Alvimopan to Affect the Pharmacokinetics of Other Drugs: Alvimopan and its ‘metabolite’ are not inhibitors of CYP 1A2, 2C9, 2C19, 3A4, 2D6, and 2E1 in vitro at concentrations far in excess of those observed clinically.
Alvimopan and its ‘metabolite’ are not inducers of CYP 1A2, 2B6, 2C9, 2C19, and 3A4.
In vitro studies also suggest that alvimopan and its ‘metabolite’ are not inhibitors of p-glycoprotein.
These in vitro findings suggest that ENTEREG is unlikely to alter the pharmacokinetics of coadministered drugs through inhibition or induction of CYP enzymes or inhibition of p-glycoprotein.
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Two-year carcinogenicity studies were conducted with alvimopan in CD-1 mice at oral doses up to 4000 mg/kg/day and in Sprague Dawley rats at oral doses up to 500 mg/kg/day. Oral administration of alvimopan for 104 weeks produced significant increases in the incidences of fibroma, fibrosarcoma, and sarcoma in the skin/subcutis, and of osteoma/osteosarcoma in bones of female mice at 4000 mg/kg/day (about 674 times the recommended human dose based on body surface area). In rats, oral administration of alvimopan for 104 weeks did not produce any tumor up to 500 mg/kg/day (about 166 times the recommended human dose based on body surface area).
Mutagenesis
Alvimopan was not genotoxic in the Ames test, the mouse lymphoma cell (L5178Y/TK +/−) forward mutation test, the Chinese Hamster Ovary (CHO) cell chromosome aberration test, or the mouse micronucleus test. The pharmacologically active ‘metabolite’ was negative in the Ames test, chromosome aberration test in CHO cells, and mouse micronucleus test.
Impairment of Fertility
Alvimopan at intravenous doses up to 10 mg/kg/day (about 3.4 to 6.8 times the recommended human oral dose based on body surface area) was found to have no adverse effect on fertility and reproductive performance of male or female rats.
14. Clinical Studies
The efficacy of ENTEREG in the management of postoperative ileus was evaluated in 6 multicenter, randomized, double-blind, parallel-group, placebo-controlled studies: 5 US studies (Studies 1-4 and 6) and 1 non–US study (Study 5). Patients 18 years of age or older undergoing partial large or small bowel resection surgery with primary anastomosis for colorectal or small bowel disease, total abdominal hysterectomy, or radical cystectomy for bladder cancer (in this procedure, resected segments of bowel are used for reconstruction of the urinary tract) under general anesthesia were randomly assigned to receive oral doses of ENTEREG 12 mg or matching placebo. The initial dose was administered at least 30 minutes and up to 5 hours prior to the scheduled start of surgery for most patients, and subsequent doses were administered twice daily beginning on the first postoperative day and continued until hospital discharge or a maximum of 7 days. There were no limitations on the type of general anesthesia used, but intrathecal or epidural opioids or anesthetics were prohibited.
All patients in the US studies were scheduled to receive intravenous patient-controlled opioid analgesia. In the non–US study, patients were scheduled to receive opioids either by intravenous patient-controlled opioid analgesia or bolus parenteral administration (intravenous or intramuscular). In all studies, there was no restriction on the type of opioid used or the duration of intravenous patient-controlled opioid analgesia. A standardized accelerated postoperative care pathway was implemented: early nasogastric tube removal (before the first postoperative dose); early ambulation (day following surgery); early diet advancement (liquids offered the day following surgery for patients undergoing bowel resection and by the third day following surgery for patients undergoing radical cystectomy; solids by the second day following surgery for patients undergoing bowel resection and by the fourth day following surgery for patients undergoing radical cystectomy), as tolerated.
Patients who received more than 3 doses of an opioid (regardless of route) during the 7 days prior to surgery and patients with complete bowel obstruction or who were scheduled for a total colectomy, colostomy, or ileostomy were excluded.
The primary endpoint for all studies was time to achieve resolution of postoperative ileus, a clinically defined composite measure of both upper and lower gastrointestinal recovery. Although both 2-component (GI2: toleration of solid food and first bowel movement) and 3-component (GI3: toleration of solid food and either first flatus or bowel movement) endpoints were used in all studies, GI2 is presented as it represents the most objective and clinically relevant measure of treatment response in patients undergoing surgeries that include a bowel resection. The time from the end of surgery to when the discharge order was written represented the length of hospital stay. In the 6 studies, 1,058 patients who underwent a surgery that included a bowel resection received placebo (not including 157 for total abdominal hysterectomy) and 1,096 patients received ENTEREG 12 mg (not including 143 for total abdominal hysterectomy).
The efficacy of ENTEREG following total abdominal hysterectomy has not been established. Therefore, the following data are presented only for surgeries that included a bowel resection (i.e., bowel resection or radical cystectomy).
Bowel Resection or Radical Cystectomy: A total of 2,154 patients underwent a surgery that included a bowel resection. The average age was 62 years, 54% were males, and 89% were Caucasian. The most common indications for surgery were colon or rectal cancer/malignancy, bladder cancer, and diverticular disease. In the non–US bowel resection study (Study 5), average daily postoperative opioid consumption was approximately 50% lower and the use of non-opioid analgesics substantially higher, as compared with the US bowel resection studies (Studies 1-4) for both treatment groups. During the first 48 hours postoperatively, the use of non-opioid analgesics was 69% compared with 4% for the non–US and US bowel resection studies, respectively. In each of the 6 studies, ENTEREG accelerated the time to recovery of gastrointestinal function, as measured by the composite endpoint GI2, and time to discharge order written as compared with placebo. Hazard ratios greater than 1 indicate a higher probability of achieving the event during the study period with treatment with ENTEREG than with placebo. Table 1 provides the Hazard Ratios, Kaplan Meier means, medians, and mean and median treatment differences (hours) in gastrointestinal recovery between ENTEREG and placebo.
Table 1: GI2 Recovery (Hours) in Bowel Resection Patients
| Study No.* | ENTEREG 12 mg | Placebo | Treatment Difference | Hazard Ratio (95% CI) | |||
|---|---|---|---|---|---|---|---|
| Mean† | Median | Mean†? | Median | Means† | Medians | ||
| 1 | 92.0 | 80.0 | 111.8 | 96.6 | 19.8 | 16.6 | 1.533 (1.293, 1.816) |
| 2 | 105.9 | 98.0 | 132.0 | 115.2 | 26.1 | 17.2 | 1.625 (1.256, 2.102) |
| 3 | 116.4 | 101.8 | 130.3 | 116.8 | 14.0 | 15.0 | 1.365 (1.057, 1.764) |
| 4 | 106.7 | 101.4 | 119.9 | 113.3 | 13.2 | 11.9 | 1.400 (1.035, 1.894) |
| 5 | 98.2 | 92.8 | 108.8 | 95.9 | 10.6 | 3.1 | 1.299 (1.070, 1.575) |
| 6 | 132.7 | 117.0 | 164.2 | 145.6 | 31.5 | 28.5 | 1.773 (1.359, 2.311) |
* Study 1 = 14CL314 ; Study 2 = 14CL313; Study 3 = 14CL308; Study 4 = 14CL302; Study 5 = SB-767905/001; Study 6 = 14CL4 03
† The estimates of the means and differences of treatment means are biased because of the censoring of events not achieved prior to the end of the observation period (10 days). The estimates of the differences of treatment means are likely to be underestimates.
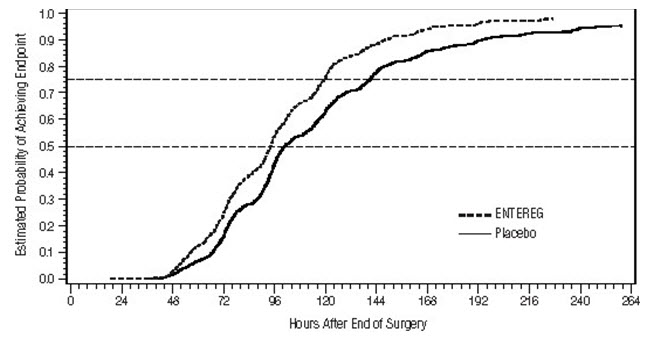
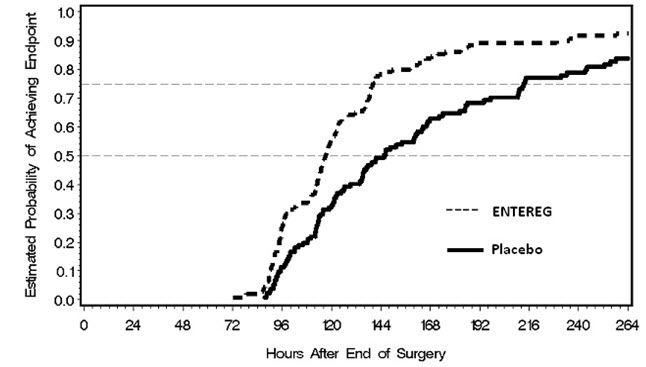
The Kaplan Meier estimate probabilities of patients receiving ENTEREG who achieved GI2 were numerically higher at all times throughout the study observation period compared with those of patients receiving placebo (see Figures 1 and 2).
Figure 1. Time to GI2 Based on Results from Studies 1 through 5:
Figure 2: Time to GI2 Based on Results from Study 6:
In Studies 1-4, the differences between ENTEREG and placebo patient groups in median time to ‘discharge order written’ ranged from 6 to 22 hours, in favor of ENTEREG patients. The group differences in mean time to ‘discharge order written’ ranged from 13 to 21 hours. In Study 6, the median time difference was 19 hours in favor of ENTEREG patients (mean time difference 22 hours).
ENTEREG did not reverse opioid analgesia as measured by visual analog scale pain intensity scores and/or amount of postoperative opioids administered across all 6 studies.
There were no sex-, age-, or race-related differences in treatment effect.
The incidence of anastomotic leak was low and comparable in patients receiving either ENTEREG or placebo (0.7% and 1.0%, respectively).
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.