IBUPAIN FORTE Capsule Ref.[108834] Active ingredients: Codeine Ibuprofen Paracetamol
Source: Health Products Regulatory Authority (ZA) Revision Year: 2023 Publisher: Sandoz SA (Pty) Ltd<sup>1</sup>, Magwa Crescent West, Waterfall City, Jukskei View, Midrand, 2090 1 Company Reg. No.: 1990/001979/07
4.1. Therapeutic indications
IBUPAIN FORTE is indicated for the relief of mild to moderate pain of inflammatory origin with or without fever.
4.2. Posology and method of administration
Posology
DO NOT EXCEED THE RECOMMENDED DOSE.
Undesirable effects may be minimised by using the lowest effective dose for the shortest duration necessary to control symptoms (see section 4.4).
Adults, the elderly and children over 12 years
1 to 2 capsules 6 hourly. Do not take more than 8 capsules in 24 hours.
The duration of treatment should be limited to 5 days and if no effective pain relief is achieved the patients/carers should be advised to seek the views of a medical practitioner.
Hepatic insufficiency and moderate renal insufficiency
In patients with impaired hepatic or renal function or Gilbert’s syndrome, the dose must be reduced or the dosing interval prolonged.
Elderly
The elderly are at increased risk of the serious consequences of adverse reactions. If an NSAID is considered necessary, the lowest effective dose should be used and for the shortest possible duration. The patient should be monitored regularly for gastrointestinal bleeding during NSAID therapy.
Children aged less than 12 years
IBUPAIN FORTE should not be used in children below the age of 12 years because of the risk of opioid toxicity due to the variable and unpredictable metabolism of codeine to morphine (see section 4.3 and section 4.4).
Method of administration
For oral use.
4.9. Overdose
In the event of overdosage or suspected overdose and notwithstanding the fact that the person may be asymptomatic, the nearest doctor, hospital or Poison Centre must be contacted immediately.
Paracetamol
Prompt treatment is essential.
In the event of an overdosage, consult a doctor immediately, or take the person directly to a hospital. A delay in starting treatment may mean that the antidote is given too late to be effective. Evidence of liver damage is often delayed until after the time for effective treatment has lapsed.
Symptoms
Susceptibility to paracetamol toxicity is increased in patients who have taken repeated high doses (greater than 5 to 10 g/day) of paracetamol for several days, in the elderly, young children, in chronic alcoholism, chronic liver disease, AIDS, malnutrition, and with the use of medicines that induce liver microsomal oxidation such as barbiturates, isoniazid, rifampicin, phenytoin and carbamazepine. In these cases, an overdose can be fatal.
In general, symptoms occur within 24 hours: pallor, nausea, vomiting, anorexia and abdominal pain. Mild symptoms during the first two days of acute poisoning do not reflect the potential seriousness of the overdosage.
Liver damage may become apparent 12 to 48 hours, or later after ingestion of paracetamol, initially by elevation of the serum transaminase and lactic dehydrogenase activity, increased serum bilirubin concentrations and prolongation of the prothrombin time. Liver damage may lead to encephalopathy, coma and death.
Acute renal failure with acute tubular necrosis may develop even in the absence of severe liver damage. Abnormalities of glucose metabolism and metabolic acidosis may occur. Cardiac arrhythmias have been reported. Cerebral oedema and nonspecific myocardial depression have occurred.
Treatment of overdose
Although evidence is limited, it is recommended that an adult who has ingested 5 to 10 g or more of paracetamol (or a child who has had more than 140 mg/kg) within the preceding 4 hours, should have the stomach emptied by lavage (emesis may be adequate for children) and a single dose of 50 g activated charcoal given via the lavage tube. Ingestion of amounts of paracetamol smaller than this may require treatment in patients susceptible to paracetamol poisoning (see above). In patients who are stuperose or comatose, endotracheal intubation should precede gastric lavage in order to avoid aspiration.
N-acetylcysteine should be administered to all cases of suspected overdose as soon as possible, preferably within 8 hours of overdosage, although treatment up to 36 hours after ingestion may still be of benefit, especially if more than 150 mg/kg of paracetamol was taken. An initial dose of 150 mg/kg N-acetylcysteine in 200 ml dextrose injection given intravenously over 15 minutes, followed by an infusion of 50 mg/kg in 500 ml dextrose injection over the next 4 hours, and then 100 mg/kg in 1000 ml dextrose injection over the next 16 hours. The volume of intravenous fluid should be modified for children.
Although the oral formulation is not the treatment of choice, 140 mg/kg dissolved in water as a 5% solution may be administered initially, followed by 70 mg/kg every 4 hours for seventeen doses. If activated charcoal is used then it should be removed by gastric lavage as it may interfere with absorption of orally administered N-acetylcysteine and decrease its efficacy.
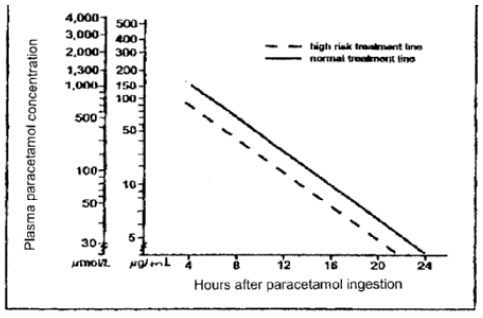
A plasma paracetamol level should be determined 4 hours after ingestion in all cases of suspected overdosage. Levels done before 4 hours may be misleading. Patients at risk of liver damage, and hence requiring continued treatment with N-acetylcysteine, can be identified according to their 4 hour plasma paracetamol level. The plasma paracetamol level can be plotted against time since ingestion in the treatment nomogram. The nomogram should be used only in relation to a single acute ingestion.
Adapted from Smilkstein et al., Ann. Emerg.Med., 1991, 20, 1059
Those whose plasma paracetamol levels are above the “normal treatment line”, should continue N-acetylcysteine treatment with 100 mg/kg IV over 16 hours repeatedly until recovery. Patients with increased susceptibility to liver damage as identified above, should continue treatment if concentrations are above the “high risk treatment line”. Prothrombin index correlates best with survival. Monitor all patients with significant ingestions for at least 96 hours.
Ibuprofen
Symptoms
Symptoms include headache, nausea, vomiting, epigastric pain, gastrointestinal bleeding, rarely diarrhoea, disorientation, excitation, coma, drowsiness, dizziness, tinnitus, fainting, occasionally convulsions. In cases of significant poisoning acute renal failure and liver damage are possible.
In serious poisoning metabolic acidosis may occur and the prothrombin time/INR may be prolonged, probably due to interference with the actions of circulating clotting factors. Acute renal failure and liver damage may occur.
Prolonged use at higher than recommended doses may result in severe hypokalaemia and renal tubular acidosis. Symptoms may include reduced level of consciousness and generalised weakness (see section 4.4 and section 4.8).
Exacerbation of asthma is possible in asthmatics.
Therapeutic measure
Patients should be treated symptomatically as required. Within one hour of ingestion of a potentially toxic amount, activated charcoal should be considered. Alternatively, in adults, gastric lavage should be considered within one hour of ingestion of a potentially life-threatening overdose.
Good urine output should be ensured.
Renal and liver function should be closely monitored.
Patients should be observed for at least four hours after ingestion of potentially toxic amounts.
Frequent or prolonged convulsions should be treated with intravenous diazepam. Other measures may be indicated by the patient’s clinical condition.
Codeine
Symptoms
Codeine overdose may result in central nervous system and respiratory depression with hypoxia, hypotension, shock, gastric hypomotility with ileus, non-cardiogenic pulmonary oedema. Nausea and vomiting are prominent features. The opiate intoxication syndrome is described as a triad of depressed level of consciousness, miotic pupils, and decreased respirations.
Management
Treatment is based more on clinical presentation than on specific laboratory data, except when complications have occurred.
Plasma codeine levels are not clinically useful.
Support the respiratory and cardiovascular function.
Monitor arterial blood gases and/or pulse oximetry, pulmonary function tests, and chest x-ray in patients with significant exposure.
Ipecac-induced emesis is not recommended because of the potential for CNS depression and seizures.
Consider pre-hospital administration of activated charcoal as aqueous slurry in patients with a potentially toxic ingestion who are awake and able to protect their airway.
Activated charcoal is most effective when administered within one hour of ingestion.
Use a minimum of 240 ml of water per 30 g charcoal.
Optimum dose has not been established, but the usual dose is 25 to 100 g in adults and adolescents; 25 to 50 g in children aged 1 to 12 years (or 0,5 to 1 g/kg body weight); and 1 g/kg in infants up to 1 year old.
Consider naloxone as antidote in patients with decreased level of consciousness. The most frequently recommended initial naloxone dose for codeine overdose is 0,4 to 2 mg intravenous bolus in both children and adults.
This dose can also be given subcutaneously in the absence of intravenous access or intratracheally.
6.3. Shelf life
24 months.
6.4. Special precautions for storage
Keep in a dry place below 25°C. Protect from light.
6.5. Nature and contents of container
White opaque polypropylene securitainers with clip-on, low density or medium density or high-density polyethylene pilfer proof seals with 10, 30, 60, 100 or 500 capsules.
Clear PVC or Tristar blisters sealed with aluminium foil with 10, 30, 60, 100 or 500 capsules packed into a cardboard carton.
Sealed aluminium layflat patient ready bags with LDPE ribbed zipper with 30, 60 or 100 capsules.
Amber glass containers with black, hard plastic (polypropylene) screw caps with expanded LDPC inner seals with 30, 60 or 100 capsules.
6.6. Special precautions for disposal and other handling
No special requirements.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.