VIMOVO Delayed release tablet Ref.[50562] Active ingredients: Esomeprazole Naproxen
Source: FDA, National Drug Code (US) Revision Year: 2022
12.1. Mechanism of Action
VIMOVO consists of an immediate-release esomeprazole magnesium layer and an enteric-coated naproxen core. As a result, esomeprazole is released first in the stomach, prior to the dissolution of naproxen in the small intestine. The enteric coating prevents naproxen release at pH levels below 5.5.
The mechanism of action of the naproxen anion, like that of other NSAIDs, is not completely understood but inhibition of cyclooxygenase (COX-1 and COX-2).
VIMOVO has analgesic, anti-inflammatory, and antipyretic properties contributed by the naproxen component. Naproxen is a potent inhibitor of prostaglandin synthesis in vitro. Naproxen concentrations reached during therapy have produced in vivo effects. Prostaglandins sensitize afferent nerves and potentiate the action of bradykinin in inducing pain in animal models. Prostaglandins are mediators of inflammation. Because naproxen is an inhibitor of prostaglandin synthesis, its mode of action may be due to an increase of prostaglandins in peripheral tissues.
Esomeprazole is a proton pump inhibitor that suppresses gastric acid secretion by specific inhibition of the H+ / K+ - ATPase in the gastric parietal cell. Esomeprazole is protonated and converted in the acidic compartment of the parietal cell forming the active inhibitor, the achiral sulphenamide. By acting specifically on the proton pump, esomeprazole blocks the final step in acid production, thus reducing gastric acidity. This effect is dose-related up to a daily dose of 20 to 40 mg and leads to inhibition of gastric acid secretion.
12.2. Pharmacodynamics
Interaction with Aspirin
In a healthy volunteer study, 10 days of concomitant administration of naproxen 220 mg once-daily with low-dose immediate-release aspirin (81 mg) showed an interaction with the antiplatelet activity of aspirin as measured by % serum thromboxane B2 inhibition at 24 hours following the day 10 dose [98.7% (aspirin alone) vs 93.1% (naproxen and aspirin)]. The interaction was observed even following discontinuation of naproxen on day 11 (while aspirin dose was continued) but normalized by day 13. In the same study, the interaction was greater when naproxen was administered 30 minutes prior to aspirin [98.7% vs 87.7%] and minimal when aspirin was administered 30 minutes prior to naproxen [98.7% vs 95.4%].
Following administration of naproxen 220 mg twice-daily with low-dose immediate-release aspirin (first naproxen dose given 30 minutes prior to aspirin), the interaction was minimal at 24 h following day 10 dose [98.7% vs 95.7%]. However, the interaction was more prominent after discontinuation of naproxen (washout) on day 11 [98.7% vs 84.3%] and did not normalize completely by day 13 [98.5% vs 90.7%] [see Drug Interactions (7)].
Antisecretory Activity
The effect of VIMOVO on intragastric pH was determined in 25 healthy volunteers in one study. Three VIMOVO combinations (naproxen 500 mg combined with either esomeprazole 10, 20, or 30 mg) were administered twice daily over 9 days. The results are shown in the following table:
Table 5. Effect on Intragastric pH on Day 9 (N=25):
| Naproxen 500 mg combined with esomeprazole | |||
|---|---|---|---|
| 10 mg | 20 mg | 30 mg | |
| % Time Gastric pH >4* | 41.1 (3.0) | 71.5 (3.0) | 76.8 (3.0) |
| Coefficient of variation | 55% | 18% | 16% |
LS Mean (SE)
Serum Gastrin Effects
The effect of esomeprazole on serum gastrin concentrations was evaluated in approximately 2,700 patients in clinical trials up to 8 weeks and in over 1,300 patients for up to 6-12 months.
The mean fasting gastrin level increased in a dose-related manner. This increase reached a plateau within two to three months of therapy and returned to baseline levels within four weeks after discontinuation of therapy.
Increased gastrin causes enterochromaffin-like cell hyperplasia and increased serum Chromogranin A (CgA) levels. The increased CgA levels may cause false positive results in diagnostic investigations for neuroendocrine tumors. Healthcare providers should temporarily stop esomeprazole treatment at least 14 days before assessing CgA levels and consider repeating the test if initial CgA levels are high.
Enterochromaffin-like (ECL) Cell Effects
In over 1,000 patients treated with esomeprazole (10, 20 or 40 mg/day) up to 6-12 months, the prevalence of ECL cell hyperplasia increased with time and dose. No patient developed ECL cell carcinoids, dysplasia, or neoplasia in the gastric mucosa.
Endocrine Effects
Esomeprazole had no effect on thyroid function when given in oral doses of 20 or 40 mg for 4 weeks. Other effects of esomeprazole on the endocrine system were assessed using omeprazole studies. Omeprazole given in oral doses of 30 or 40 mg for 2 to 4 weeks had no effect on carbohydrate metabolism, circulating levels of parathyroid hormone, cortisol, estradiol, testosterone, prolactin, cholecystokinin or secretin.
Effects on Gastrointestinal Microbial Ecology
Decreased gastric acidity due to any means including proton pump inhibitors, increases gastric counts of bacteria normally present in the gastrointestinal tract. Treatment with proton pump inhibitors may lead to slightly increased risk of gastrointestinal infections such as Salmonella and Campylobacter and, in hospitalized patients, possibly also Clostridium difficile.
12.3. Pharmacokinetics
Absorption
Naproxen
At steady state following administration of VIMOVO twice daily, peak plasma concentrations of naproxen are reached on average 3 hours following both the morning and the evening dose.
Bioequivalence between VIMOVO and enteric-coated naproxen, based on both area under the plasma concentration-time curve (AUC) and maximum plasma concentration (Cmax) of naproxen, has been demonstrated for both the 375 mg and 500 mg doses.
Naproxen is absorbed from the gastrointestinal tract with an in vivo bioavailability of 95%.
Steady-state levels of naproxen are reached in 4 to 5 days.
Esomeprazole
Following administration of VIMOVO twice daily, esomeprazole is rapidly absorbed with peak plasma concentration reached within on average, 0.43 to 1.2 hours, following the morning and evening dose on both the first day of administration and at steady state. The peak plasma concentrations of esomeprazole are higher at steady state compared to on first day of dosing of VIMOVO.
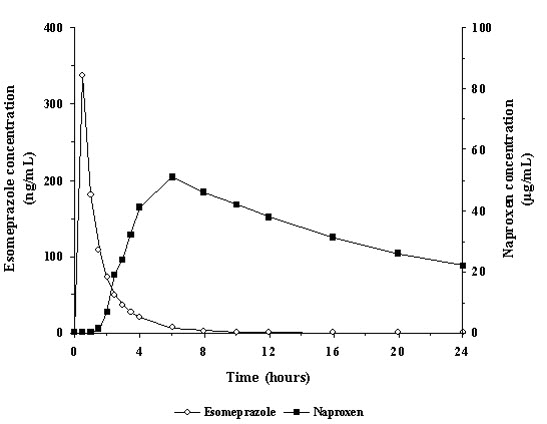
Figure 1 represents the pharmacokinetics of naproxen and esomeprazole following administration of VIMOVO 500 mg/20 mg.
Figure 1. Mean plasma concentrations of naproxen and esomeprazole following single dose administration of VIMOVO (500mg/20 mg):
Food Effect
Administration of VIMOVO together with high-fat food in healthy volunteers does not affect the extent of absorption of naproxen but significantly prolongs tmax by 10 hours and decreases peak plasma concentration (Cmax) by about 12%.
Administration of VIMOVO together with high-fat food in healthy volunteers delays tmax of esomeprazole by 1 hour and significantly reduces the extent of absorption, resulting in 52% and 75% reductions of area under the plasma concentration versus time curve (AUC) and peak plasma concentration (Cmax), respectively.
Administration of VIMOVO 30 minutes before high-fat food intake in healthy volunteers does not affect the extent of absorption of naproxen but delays the absorption by about 4 hours and decreases peak plasma concentration (Cmax) by about 17%, but has no significant effect on the rate or extent of esomeprazole absorption compared to administration under fasted conditions [see Dosage and Administration (2)].
Administration of VIMOVO 60 minutes before high-fat food intake in healthy volunteers has no effect on the rate and extent of naproxen absorption; however, increases the esomeprazole AUC by 25% and Cmax by 50% compared to administration under fasted conditions. This increase in esomeprazole Cmax does not raise a safety issue since the approved dosing regimen of esomeprazole at 40 mg QD would result in higher Cmax [see Dosage and Administration (2)].
Therefore, VIMOVO should be taken at least 30 minutes before the meal.
Distribution
Naproxen
Naproxen has a volume of distribution of 0.16 L/kg. At therapeutic levels naproxen is greater than 99% albumin-bound. At doses of naproxen greater than 500 mg/day there is less than proportional increase in plasma levels due to an increase in clearance caused by saturation of plasma protein binding at higher doses (average trough Css 36.5, 49.2 and 56.4 mg/L with 500, 1000 and 1500 mg daily doses of naproxen, respectively). The naproxen anion has been found in the milk of lactating women at a concentration equivalent to approximately 1% of maximum naproxen concentration in plasma [see Use in Specific Populations (8.2)].
Esomeprazole
The apparent volume of distribution at steady state in healthy subjects is approximately 16L. Esomeprazole is 97% plasma protein bound.
Elimination
Metabolism
Naproxen:
Naproxen is extensively metabolized in the liver by the cytochrome P450 system (CYP), CYP2C9 and CYP1A2, to 6-0-desmethyl naproxen. Neither the parent drug nor the metabolites induce metabolizing enzymes. Both naproxen and 6-0-desmethyl naproxen are further metabolized to their respective acylglucuronide conjugated metabolites. Consistent with the half- life of naproxen, the area under the plasma concentration time curve increases with repeated dosing of VIMOVO twice daily.
Esomeprazole:
Esomeprazole is extensively metabolized in the liver by the CYP enzyme system. The major part of the metabolism of esomeprazole is dependent on the polymorphic CYP2C19, responsible for the formation of the hydroxyl- and desmethyl metabolites of esomeprazole. The remaining part is dependent on another specific isoform CYP3A4, responsible for the formation of esomeprazole sulphone, the main metabolite in plasma. The major metabolites of esomeprazole have no effect on gastric acid secretion.
The area under the plasma esomeprazole concentration-time curve increases with repeated administration of VIMOVO. This increase is dose-dependent and results in a non-linear dose-AUC relationship after repeated administration. An increased absorption of esomeprazole with repeated administration of VIMOVO probably also contributes to the time-and dose-dependency.
Excretion
Naproxen:
Following administration of VIMOVO twice daily, the mean elimination half-life for naproxen is approximately 15 hours following the evening dose, with no change with repeated dosing.
The clearance of naproxen is 0.13 mL/min/kg. Approximately 95% of the naproxen from any dose is excreted in the urine, primarily as naproxen (<1%), 6-0-desmethyl naproxen (<1%) or their conjugates (66% to 92%). Small amounts, 3% or less of the administered dose, are excreted in the feces. In patients with renal failure, metabolites may accumulate [see Warnings and Precautions (5.6)].
Esomeprazole:
Following administration of VIMOVO twice daily, the mean elimination half-life of esomeprazole is approximately 1 hour following both the morning and evening dose on day 1, with a slightly longer elimination half-life at steady state (1.2-1.5 hours).
Almost 80% of an oral dose of esomeprazole is excreted as metabolites in the urine, the remainder in the feces. Less than 1% of the parent drug is found in the urine.
Specific Populations
Geriatric Patients
There is no specific data on the pharmacokinetics of VIMOVO in patients over age 65.
Studies indicate that although total plasma concentration of naproxen is unchanged, the unbound plasma fraction of naproxen is increased in the elderly, although the unbound fraction is <1% of the total naproxen concentration. Unbound trough naproxen concentrations in elderly subjects have been reported to range from 0.12% to 0.19% of total naproxen concentration, compared with 0.05% to 0.075% in younger subjects. The clinical significance of this finding is unclear, although it is possible that the increase in free naproxen concentration could be associated with an increase in the rate of adverse events per a given dosage in some elderly patients [see Adverse Reactions (6) and Use in Specific Populations (8.5)].
The AUC and Cmax values of esomeprazole were slightly higher (25% and 18%, respectively) in the elderly as compared to younger subjects at steady state. Dosage adjustment for the esomeprazole component based on age is not necessary.
Male and Female Patients
The AUC and Cmax values of esomeprazole were slightly higher (13%) in females than in males at steady state. Dosage adjustment for the esomeprazole component based on gender is not necessary.
Racial or Ethnic Groups
Pharmacokinetic differences due to race have not been studied for naproxen.
Approximately 3% of Caucasians and 15 to 20% of Asians lack a functional CYP2C19 enzyme and are called poor metabolizers. In these individuals the metabolism of esomeprazole is probably mainly catalyzed by CYP3A4. After repeated once-daily administration of 40 mg esomeprazole, the mean area under the plasma concentration-time curve was approximately 100% higher in poor metabolizers than in subjects having a functional CYP2C19 enzyme (extensive metabolizers).
Patients with Renal Impairment
The pharmacokinetics of VIMOVO or naproxen have not been determined in subjects with renal impairment.
Given that naproxen, its metabolites and conjugates are primarily excreted by the kidney, the potential exists for naproxen metabolites to accumulate in the presence of renal impairment. Elimination of naproxen is decreased in patients with severe renal impairment. Naproxen- containing products, including VIMOVO, is not recommended for use in patients with moderate to severe and severe renal impairment (creatinine clearance <30 ml/min) [see Dosage and Administration (2), Warnings and Precautions (5.6), Use in Specific Populations (8.7)].
No studies have been performed with esomeprazole in patients with decreased renal function. Since the kidney is responsible for the excretion of the metabolites of esomeprazole but not for the elimination of the parent compound, the metabolism of esomeprazole is not expected to be changed in patients with impaired renal function.
Patients with Hepatic Impairment
The pharmacokinetics of VIMOVO or naproxen have not been determined in subjects with hepatic impairment.
In patients with severe hepatic impairment, VIMOVO should be avoided due to increase of risk of NSAID associated bleeding and/or renal failure associated with naproxen.
Chronic alcoholic liver disease and probably also other forms of cirrhosis reduce the total plasma concentration of naproxen, but the plasma concentration of unbound naproxen is increased. The implication of this finding for the naproxen component of VIMOVO dosing is unknown but it is prudent to use the lowest effective dose.
The AUCs of esomeprazole in patients with severe hepatic impairment (Child Pugh Class C) have been shown to be 2-3 times higher than in patients with normal liver function. For this reason, it has been recommended that esomeprazole doses not exceed 20 mg daily in patients with severe hepatic impairment. However, there is no dose adjustment necessary for patients with Child Pugh Class A and B for the esomeprazole component of VIMOVO. There is no VIMOVO dosage form that contains less than 20 mg esomeprazole for twice daily dosing [see Dosage and Administration (2), Warnings and Precautions (5.3)].
Drug Interaction Studies
Effect of Naproxen on Other Drugs
Aspirin:
When NSAIDs were administered with aspirin, the protein binding of NSAIDs were reduced, although the clearance of free NSAID was not altered. The clinical significance of this interaction is not known. See Table 3 for clinically significant drug interactions of NSAIDs with aspirin [see Drug Interactions (7)].
Effect of Esomeprazole on Other Drugs
Cytochrome P 450 Interactions:
Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. In vitro and in vivo studies have shown that esomeprazole is not likely to inhibit CYPs 1A2, 2A6, 2C9, 2D6, 2E1 and 3A4. No clinically relevant interactions with drugs metabolized by these CYP enzymes would be expected. Drug interaction studies have shown that esomeprazole does not have any clinically significant interactions with phenytoin, warfarin, quinidine, clarithromycin or amoxicillin.
Clopidogrel: Results from a crossover study in healthy subjects have shown a pharmacokinetic interaction between clopidogrel (300 mg loading dose/75 mg daily maintenance dose) and esomeprazole (40 mg p.o. once daily) when co-administered for 30 days. Exposure to the active metabolite of clopidogrel was reduced by 35% to 40% over this time period. Pharmacodynamic parameters were also measured and demonstrated that the change in inhibition of platelet aggregation was related to the change in the exposure to clopidogrel active metabolite [see Warnings and Precautions (5.22), Drug Interactions (7)].
Mycophenolate Mofetil: Administration of omeprazole 20 mg twice daily for 4 days and a single 1000 mg dose of MMF approximately one hour after the last dose of omeprazole to 12 healthy subjects in a cross-over study resulted in a 52% reduction in the Cmax and 23% reduction in the AUC of MPA [see Drug Interactions (7)].
Cilostazol: Omeprazole acts as an inhibitor of CYP2C19. Omeprazole, given in doses of 40 mg daily for one week to 20 healthy subjects in cross-over study, increased Cmax and AUC of cilostazol by 18% and 26% respectively. Cmax and AUC of one of its active metabolites, 3,4- dihydrocilostazol, which has 4-7 times the activity of cilostazol, were increased by 29% and 69% respectively [see Drug Interactions (7)].
Nelfinavir: Following multiple doses of nelfinavir (1250 mg, twice daily) and omeprazole (40 mg once a day), AUC was decreased by 36% and 92%, Cmax by 37% and 89% and Cmin by 39% and 75% respectively for nelfinavir and main oxidative metabolite, hydroxy-t-butylamide (M8) [see Drug Interactions (7)].
Atazanavir: Following multiple doses of atazanavir (400 mg, once a day) and omeprazole (40 mg, once a day, 2 hr before atazanavir), AUC was decreased by 94%, Cmax by 96%, and Cmin by 95% [see Drug Interactions (7)].
Saquinavir: Elevated serum levels have been reported with an increase in AUC by 82% in Cmax by 75% and in Cmin by 106% following multiple dosing of saquinavir/ritonavir (1000/100 mg) twice a day for 15 days with omeprazole 40 mg once a day co-administered on days 11 to 15 [see Drug Interactions (7)].
Diazepam: Co-administration of esomeprazole 30 mg and diazepam, a CYP2C19 substrate, resulted in a 45% decrease in clearance of diazepam [see Drug Interactions (7)].
Digoxin: Concomitant administration of omeprazole 20 mg once daily and digoxin in healthy subjects increased the bioavailability of digoxin by 10% (30% in two subjects) [see Drug Interactions (7)].
Effect of Other Drugs on Esomeprazole
Because esomeprazole is metabolized by CYP2C19 and CYP3A4, inducers and inhibitors of these enzymes may potentially alter exposure of esomeprazole.
St. John's Wort: In a cross-over study in 12 healthy male subjects, St. John's Wort (300 mg three times daily for 14 days) significantly decreased the systemic exposure of omeprazole in CYP2C19 poor metabolizers (Cmax and AUC decreased by 37.5% and 37.9%, respectively) and extensive metabolizers (Cmax and AUC decreased by 49.6% and 43.9%, respectively) [see Warnings and Precautions (5.25), Drug Interactions (7)].
Voriconazole: Concomitant administration of omeprazole and voriconazole (a combined inhibitor of CYP2C19 and CYP3A4) resulted in more than doubling of the omeprazole exposure. When voriconazole (400 mg every 12 hours for one day, followed by 200 mg once daily for 6 days) was given with omeprazole (40 mg once daily for 7 days) to healthy subjects, the steady-state Cmax and AUC0-24 of omeprazole significantly increased: an average of 2 times (90% CI: 1.8, 2.6) and 4 times (90% CI: 3.3, 4.4), respectively, as compared to when omeprazole was given without voriconazole [see Drug Interactions (7)].
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Naproxen
A 2-year study was performed in rats to evaluate the carcinogenic potential of naproxen at rat doses of 8, 16, and 24 mg/kg/day (0.05, 0.1, and 0.16 times the maximum recommended human daily dose of 1500 mg/day based on a body surface area comparison). The maximum dose used was 0.28 times the highest recommended human dose. No evidence of tumorigenicity was found.
Esomeprazole
The carcinogenic potential of esomeprazole was assessed using omeprazole studies, of which esomeprazole is an enantiomer. In two 24-month oral carcinogenicity studies in rats, omeprazole at daily doses of 1.7, 3.4, 13.8, 44 and 140.8 mg/kg/day (about 0.41 to 34.2 times the human dose of 40 mg/day expressed on a body surface area basis) produced gastric ECL cell carcinoids in a dose-related manner in both male and female rats; the incidence of this effect was markedly higher in female rats, which had higher blood levels of omeprazole. Gastric carcinoids seldom occur in the untreated rat. In addition, ECL cell hyperplasia was present in all treated groups of both sexes. In one of these studies, female rats were treated with 13.8 mg omeprazole/kg/day (about 3.36 times the human dose of 40 mg/day on a body surface area basis) for 1 year, then followed for an additional year without the drug. No carcinoids were seen in these rats. An increased incidence of treatment-related ECL cell hyperplasia was observed at the end of 1 year (94% treated vs 10% controls). By the second year the difference between treated and control rats was much smaller (46% vs 26%) but still showed more hyperplasia in the treated group. Gastric adenocarcinoma was seen in one rat (2%). No similar tumor was seen in male or female rats treated for 2 years. For this strain of rat, no similar tumor has been noted historically, but a finding involving only one tumor is difficult to interpret. A 78-week mouse carcinogenicity study of omeprazole did not show increased tumor occurrence, but the study was not conclusive.
Mutagenesis
Esomeprazole was negative in the Ames mutation test, in the in vivo rat bone marrow cell chromosome aberration test, and the in vivo mouse micronucleus test. Esomeprazole, however, was positive in the in vitro human lymphocyte chromosome aberration test. Omeprazole was positive in the in vitro human lymphocyte chromosome aberration test, the in vivo mouse bone marrow cell chromosome aberration test, and the in vivo mouse micronucleus test.
Impairment of Fertility
The potential effects of esomeprazole on fertility and reproductive performance were assessed using omeprazole studies. Omeprazole at oral doses up to 138 mg/kg/day in rats (about 33.6 times the human dose of 40 mg/day on a body surface area basis) was found to have no effect on reproductive performance of parental animals.
Studies to evaluate the impact of naproxen on male or female fertility have not been completed.
13.2. Animal Toxicology and/or Pharmacology
Naproxen
Reproduction studies have been performed in rats at 20 mg/kg/day (125 mg/m²/day, 0.23 times the maximum recommended human dose), rabbits at 20 mg/kg/day (220 mg/m²/day, 0.27 times the maximum recommended human dose), and mice at 170 mg/kg/day (510 mg/m²/day, 0.28 times the maximum recommended human dose) with no evidence of impaired fertility or harm to the fetus due to the drug. However, animal reproduction studies are not always predictive of human response.
Esomeprazole – Reproduction Studies
Reproduction studies have been performed in rats at oral doses up to 280 mg/kg/day (about 68 times an oral human dose of 40 mg on a body surface area basis) and in rabbits at oral doses up to 86 mg/kg/day (about 42 times an oral human dose of 40 mg on a body surface area basis) and have revealed no evidence of impaired fertility or harm to the fetus due to esomeprazole [see Use in Specific Populations (8.1)].
Esomeprazole – Juvenile Animal Data
A 28-day toxicity study with a 14-day recovery phase was conducted in juvenile rats with esomeprazole magnesium at doses of 70 to 280 mg/kg/day (about 17 to 68 times a daily oral human dose of 40 mg on a body surface area basis). An increase in the number of deaths at the high dose of 280 mg/kg/day was observed when juvenile rats were administered esomeprazole magnesium from postnatal day 7 through postnatal day 35. In addition, doses equal to or greater than 140 mg/kg/day (about 34 times a daily oral human dose of 40 mg on a body surface area basis), produced treatment-related decreases in body weight (approximately 14%) and body weight gain, decreases in femur weight and femur length, and affected overall growth.
Comparable findings described above have also been observed in this study with another esomeprazole salt, esomeprazole strontium, at equimolar doses of esomeprazole.
14. Clinical Studies
Two randomized, multi-center, double-blind trials (Study 1 and Study 2) compared the incidence of gastric ulcer formation in 428 patients taking VIMOVO and 426 patients taking enteric-coated naproxen. Subjects were at least 18 years of age with a medical condition expected to require daily NSAID therapy for at least 6 months, and, if less than 50 years old, with a documented history of gastric or duodenal ulcer within the past 5 years. The majority of patients were female (67%), white (86%). The majority of patients were 50-69 years of age (83%). Approximately one quarter were on low-dose aspirin.
Studies 1 and 2 showed that VIMOVO given as 500 mg/20 mg twice daily statistically significantly reduced the 6-month cumulative incidence of gastric ulcers compared to enteric-coated naproxen 500 mg twice daily (see Table 6).
Approximately a quarter of the patients in Studies 1 and 2 were taking concurrent low-dose aspirin (≤325 mg daily). The results for this subgroup analysis in patients who used aspirin were consistent with the overall findings of the study.
The results at one month, three months, and six months are presented in Table 6.
Table 6. Cumulative Observed Incidence of Gastric Ulcers at 1, 3 and 6 Months:
| Study 1 | Study 2 | |||
|---|---|---|---|---|
| VIMOVO N=218 number (%) | EC-naproxen N=216 number (%) | VIMOVO N=210 number (%) | EC-naproxen N=210 number (%) | |
| 0-1 Month | 3 (1.4) | 28 (13.0) | 4 (1.9) | 21 (10.0) |
| 0-3 Months | 4 (1.8) | 42 (19.4) | 10 (4.8) | 37 (17.6) |
| 0-6 Months* | 9 (4.1) | 50 (23.1) | 15 (7.1) | 51 (24.3) |
* For both Studies, p<0.001 for treatment comparisons of cumulative GU incidence at six months.
In these trials, patients receiving VIMOVO had a mean duration of therapy of 152 days compared to 124 days in patients receiving enteric-coated naproxen alone. A higher proportion of patients taking EC-naproxen (12%) discontinued the study due to upper GI adverse events (including duodenal ulcers) compared to VIMOVO (4%) in both trials [see Adverse Reactions (6)].
The efficacy of VIMOVO in treating the signs and symptoms of osteoarthritis was established in two 12-week randomized, double-blind, placebo-controlled trials in patients with osteoarthritis (OA) of the knee. In these two trials, patients were allowed to remain on low-dose aspirin for cardioprophylaxis. VIMOVO was given as 500 mg/20 mg twice daily. In each trial, patients receiving VIMOVO had significantly better results compared to patients receiving placebo as measured by change from baseline of the WOMAC pain subscale and the WOMAC physical function subscale and a Patient Global Assessment Score.
Based on studies with enteric-coated naproxen, improvement in patients treated for rheumatoid arthritis was demonstrated by a reduction in joint swelling, a reduction in duration of morning stiffness, a reduction in disease activity as assessed by both the investigator and patient, and by increased mobility as demonstrated by a reduction in walking time. In patients with osteoarthritis, the therapeutic action of naproxen has been shown by a reduction in joint pain or tenderness, an increase in range of motion in knee joints, increased mobility as demonstrated by a reduction in walking time, and improvement in capacity to perform activities of daily living impaired by the disease. In patients with ankylosing spondylitis, naproxen has been shown to decrease night pain, morning stiffness and pain at rest.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.